We aimed to assess the effectiveness of ambulatory blood pressure monitoring (ABPM) and subclinical target organ damage parameters for diagnosis of resistant hypertension (RH).
MethodsWe assessed demographic and anthropometric variables, the incidence of cardiovascular events and subclinical target organ damage (n=112). We also studied the relationship between these variables and the ABPM results.
ResultsOf the 112 patients referred from primary care with a diagnosis of RH, 69 (61.6%) were confirmed by ABPM. We found statistically significant differences (p<0.001) between patients with RH and pseudo-resistant hypertension in the appearance of subclinical target organ damage. A percentage of 84 of the patients had microalbuminuria: 66.25±30.7mg/dl); 44.9% had stage 3 chronic kidney disease: the average glomerular filtration was 59ml/min/1.73m2; and 56.5% had left ventricular hypertrophy on echocardiography. Fundoscopy revealed that 64% of the patients had hypertensive retinopathy. Three variables were associated with an increased HR risk: microalbuminuria, hypertensive retinopathy and left ventricular hypertrophy (OR 5.7, 6.2 and 11.2, respectively).
ConclusionsThis study shows that the systematic testing for target organ damage, particularly in terms of albuminuria, is a simple and inexpensive tool, with a high predictive value for RH (85%), which could be useful for prioritizing patients who need ABPM.
El presente estudio tiene como objetivo destacar la importancia de la monitorización ambulatoria de la presión arterial (MAPA) y de los parámetros de lesión subclínica de órgano diana en el diagnóstico de hipertensión refractaria (HR).
MétodosSe estudiaron pacientes con diagnóstico de HR (n=112). Se analizaron variables demográficas, antropométricas, riesgo cardiovascular y lesión subclínica de órgano diana y se relacionaron con la confirmación de HR a través de la MAPA.
ResultadosDel total de 112 pacientes con el diagnóstico de HR derivados desde atención primaria se confirmaron mediante MAPA el 61,6% de los casos (n=69). Se observaron diferencias estadísticamente significativas (p<0,001) en la aparición de lesión subclínica de órgano diana en los hipertensos refractarios respecto a los pseudorrefractarios. Un 84% de los pacientes con HR presentaban microalbuminuria: 66,25±30,7mg/dl). El 44,9% tienen una enfermedad renal crónica estadio 3 con filtrado glomerular medio de 59ml/min/1,73m2. El 56,5% presentaba hallazgos ecocardiográficos de hipertrofia de ventrículo izquierdo. El examen de fondo de ojo reveló que un 64% de los pacientes presentaban retinopatía hipertensiva. Las 3 variables que se asociaron a mayor riesgo de HR fueron la presencia de microalbuminuria, retinopatía hipertensiva e hipertrofia de ventrículo izquierdo por ecocardiograma (OR 5,7, 6,2 y 11,2, respectivamente).
ConclusionesNuestro estudio demuestra que la búsqueda sistemática de daño de órgano diana, especialmente en lo referente a albuminuria, es una herramienta sencilla y barata, con un valor predictivo de HR alto (85%). Podría ser de utilidad en circunstancias en las que es necesario priorizar la realización de MAPA.
Hypertension (HTN) is considered the main cardiovascular risk factor. Refractory hypertension, from now on RHTN, is defined as the failure to achieve the target blood pressure (PA≤140/90mmHg or PA≤130/80mmHg in the case diabetics or patients with chronic kidney disease) despite the use of full doses of 3 or more antihypertensive drugs, one of them being a diuretic.1,2
It is estimated that approximately 13% of treated hypertensive patients have RHTN.3,4 The exact percentage is difficult to estimate because a high number of patients with RHTN present pseudo refractory HTN, that is, they are patients with an incorrect diagnosis of RHTN due to inadequate medical treatment, non-adherence to treatment or non-accurate measurement of blood pressure in the clinic visit.5
There are two fundamental basis for the good treatment and control of blood pressure: the modification of the habits of life and the adequate use of antihypertensive drugs3; the main objective of the treatment of HTN is to achieve optimal cardiovascular protection of the patient.
