Dear Editor,
We present a case of septicaemia, endocarditis, meningitis and pneumonia caused by Staphylococcus aureus in a patient on haemodialysis whose arteriovenous fistula (AVF) became infected with this organism. These include, a description of a case infrequently found in the medical literature.
Woman of 45 years of age, allergic to tetracyclines, with a personal history of active smoking, poorly controlled hypertension (HT), mixed cryoglobulinaemia undergoing steroid treatment and on haemodialysis due to chronic kidney disease due to nephroangiosclerosis.
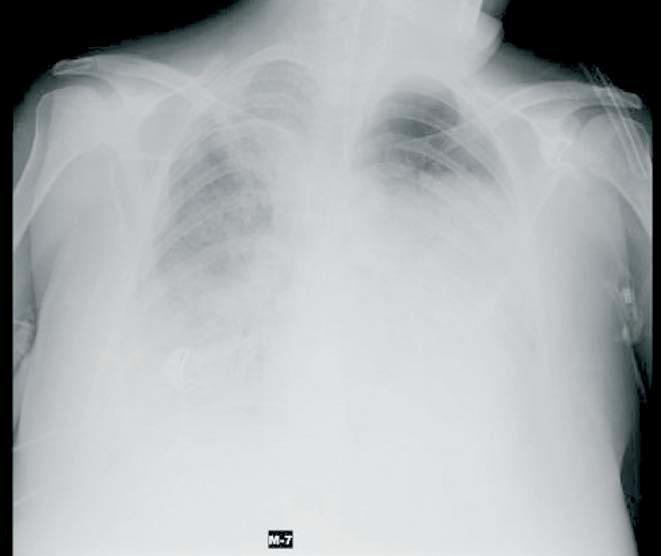
The patient entered the Intensive Medicine Department with suspected meningitis, after having a fever for 5 days and decrease of consciousness. On initial clinical examination the following were found: neurologically, GSC 8 (M4, O2, V2), nuchal rigidity, no alterations of cranial nerves; on heart auscultation: a mitral squeaking systolic murmur (not found on previous admittances); on lung auscultation: there was right basal hypoventilation and signs of infection of the AVF in the right upper limb. Based on the patient's neurological study orotracheal intubation was performed and mechanical ventilation started. On chest X-ray an image of bilateral alveolar condensation was seen (Figure 1). A cranial CT was performed and showed a left occipital hypodense lesion, without ventricular system dilatation. Lumbar puncture was performed and the results were compatible with acute bacterial meningitis; simultaneously blood and bronchoaspirate cultures were performed. Empirical antibiotic treatment was begun. Subsequently, Methicillin sensitive S. areus (MSSA) was isolated from all samples.
As AVF infection was suspected it was closed (subsequently MSSA was also isolated from this site). Forty-eight hours after admittance, in view of the patient's haemodynamic deterioration and suspected endocarditis, a transoesophageal echocardiogram was performed and large vegetations were seen on the septal and posterior flap of the mitral valve with images indicating the presence of a fistulised abscess.
The patient's evolution was poor; she suffered septic shock and multi-organ failure and died 9 days after admittance to our unit.
Patients on haemodialysis are at greater risk for bacterial infections than the rest of the population, and vascular catheters are the point of entry of these infections due to their frequent manipulation, added to the uraemia’s immunosuppression condition.1 The most common germs that may cause bacteraemia in this type of patient are S. aureus, followed by gram negative aerobic bacilli and polymicrobial flora.1,2
When an S. aureus infection appears the main point of entry is usually the vascular access. Clinically, and especially in patients on haemodialysis, this can cause meningitis, endocarditis, bacteraemia, osteomyelitis, sepsis, etc. In our case, the patient was diagnosed with meningitis, bacteraemia, endocarditis and pneumonia.
Endocarditis is one of the most severe complications of bacteraemia, due to its high mortality rate (close to 30%). The mitral valve is the most affected (about 50%), followed by the aortic valve (30%) and, lastly, the right chambers (25%).1,3,4 In cases of endocarditis with valve obstruction this must be replaced surgically, as soon as the patient’s condition allows.5
Broad spectrum antibiotic treatment must be begun and vascular access must be dismantled, since it is frequently the source of infection. In spite of all this, infection due to S. aureus usually has a high rate of morbidity/mortality,2 with a mortality of 25-47% according to the series, which increases to 47-65% at one year when the patient is in haemodialysis.1,5 Hospital mortality at 60 days, independent of the microorganism responsible, is around 47-52%1,5.
Figure 1. Chest X-ray in which it is possible to see an alveolar-bilateral image of condensation