Antecedentes y objetivos: A pesar de los beneficios del tratamiento insulínico intensivo, la nefropatía continúa siendo un problema importante en la diabetes mellitus tipo 1 (DM1). Dada la escasez de datos en nuestro medio, hemos realizado un estudio observacional con el objetivo de analizar la prevalencia de albuminuria y sus estadios en una serie pacientes con DM1 y evaluar los factores relacionados. Pacientes y métodos: Estudio transversal que incluyó a todos los pacientes mayores de 18 años con un tiempo de evolución de la DM1 superior a 6 meses, que fueron atendidos de manera consecutiva durante el año 2008 en el Hospital del Mar de Barcelona y el Hospital de Granollers. Resultados: De los 291 pacientes analizados, 46 (20,2 %) presentaban microalbuminuria o proteinuria. Los pacientes albuminúricos presentaron, en comparación con aquellos sin enfermedad renal, mayor edad (42,0 ± 12,3 años vs. 37,1 ± 11,5 años), tiempo de evolución de la diabetes (22,5 ± 11,5 años vs. 14,1 ± 10,1 años), índice de masa corporal (26,3 ± 3,7 kg/m2 vs. 25,2 ± 3,4 kg/m2), hemoglobina glucosilada (8,15 ± 1,5 % vs. 7,59 ± 1,4 %) y de presión arterial sistólica (139,7 ± 21,7 mmHg vs. 122,2 ± 20,3 mmHg). El análisis multivariado mostró una asociación independiente de la presencia de albuminuria con la duración de la diabetes (odds ratio [OR] 1,081; intervalo de confianza [IC] del 95 % 1,038-1,126), la trigliceridemia (OR 1,011; IC del 95 %: 1,002-1,018), el tabaquismo (OR 3,279; IC del 95 %: 1,114-9,654) y la hipertensión arterial (OR 3,495; IC del 95 %: 1,074-11,368). Conclusión: En la presente serie, uno de cada cinco pacientes con DM1 tenía microalbuminuria o proteinuria, y su presencia se relacionó con el tiempo de evolución de la diabetes, la trigliceridemia, el tabaquismo y la hipertensión arterial.
Background and objectives: Despite the beneficial effects of intensive insulin therapy, nephropathy continues to be a major concern in type 1 diabetes mellitus (DM). Given the scarce data on this subject in our population, we performed an observational study in order to analyse the prevalence of albuminuria and its stages in a series of patients with type 1 DM and to evaluate the related factors. Patients and methods: Cross-sectional study that included all patients aged 18 and over, diagnosed of type 1 DM for at least 6 months, consecutively attended during 2008 at the Hospital del Mar de Barcelona and Hospital Granollers. Results: 291 patients were analysed and 46 (20.2%) had micro- or macroalbuminuria. Albuminuric patients, compared to those without were older (42.0±12.3 years vs. 37.1±11.5 years), had longer duration of diabetes (22.5±11.5 years vs. 14.1±10.1 years), and higher body mass index (26.3±3.7kg/m2 vs. 25.2±3.4kg/m2), glycosylated haemoglobin (8.15±1.5% vs. 7.59±1.4%) and systolic blood pressure (139.7±21.7 mmHg vs. 122.2±20.3mmHg). Multivariate analysis showed an independent association of albuminuria with diabetes duration (OR 1.081, 95% CI 1.038-1.126), triglyceride levels (OR 1.011, 95% CI: 1.002-1.018), smoking habit (OR 3.279, CI 95%: 1.114-9.654) and hypertension (OR 3.495, 95% CI: 1.074-11.368). Conclusion: In our series, one out of five patients with type 1 DM had micro- or macroalbuminuria, and its presence is associated with diabetes duration, triglyceride concentration, smoking and hypertension.