In recent decades, it has been shown that high variability of BP is associated with the development, progression and severity of organic damage and, therefore, with an increased risk of mortality.6 For this reason, the determination of BP, as well as the evaluation of its fluctuations, are studied by different methods, such as the ambulatory BP monitoring of 24h (ABPM) or the self-measurement of BP which is increasingly used in our cclinics.
Hence, these methods of BP measurement are fundamental for the diagnosis of RHTN vs. pseudo-refractory hypertension, helping to discern between fluctuations and the appearance of subclinical organic damage.7
In primary prevention, the stratification of cardiovascular risk refers to the use of both demographic data (age, sex, family history of cardiovascular disease) and cardiovascular risk factors (diabetes, dyslipidemia, obesity, etc.). Therefore, in the diagnosis of hypertension, the search for subclinical target organ injury is recommended both in patients with RHTN and in those with pseudo-refractory HTN. The detection of this subclinical organ damage is a powerful predictor of future cardiovascular events independent of the systematic evaluation of vascular risk (score), and adds an additional risk according to the clinical guidelines of the ESH/ESC.8,9 The physician who treats patients with hypertension refers patients to specialized clinics to perform an ABPM and make the diagnosis of RHTN. One can ask if these patients with RHTN have demonstrable organ damage that could help to the diagnosis of RHTN. Certainly, in clinical practice, it would be very helpful to have parameters that allow to distinguish between RHTN and pseudo-refractory HTN, and always considering that ABPM is necessary to reach the diagnosis with certainty.
The present study aims to highlight the value of ABPM and the parameters indicating subclinical target organ injury in the diagnosis of RHTN.
MethodsThis is a cross-sectional, prospective cohort study conducted in consecutive patients referred from primary care to the Nephrology outpatient clinic during the years 2016–2017 with the diagnosis of RHTN.
The true RHTN was defined as ABPM in 24h≥140/90mmHg despite treatment with full doses of 3 antihypertensive drugs including a diuretic, after excluding non-adherence to treatment and secondary causes of hypertension.
Patients included were more than 18 years old without previous history of cardiovascular disease. Exclusion criteria were chronic kidney disease stage 4 or more, nephrotic range proteinuria, diabetes mellitus or a clear manifestation of cardiovascular disease (cerebrovascular disease, coronary artery disease, heart failure, symptomatic peripheral arterial disease or hospital admission due to cardiovascular disease).
The demographic and clinical variables recorded included age and gender, the year of diagnosis of hypertension and the history of smoking. In the anthropometric variables, data such as weight and height were recorded and the body mass index (kg/m2) was calculated.
The BP was measured in 3 different manners: measurement of BP in the outpatient clinic considering the average of 3 determinations; self-measurement of the BP at home, estimated as BP provided by the patient; and through 2 ABPM: one at baseline and another after the treatment modifications.
A systematic search for target organ injury was performed, including a blood test to calculate glomerular filtration through the MDRD-4 formula. An urinalysis was also performed to measure of microalbuminuria from a single isolated morning sample. For cardiac assessment, a 12-lead electrocardiogram and an echocardiogram were performed to study left ventricular hypertrophy (LVH). For the assessment of peripheral arterial disease, the ankle-brachial index and eye fundi were used for the screening of hypertensive retinopathy.
The use of antihypertensive medications before and after ABPM were recorded as well as the changes made after performing ABPM.
As far as the statistical analysis, Student's t test or Chi-square were used to compare groups depending on whether they were continuous variables. Logistic regression was used to identify risk factors for RHTN. In addition, the area under the curve, sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were calculated to assess the prediction capacity of the model.
From the logistic regression data, models were developed to calculate the predictive value of RHTN diagnosis using variables representing organic damage. These calculations are based on previous publications.10 To know the predictive value of the variables as a whole, the following formula is applied: LN (odds)=β0+βiXi+β2X2...+βkXk.
The statistical analysis was performed using the SPSS program version 22.0 for Windows.
