To the Editor,
Peritoneal infections are a serious complication in peritoneal dialysis and can affect the clinical state of the patient and technique viability.1 Gram positive bacteria are most frequently involved (coagulase negative Staphylococcus [40%-60%], Staphylococcus aureus [10%-20%] and Streptococcus [10%-20%]). Of all peritonitis, 5%-20% are due to gram negative organisms. Other germs, which represent less than 5% of cases, are other bacteria, fungi and protozoa.1
There are not many cases of Listeria monocytogenes peritonitis published in the literature, and they generally affect immunocompromised patients.2-12
We present the case of a patient undergoing peritoneal dialysis due to heart failure resistant to diuretics. This is the first case of Listeria monocytogenes infection in the peritoneum in our hospital.
We present a 64-year-old man who underwent an operation for tetralogy of Fallot when he was younger. He later developed a severe right heart failure and eventually became resistant to diuretics. This caused him to be admitted to hospital on several occasions for anasarca and acute renal failure. He was rejected for a heart transplant because he had severe pulmonary hypertension. Given this situation, he was entered onto a peritoneal ultrafiltration programme (May 2006), having a single night exchange of 2l of icodextrin.
The patient arrived at the emergency department with abdominal pain, moderate diarrhoea and cloudy peritoneal drainage fluid. He did not complain of fever, vomiting or focal neurological or infectious signs. He had no family history of food borne diseases and he was not aware of having made any mistakes with the dialysis technique, which would have caused the equipment to become unsterile. This patient had already suffered two other peritonitis, with negative peritoneal fluid culture. He was treated successfully with wide spectrum antibiotics (vancomycin and ceftazidime), recovering without any major problems.
When he was admitted, signs of distension and pain were noted upon abdominal palpation. Analytical tests showed: leukocyte count: 8900/µl, 84% neutrophils, haemoglobin: 12.1g/dl; platelets: 163 000/µl; urea: 60mg/dl, creatinine: 1.7mg/dl; normal hepatic enzymes; peritoneal leukocytes count: 8800/µl, 96% neutrophils. The Gram staining of the peritoneal fluid revealed single and short-chain bacilli. Empirical intraperitoneal antibiotic treatment was started with vancomycin and ceftazidime. Small, translucent, grey colonies with a discreet beta haemolysis area were found in the peritoneal fluid on blood agar plate cultures following aerobic incubation at 37ºC (pH 7.2-7.4), indicating Listeria monocytogenes. Faecal samples were cultivated. They were negative for Listeria, although it was provided after antibiotic treatment had been started which could have halted its growth. Initial antibiotics were substituted for intravenous ampicillin and intraperitoneal gentamicin. The infection started responding to the antibiotics after 72 hours. Specific antibiotic therapy was maintained for three weeks.
Listeria monocytogenes is the only Listeria among the seven known species that can infect human beings. It is an aerobic gram positive germ (in certain circumstances can also behave like an anaerobic one) which cannot form spores. Despite being present in the environment, it does not usually cause humans to become ill. An incidence of 0.7 cases/100 000 has been calculated.13 The elderly, newborns, cancer patients, cirrhotic and immunocompromised patients are more susceptible to contracting a Listeria infection. The most common clinical signs include meningitis, endocarditis, gastroenteritis, miscarriage and bacteraemia. Peritonitis caused by Listeria is a rare, dangerous form of the complication. Spontaneous forms of peritonitis caused by Listeria are well known, especially in cirrhosis patients.13 Around 50 cases have been published and most of them describe Spanish patients.14 The geographical predilection in Spain is not entirely understood, but may be due to eating habits including the consumption of incorrectly pasteurised dairy products or raw fruit and vegetables.14
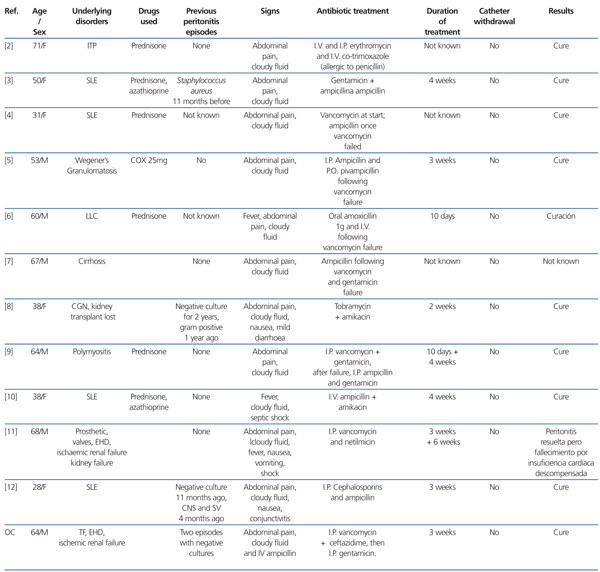
For patients undergoing dialysis, peritonitis caused by Listeria is very rare. Table 1 shows the cases published to date in the medical literature. All cases have occurred in immunocompromised patients, due to illness or medication.
It has been reported that natural killer cells (non-antigen first line of defence) in heart failure patients are in a situation of anergy and respond less to the molecules that usually stimulate them, such as interleukin-2 and interferon-gamma. These patients are therefore considered to be at greater risk of developing infections given their immunocompromised sitution.15
Listeria is one of the most virulent pathogens which cause food borne diseases. It has a mortality rate of 20%-30%, higher than almost all other food borne illnesses. It was difficult to find the source of infection in our patient, but given that he lives in a rural area it is possible that he ingested incorrectly pasteurised dairy products, which would have caused this germ to colonise the intestine. The bacteria would have then invaded the mucosa, reaching the peritoneum. Unfortunately, this has not been confirmed, given that the faecal culture sample was provided after antibiotic treatment had been started. However, the hypothesis mentioned above seems the most plausible.12 Furthermore, chronic heart failure could have been involved in this process. In this situation, the patient would have intestinal oedema, increased permeability and would be more susceptible to bacterial invasion.16
The antibiotic treatment of choice for Listeria infection is penicillin or ampicillin, which can be administered in combination with aminoglycosides or not.12 However, there is no clear indications as to which treatment is better for peritonitis caused by Listeria, or how long treatment should last. Vancomycin may not be effective since Listeria is an intracellular microorganism.5,6,9 Both trimethoprim-sulfamethoxazole and erythromycin have been used successfully for patients allergic to penicillin.2,12 For most cases, peritonitis responds rapidly and effectively to antibiotics, without needing to withdraw the peritoneal catheter.
In summary, we must remember that Listeria monocytogenes is a germ that can cause peritonitis in patients undergoing peritoneal dialysis, where rod-shaped gram positive bacteria can be found, even in patients considered immunocompetent. Above all, prevention is the best weapon to combat this zoonosis.
Table 1. Characteristics of 11 cases of peritonitis caused by Listeria monocytogenes in patients undergoing peritoneal dialysis