INTRODUCTION
For many years, the leading cause of death in patients with type 1 diabetes mellitus (DM1) has been diabetic nephropathy or one of its direct consequences1. From 1993, with the publication of the results of the Diabetes Control and Complications Trial (DCCT), which demonstrated a 50% decrease in the incidence of nephropathy when insulin treatment is stepped up, there has been a positive change in this trend.2 In contrast, cardiovascular disease the is main factor responsible for the increase in mortality in this particular population.3
However, and despite the improvements gained after the generalisation of intensive insulin therapy, the prevalence of microalbuminuria and proteinuria remains high. In this respect, US studies indicate a prevalence of nephropathy in DM1 of 22% after 14 years of treatment.4 In our field, the data - though scarce - show a prevalence of microalbuminuria of 10% at 10 years5 and 25% at 20 years after diagnosis.6 In addition, a direct relationship has been observed between nephropathy with macroangiopathy and metabolic syndrome, and it has been demonstrated that its presence is a predictor of mortality in this group of patients.7
The main risk factors for the development of nephropathy in DM1 are age, duration of diabetes, poor glycaemic control and blood pressure, along with an unfavourable lipid profile.8-11 Other factors described are smoking, ponderal status and the presence of insulin resistance or metabolic syndrome.12 In the latter case, there has been a mention of a direct relationship between the number of components of metabolic syndrome and the risk of developing nephropathy.13 For these reasons, we have analysed the prevavlence of albuminuria and its stages in a series of DM1 patients and evaluated the possible related factors.
PATIENTS AND METHODS
Patients
A cross-sectional study was carried out with DM1 patients treated consecutively at the Endocrinology Outpatients Clinic of the Hospital del Mar of Barcelona and the Hospital de Granollers between January and December 2008. DM1 was considered autoimmune when, in addition to the diagnostic criteria of diabetes, there was positivity for anti-GAD/65Ks antibodies or anti-IA2 at the time of debut, and a free C-peptide concentration of less than 1.1ng/ml 6 minutes after the administration of 1mg of intravenous glucagon. The study protocol, with approval from the centre's Ethics Committtee, included a physical examination and a blood sample. All participants were over 18 years of age and had suffered diabetes for over 6 months.
Each patient's age and sex, were recorded, along with the time elapsed since being diagnosed with DM1, history of serious cardiovascular episodes (myocardial infarction, coronary revascularization surgery, angioplasty, seizures, transient ischaemic attack, and peripheral vascular disease, defined as the presence of intermittent claudication or amputation), as well as the presence of chronic microangiopathic complications of diabetes (microalbuminuria or proteinuria, retinopathy, peripheral or autonomic neuropathy). The presence of complications was assessed by an expert diabetologist (JJC, IC) except for retinopathy, which was evaluated by an ophthalmologist after conducting an in-depth examination of the eye under pharmacological mydriasis. The study followed the criteria of the American Diabetes Association for clinical diagnosis of complications14 and insulin requirements were calculated in units by kilogram of weight and by day (IU · kg-1 · d-1). The physical examination included measurement of weight, height and abdominal circumference, as well as blood pressure using standard techniques. Arterial hypertension was classified as the presence of blood pressure figures exceeding 130/80mmHg, confirmed by two separate measurements over two weeks, or the need to undergo hypotensive treatment.
Diagnosis of neuropathy was based on clinical findings such as paraesthesia, anaesthesia or other positive symptoms in the lower limbs. The Semmes-Weinstein monofilament test on the first toe pulp and the first and fifth metatarsals of both feet was also used, labelling as neuropathy a lack of response in 1 or more of the 6 points explored.
Albuminuria was classified in stages according to urinary excretion of albumin (UEA): 1) normal albumin levels (UEA <30mg/24 h); 2) microalbuminuria (UEA 30-300mg/24h), and 3) proteinuria (UEA >300mg/24 h).
Metabolic syndrome was diagnosed in accordance with the modified criteria of the National Cholesterol Education Program Adult Treatment Panel III (NCEP-ATP III).14
Measurement
Patients included in the study had blood samples taken after a 12-hour fasting period. Measurements were made of the concentration of total cholesterol and triglycerides using enzymatic methods in an automatic analyser - Cobas Mira® (Baxter Diagnostics AG, Düdingen, Switzerland) - and high-density lipoprotein cholesterol by means of separation by precipitation with phosphotungstic acid and magnesium chloride. Blood glucose was measured by the oxidase method. Glycated haemoglobin was quantified using chromatography (Biosystem, Barcelona, Spain), and UEA by means of nephelometry (inter-assay variation coefficient 2.0%).
The sensitivity of the insulin was assessed using the estimated glucose disposal rate (eGDR), calculated according to the following formula:
24.31 – 12.22 (Cint/Cad) – 3.29 (HTA) – 0.57 (HbA1c)
where Cint/Cad is the coefficient between waist and hip circumference, HTA represents the history of arterial hypertension defined as blood pressure higher than 140/90mmHg or in antihypertensive treatment (0=no, 1=yes) and HbA1c the value of glycated haemoglobin as a percentage. It should be noted that higher TeDG values indicate greater sensitivity to insulin, while lower values indicate greater resistance.