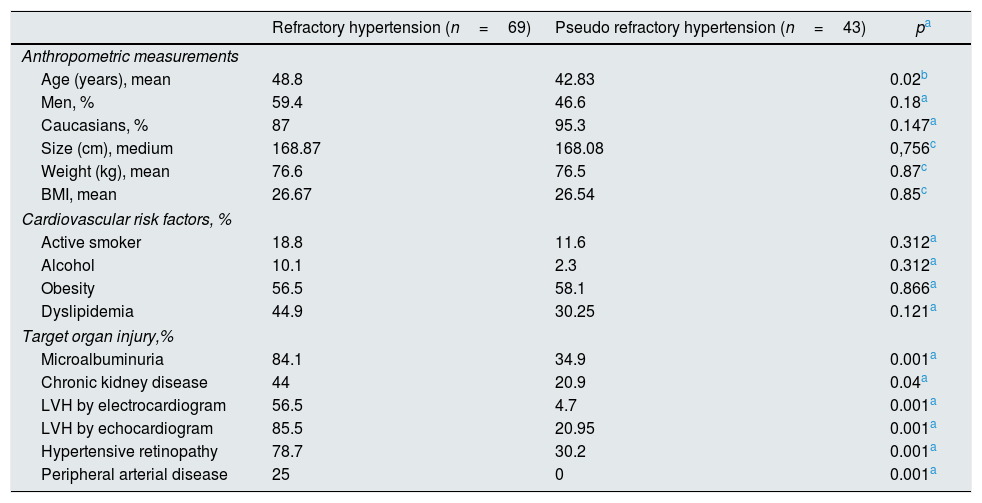
ResultsThere were 112 patients referred from primary care with the probable diagnosis of RHTN, the diagnosis was confirmed by ABPM in only 61.6% (n=69). Therefore, the final cohort included a total of 69 patients with RHTN. The median age of the cohort was 48.8±13.34 years, 59.4% were males, 87% were Caucasian and 13% were black. The anthropometric characteristics of the studied population were: average weight 76.6±10.52kg, average height 168.87±7.49cm, average body mass index 26.67±3, 95kg/m2) (Table 1).
Baseline characteristics of the groups with refractory hypertension and pseudo refractory hypertension.
| Refractory hypertension (n=69) | Pseudo refractory hypertension (n=43) | pa | |
|---|---|---|---|
| Anthropometric measurements | |||
| Age (years), mean | 48.8 | 42.83 | 0.02b |
| Men, % | 59.4 | 46.6 | 0.18a |
| Caucasians, % | 87 | 95.3 | 0.147a |
| Size (cm), medium | 168.87 | 168.08 | 0,756c |
| Weight (kg), mean | 76.6 | 76.5 | 0.87c |
| BMI, mean | 26.67 | 26.54 | 0.85c |
| Cardiovascular risk factors, % | |||
| Active smoker | 18.8 | 11.6 | 0.312a |
| Alcohol | 10.1 | 2.3 | 0.312a |
| Obesity | 56.5 | 58.1 | 0.866a |
| Dyslipidemia | 44.9 | 30.25 | 0.121a |
| Target organ injury,% | |||
| Microalbuminuria | 84.1 | 34.9 | 0.001a |
| Chronic kidney disease | 44 | 20.9 | 0.04a |
| LVH by electrocardiogram | 56.5 | 4.7 | 0.001a |
| LVH by echocardiogram | 85.5 | 20.95 | 0.001a |
| Hypertensive retinopathy | 78.7 | 30.2 | 0.001a |
| Peripheral arterial disease | 25 | 0 | 0.001a |
An 18.8% were active smokers and 11.6% ex-smokers; Obesity was present in 56.5%, altered basal glycaemia in 15.9% and dyslipidemia in 44.9% (Table 1).
