Dear Editor:
The kidney and the eye, with their characteristic vascular anatomy, are vulnerable to vasculitis syndromes like antineutrophil cytoplasmic antibodies (ANCA) associated small vessel vasculitis1-3.
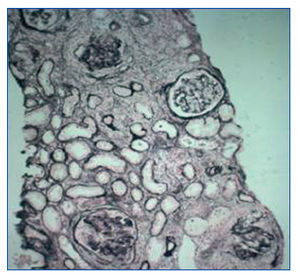
Here we present a case of a 44 year old male patient complained of asthenia for one month. Two weeks before he developed bilateral subconjunctival hemorrhage without photophobia or ocular pain. The patient denied epistaxis, hemoptysis, abdominal pain, arthralgias or myalgias. On examination he had subconjunctival bleeding due to bilateral difuse episcleritis (Figure 1). There were no cardiopulmonary auscultatory findings, no purpura and no signs of arthritis. The patient past medical history was remarkable for chronic sinusitis with frequent episodes of epistaxis. The blood panel showed severe azotemia (serum creatinine 11,2 mg/dl, BUN 100 mg/dl), normocytic normochromic anaemia (Hb 11,3 g/dl; Ht 33,3%), C-reactive protein 16,9 mg/L (0-10 mg/L), active urinary sediment (30 red blood cells per high-power field, 4 red blood cell casts), and a 24 hour proteinuria of 2,2 g. Renal imaging revealed normal size kidneys and normal corticomedular diferentiation. Hemodialysis was initiated due to uremic syndrome. Chest x-ray and chest CT scan did not show any evidence of active disease in the lower respiratory tract. Nasal sinus CT scan was compatible with a previous history of chronic sinusitis involving right etmoidal and both maxillary sinus. Nasal mucosa biopsy showed a non-specific inflammatory process. Serologic panel was negative for HIV1 and 2, HBV and HCV infection, complement fractions were within normal range. The immunological study was positive for circulating C-ANCA with anti-proteinase 3 (PR3) activity confirmed by enzimatic imunoassay (ELISA), and negative for anti-nuclear, anti DNAds and anti- glomerular basement membrane (anti-GBM) antibodies. The renal biopsy revealed a segmentar necrotizing glomerulonephritis with circumferential crescents in more than 80% of glomeruli (Figure 2). Immunofluorescence microscopy was compatible with a pauci-imune glomerulonephritis The above investigation confirmed the diagnosis of ANCA associated small vessel vasculitis and the patient initiated treatment with cyclophosphamide (100 mg id po), methylprednisolone (1 g id ev) changed to prednisolone (70 mg id po) after 3 days, and prophylactic antibiotherapy with trimethoprim/sulfamethoxazole. On hospital day four, he had a complete remission of the oftalmic disease, maintaining severe renal failure. Three months later, our patient remained on hemodialysis due to severe azotemia, without glomerular hematuria. Since renal function did not recover and there was no evidence of active extrarenal disease, immunesupressors were discontinued.
The authors present a case report of systemic vasculitis associated with ANCAs with specificity for anti-proteinase 3 (PR3), with renal, upper respiratory tract and eye involvement suggestive of Wegener granulomatosis.
The specificity of ANCA and its role on prognosis was shown by a retrospective study by Sven Weidner, involving 80 patients with confirmed pathological diagnosis of pauci-imune glomerulonephritis. In this study, patients with PR3 ANCAs had a higher risk of progressing to end-stage renal disease (ESRD)4.The patient in our case report, besides having PR3 ANCAs, also presented with a pre-treatment serum creatinine above 500 µmol/L (5,7 mg/dl), which also predicts a worse outcome4. As for the type and number of crescents, the presence of circumferencial crescents in more than 80% of glomeruli, determines a dismal prognosis, indicating a worse response to immunesupressor treatment5.
Our case report illustrates that an uncommon extra-renal involvement like an episcleritis, can be the form of presentation of a systemic disease with lethal potential. Although the prognosis in terms of progression for ESRD is mainly determined by the renal histology, the type of ANCA involved and serum creatinine value when treatment is begun, the patient survival is still dependent on the level of clinical suspicion leading to an early diagnosis and treatment.
Figure 1. Subconjunctival bleeding due to difuse episcleritis.
Figure 2. Cellular circumferential crescents in more than 80% of glomeruli (Silver stain, x100).