Statistical analysis
The Student's t-test was used for the comparison of means and the χ-test2 for analysing the categorical variables, along with the Mann-Whitney U test for those variables not following normal distribution and the Pearson correlation coefficient to establish relationships between quantitative variables. In order to evaluate factors related to the presence of albuminuria (dependent variable), a multiple logistic regression model was employed, which included as independent variables those showing a P value of <0.05 in the univariate analysis. The statistics software SPSS version 12.0 for Windows was used to analyse the results.
RESULTS
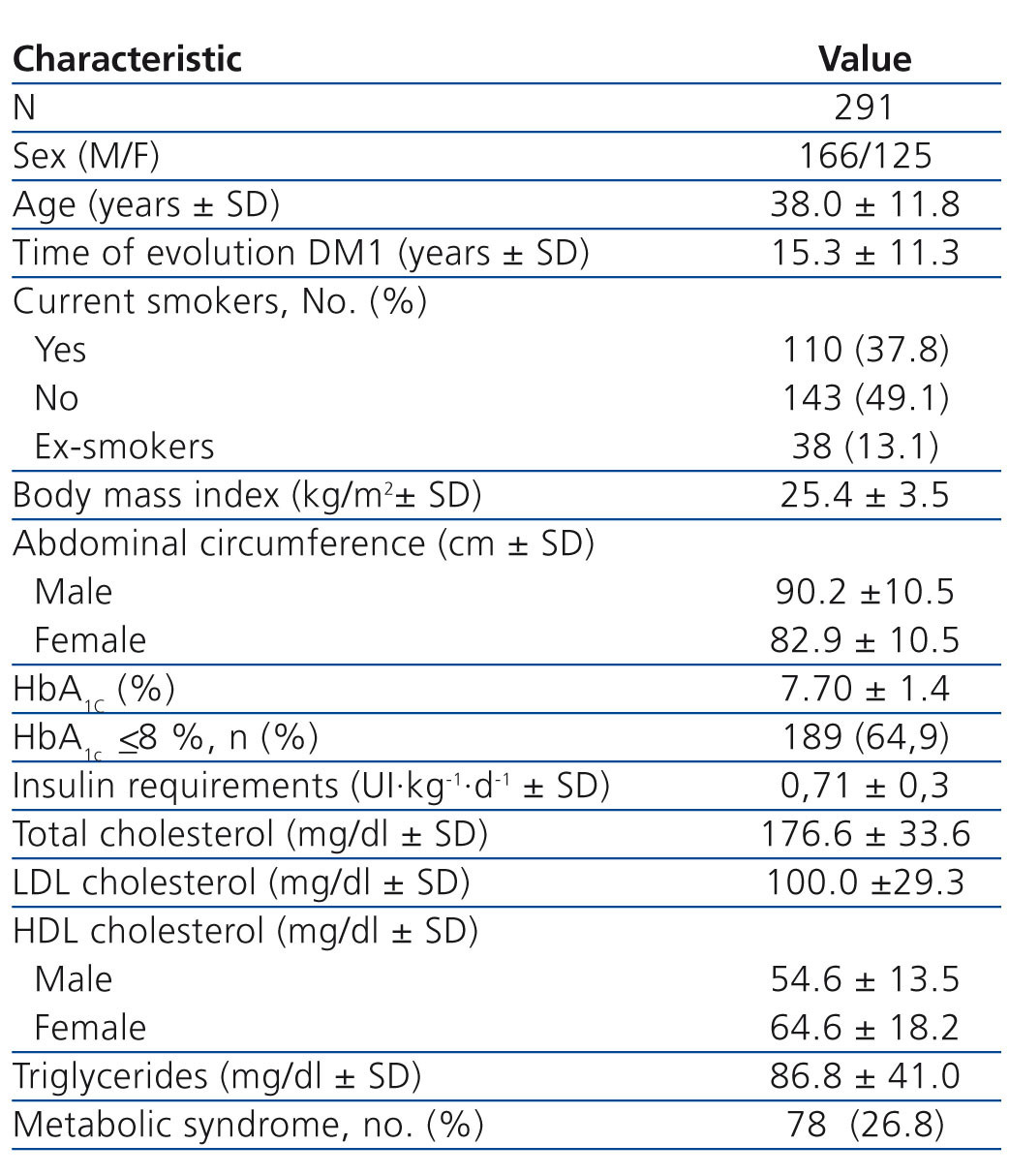
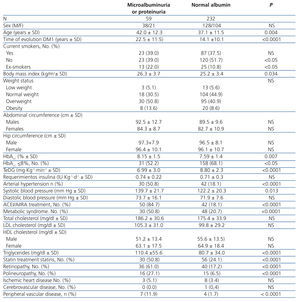
The study included 291 patients assessed consecutively during 2008; their principal characteristics are shown in Table 1. Forty-six patients (15.8%; confidence interval [CI] 95%: 5,3-26.4%) had microalbuminuria, and 13 (4.4%; CI 95%: 0-15.7%) proteinuria, meaning a total prevalence of 20.2% (CI 95%: 10.0-30.5%). With regard to the remaining chronic complications of DM1, the prevalence of retinopathy was 26.1% (CI 95%: 16,2-36,0%), peripheral polyneuropathy 10.7% (CI 95%: 0-21.6%), ischaemic heart disease 3.8% (CI 95%: 0-15.1%), cerebrovascular disease 0.3% (CI 95%: 0-11.0%), and peripheral vascular disease 3.8% (CI 95%: 0-15.1%).