In the analysis of the variables related to the measurement of BP, the average heart rate was 75.58 lpm, the average SBP of 154.16mmHg and an average DBP of 93.1. The self-measurement of the BP showed a heart rate of 73.78lpm, the average SBP was 151.12mmHg and an average DBP of 90.39mmHg. And with ABPM, the heart rate was 73.04lpm, average SBP 150.0mmHg and a mean DBP of 88.67mmHg. The circadian pattern of BP was analyzed through ABPM showing that 78.3% had a dipper pattern, 13% non-dipper and 8.7% riser.
Regarding the occurrence of target organ injury, statistically significant differences were observed (p<0.001) in refractory hypertensive patients compared to pseudo refractory HTN. RHTN was associated with subclinical lesion of target organ; 84% presented microalbuminuria: 66.25±30.7mg/dl. A 44.9% had stage 3 chronic kidney disease with an average glomerular filtration rate of 59.6ml/min/1.73m2. A 56.5% presented echocardiographic findings of LVH. The eye fundi examination revealed that 64% of the patients had hypertensive retinopathy. A 24.6% had a pathological ankle-brachial index (Table 1), despite not presenting clinical signs of peripheral arterial disease (Table 1).
In relation to hypotensive drugs, it should be mentioned that 100% of patients with RHTN were on diuretics, 73.9% on calcium antagonists, 53.6% on ACEI, 50.7% on ARA-II, 40.6% on alpha blockers, 39.1% on beta-blockers and 18.8% on sympatholytics.
A 46.3% were on antihypertensive treatment combining 3 drugs, followed by 43.5% with 4 drugs and 10.1% with 5 drugs.
After performing the ABPM and readjusting the treatment, modifications were evaluated in both the BP and the circadian pattern and the number of drugs, obtaining a reduction in BP of 8.6 and 5.7mmHg in SBP and PAD in 24h, respectively, in the true refractory HTN, and of 6.2 and 4.1mmHg in the SBP and the DBP in 24h in the pseudo refractory HTN (p<0.001). A change in the circadian pattern to dipper pattern was achieved in 97% of the refractory patients and in 100% of the pseudo refractory patients. The change in medical treatment was also statistically significant (p<0.001), with a decrease of 0.93 drugs in patients with RHTN and 0.47 drugs in pseudo refractory HTN.
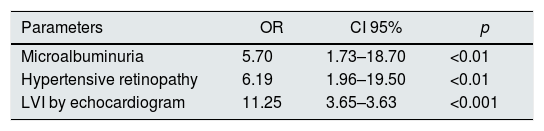
Target organ damage and diagnosis of refractory hypertensionThe binary logistic regression analysis of patients with RHTN adjusted by type of lesion of the target organ is included in Table 2. The initial variables included in the model were: age, sex, body mass index, abdominal perimeter, degree of obesity, dyslipidemia, smoking habit, microalbuminuria, MDRD-4, hypertensive retinopathy and LVH by echocardiography. The 3 variables that were associated with a higher risk of RHTN were the presence of microalbuminuria, hypertensive retinopathy and LVH by echocardiogram (OR 5.7, 6.2 and 11.2, respectively).
Binary logistic regression analysis of risk factors of refractory hypertension.
| Parameters | OR | CI 95% | p |
|---|---|---|---|
| Microalbuminuria | 5.70 | 1.73–18.70 | <0.01 |
| Hypertensive retinopathy | 6.19 | 1.96–19.50 | <0.01 |
| LVI by echocardiogram | 11.25 | 3.65–3.63 | <0.001 |
Variables introduced in the model: age, sex, body mass index, abdominal perimeter, degree of obesity, dyslipidemia, smoking, microalbuminuria, MDRD-4, hypertensive retinopathy, left ventricular hypertrophy by echocardiogram.
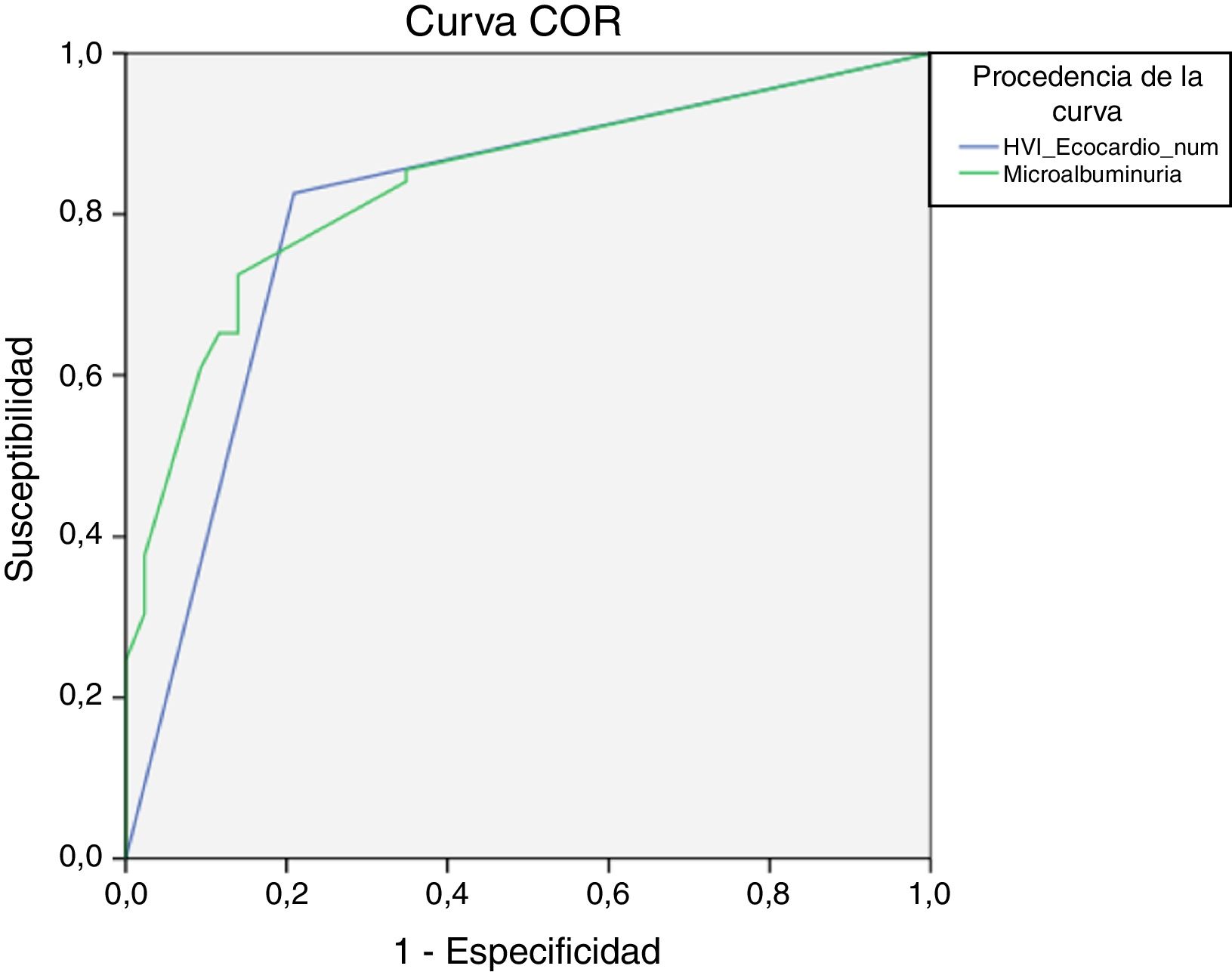
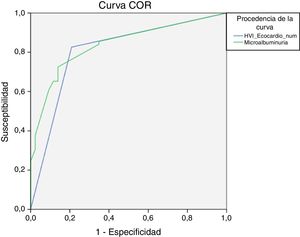
With these results, the ability to predict the association between the variables included in the multivariate analysis was calculated using ROC curves. The presence of microalbuminuria showed the best area under the curve of all the variables included in the model (0.83, 95% IC 0.76–0.91, p<0.001), followed by the presence of LVH with an area under the curve of 0.80 (95% IC 0.72–0.89, p<0.001) (Fig. 1).