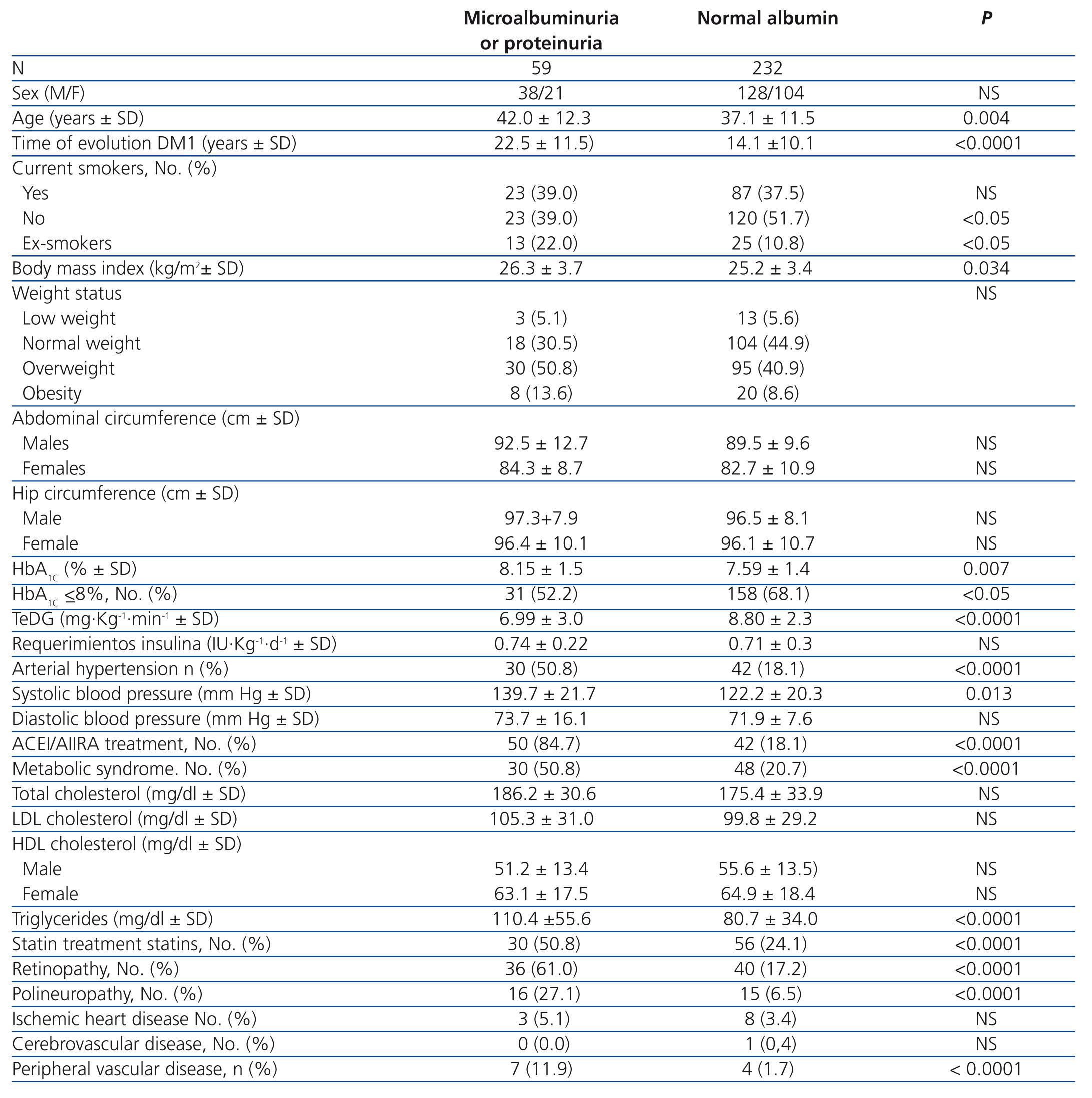
Patients with microalbuminuria or proteinuria were older, had longer diabetes duration and their body mass index was greater; also, their glycaemic control and blood pressure were worse than those with normal albumin levels (Table 2). It is notable that only 40% of albuminuric patients had blood pressure levels of lower than 130/80mmHg. Furthermore,they had greater resistance to insulin assessed by TeDG and a greater concentration of triglycerides, although lower than 150mg/dl, the level considered to be the objective in this group of patients.