The sensitivity, which expresses the percentage of patients correctly identified by the model, and the specificity, which assesses the ability of the model to identify those who are not at risk of developing RHTN, were 79.4% and 71.7% for microalbuminuria and 86.3 and 73.9% for LVH, respectively. The PPV of microalbuminuria was 84.4% and the NPV was 65.1%. The PPV and the NPV of the presence of LVH were 82.6 and 79%, respectively.
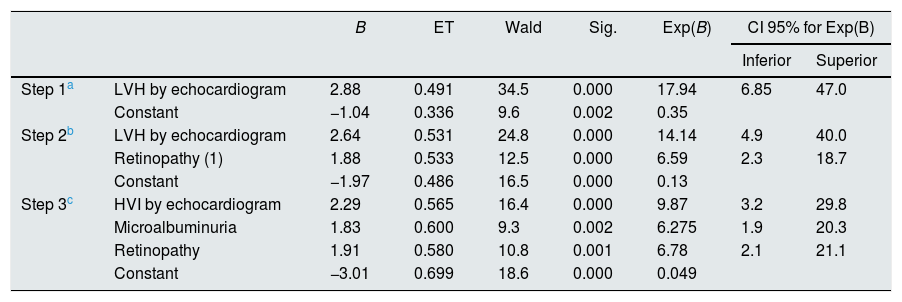
Table 3 shows the data obtained from the logistic regression, which are used to calculate the predictive value of the variables as a whole: LVH, microalbuminuria and retinopathy. The values of B, Exp (B) and the constant are used to calculate the predictive value of RHTN using the formula: LN (odds)=β0+βiXi+β2X2+...+βkXk. The model predicts a risk of 95% of experiencing RHTN if the patient presents simultaneously with microalbuminuria, LVH and retinopathy.
Logistic regression analysis to calculate the predictive value considering the three variable together: left ventricular hypertrophy, microalbuminuria and retinopathy.
| B | ET | Wald | Sig. | Exp(B) | CI 95% for Exp(B) | |||
|---|---|---|---|---|---|---|---|---|
| Inferior | Superior | |||||||
| Step 1a | LVH by echocardiogram | 2.88 | 0.491 | 34.5 | 0.000 | 17.94 | 6.85 | 47.0 |
| Constant | −1.04 | 0.336 | 9.6 | 0.002 | 0.35 | |||
| Step 2b | LVH by echocardiogram | 2.64 | 0.531 | 24.8 | 0.000 | 14.14 | 4.9 | 40.0 |
| Retinopathy (1) | 1.88 | 0.533 | 12.5 | 0.000 | 6.59 | 2.3 | 18.7 | |
| Constant | −1.97 | 0.486 | 16.5 | 0.000 | 0.13 | |||
| Step 3c | HVI by echocardiogram | 2.29 | 0.565 | 16.4 | 0.000 | 9.87 | 3.2 | 29.8 |
| Microalbuminuria | 1.83 | 0.600 | 9.3 | 0.002 | 6.275 | 1.9 | 20.3 | |
| Retinopathy | 1.91 | 0.580 | 10.8 | 0.001 | 6.78 | 2.1 | 21.1 | |
| Constant | −3.01 | 0.699 | 18.6 | 0.000 | 0.049 | |||
Within the large population of subjects with hypertension it is estimated that approximately 15% fail to achieve adequate control of BP despite the use of at least 3 antihypertensive drugs. These patients are called patients with hypertensive refractory to treatment, representing one of the most important clinical challenges in the management of hypertension.11,12 This group of subjects with RHTN is characterized by a long history of hypertension, obesity, dyslipidemia and target organ involvement that could be affecting the kidney (microalbuminuria), heart (LVH) or retina (hypertensive retinopathy), among others.