In addition, the presence of albuminuria was associated with retinopathy, polyneuropathy and peripheral vascular disease. No relation was observed with ischemic heart disease or seizures, probably due to the low number of cases in these latter two categories.
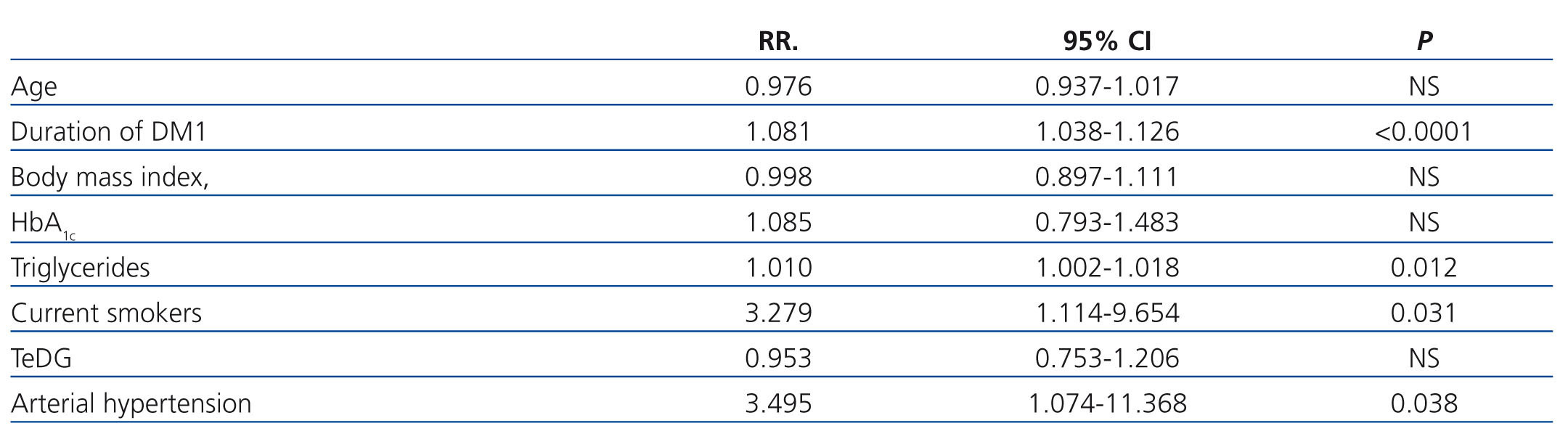
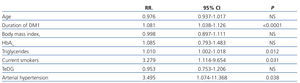
The logistic regression analysis (Table 3) revealed that the variable associated with the presence of albuminuria with greatest statistical power was diabetes duration. Also, it confirmed smoking and hypertension as risk factors. The rise in triglyceride concentration, even at levels considered within normal limits, had negative repercussions on the prevalence of albuminuria. Thus, for every mg/dl of increase in triglycerides, there was an increase of 1% in the probability of pathological urinary excretion of albumin.
DISCUSSION
This study on patients suffering from DM1 with an average duration of 15 years has demonstrated that albuminuria is present in one out of five cases. The cases included in the analysis were diagnosed with DM1 following the publication of the DCCT2 for which they were treated with a course of intensive insulin from the time of their diagnosis. It that cohort, the prevalence of micro and macroalbuminuriain the intensive insulin treatment group after monitoring for an average of 22 years was 22.6%, which agrees with the data obtained in this study. However, the results from the arm initially receiving conventional treatment, although this was subsequently stepped up, showed a greater prevalence (29.9%) confirming the benefits of metabolic optimisation in this group of patients in relation to the incidence of microangiopathy.9 Thus, the univariate analysis revealed poorer metabolic control in those patients with DM1 and albuminuria, with an average concentration of glycated haemoglobin of 8.15%, not excessively far from the objectives currently established.15 In this group, more than half of all patients had levels of HbA1c ≤8 %. It is probably for this reason that, after adjusting other factors in the logistic regression study, this variable lost significance.
With respect to the impact of time on the prevalence of albuminuria, the present study showed that, despite the fact that both the patient's age and the duration of DM1 showed a significant relation in the univariate analysis, this relation with was only maintained with duration in the multivariate, findings similar - once again - to those of the cohort in the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC). However, it should be noted that in said study, the duration of DM1 was similar in all the sections made, since the inclusion of patients was done as the diagnosis of DM1 was made, over a relatively short period of time.4
With regard to weight, patients with albuminuria had a higher body mass index in the univariate analysis which did not continue to have statistical significance in the multivariate. Nor were any differences observed in terms of weight status, although the prevalence of overweight and obesity in these patients is worrying. Thus, 64.4% of patients with albuminuria and 49.5% of those with normal albumin levels had a body mass index of over 25kg/m2. These findings, together with the marked difference in sensitivity to insulin, quantified through eGDR, and an elevated percentage of patients with metabolic syndrome, all factors associated with the presence of microangiopathic complications,12 suggest that the clinical phenotype of DM1 patients is increasingly similar to those with type 2 diabetes. In addition, there is scientific evidence indicating that in our field the prevalence and features of nephropathy in DM1 are at the present time similar to those described for type 2.16,17
Other relevant data from the study were those concerning control of blood pressure. More than half of the albuminuric patients suffered from arterial hypertension and all of them were taking taking specific drug treatments. Despite this, however, systolic blood pressure levels were close to 140mmHg, and was clearly higher than the 130mmHg recommended in this clinical situation.15 Although it is unlikely that arterial hypertension was a consequence of the presence of nephropathy in view of the characteristics of the patients, the design of the study makes it impossible to exclude that possibility completely. It is, therefore, necessary to persist with all those strategies aimed at convincing patients to adopt lifestyles that are as heart-healthy as possible. Likewise, therapeutic inertia must be avoided and the care team should be made aware of the importance of managing blood pressure in these patients, as less than half of them have optimal levels according to existing clinical practice guidelines.
Lastly, it is known that high triglyceride levels are the most frequent lipid alteration in DM1 patients with poor metabolic control and/or nephropathy.18 It should be emphasised that in the current study, triglyceride studies are normal, which is attributable in part to satisfactory metabolic control, with average HbA1c levels close to those desired. Furthermore, the concentration of triglycerides in patients with microalbuminuria or proteinuria was 110mg/dl, similar to that referred to in the context of the DCCT study,4 and clearly lower than the 150mg/dl recommended by clinical practice guidelines.15 Even so, these concentrations were higher than those of the group without kidney disease and the multivariate analysis showed that, for each mg/dl rise in triglycerides, the risk of albuminuria increased 1%.
The limitations of this study lie in its cross-sectional design, so we should not forget the possible temporal variability of the parameters evaluated, nor that the findings described represent associations only and do not imply causality. With respect to the diagnosis of chronic complications, retinopathy and polyneuropathy were registered as dichotomous variables, without quantifying their status by means of scales or other methods. Also, some of the patients included had had DM1 for less than 5 years, during which the prevalence of microangiopathy is very low, a fact that may undervalue their percentages. Lastly, no data were recorded concerning physical activity or sociocultural levels, which may have influenced the results.
In conclusion, one in five patients with DM1 of an average duration of 15 years developed albuminuria and its presences was related to the duration of the disease, high triglyceride levels, smoking and arterial hypertension.
Conflict of Interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. Demographic, anthropometric and clinical characteristics of 291 patients with type 1 diabetes
Table 2. Association of age, sex and clinical features of type 1 diabetes with the presence or absence of albuminuria.
Table 3. Risk ratio and confidence intervals for the presence of albuminuria for the variables selected in the logistic regression analysis