In the last decade, ABPM has been added to the diagnostic and therapeutic maneuvers aiming to guarantee treatment adherence and optimization, and the evaluation of secondary HTN. Thanks to the ABPM, the truly RHTN patients are identified and separated from pseudo refractory hypertension group which are 30% of the patients with the potential diagnosis of RHTN which as is the case in our study only 68% of the patients had RHTN confirmed with ABPM.13
Therefore, ABPM is a useful tool for the diagnosis, treatment, follow-up and prognosis of patients with RHTN. Performing ABPM allows a correct classification in the 4 established subgroups of hypertensive patients (true resistant hypertension, white coat resistant hypertension, controlled resistant hypertension and masked resistant hypertension) with a greater characterization of the subject, with its clinical nuances and a better adjustment of the treatment of the HTA, which is translated in a reduction of the secondary effects, a greater adherence to the treatment and a less economic cost.
The use of ABPM has allowed us to know the prognostic value of nocturnal hypertension, as described in the study by Muxfeldt and Salles,7 which determines nocturnal BP as the most reliable prognostic factor in RHTN and as shown in the present study it highlights the high prevalence of patients with circadian non-dipper pattern both with RHTN and pseudo refractory HTN. This information allows to intensify chronotherapy and adjust medication at night, as described in the study by Hermida et al.12
The general objective of antihypertensive treatment in patients with resistant hypertension is to maintain daytime and nighttime control of BP. The present study shows that refractory hypertensive patients are older than pseudo refractory patients, with higher prevalence of men and a greater cardiovascular involvement (obesity, altered basal glycaemia, dyslipidemia), coinciding with the observations by Brown et al.15
Regarding the target organ injury, it was found that 87% of the cohort had at least the involvement of one target organ, the most prevalent was microalbuminuria, a finding that coincides with that described in other studies, Armario16; in addition, the glomerular filtration rate of patients with RHTN is lower than that of patients with pseudo refractory HTN.14 In RHTN the prevalence of cardiac involvement measured as LVH,17 was 61%, similar to that of other publications14 and higher than in non-refractory hypertensive patients. Hypertensive retinopathy occurred in 79.7%, which coincides with what is being described in the literature.11 Peripheral arterial disease, measured as pathological ankle-brachial index was present in 27.8% of patients, although during the anamnesis, no patient reported symptoms indicative of this disease; peripheral arterial disease is probably secondary to atherosclerosis caused mainly by hypertension and smoking habit.18
It should be remembered the importance of changes in lifestyle directed to avoid obesity, excess of high salt and alcohol intake and encourage physical exercise. The patient must be aware of the importance of changes in lifestyle which should be verified in the clinic visits. Then, to achieve adequate control of BP in patients with RHTN, it is necessary to use at least 3 hypotensive drugs as indicated by the guidelines of the European Society of Hypertension.15
Within the pharmacological groups, the use of diuretics stands out and the most used are thiazides and aldosterone antagonists. It has been confirmed that 90% of patients are treated with the classic triad (diuretic, ACEI or ARA-II and calcium antagonists). In 43.5% of patients in whom this treatment is not sufficient, the fourth most used medication has been alpha-blockers, followed by beta-blockers and, finally, sympatholytic.
In cases where ABPM is not easy to perform, there is the possibility of analyzing parameters of organic damage to predict the presence of RHTN vs Pseudo refractory HTN. The detection of target organ damage, given its PPV as described in the results, can be a tool that helps to prioritize, rather than substitute, the determination of ABPM. The PPV for RHTN of the presence of microalbuminuria was 84.4% and the NPV was 65.1%. The PPV and the NPV of the presence of LVH were 82.6 and 79%, respectively. Therefore, the probability of certainty in the diagnosis of RHTN is approximately 85% using parameters such as microalbuminuria or LVH. If 3 parameters are present in the same patient - microalbuminuria, LVH and retinopathy - the predictive value of RHTN using the 3 variables as a whole is 95%.
However, ABPM is necessary to establish the so-called chronotherapy, that is, to identify the most adequate time for administration of the drug during the day to optimize the effectiveness of treatment. Thanks to these modifications it has been achieved a change in the circadian pattern to a dipper pattern, a reduction in BP and avoid an increase in the number of drugs or even reduce the medication in patients with either RHTN or pseudo refractory HTN.
ConclusionOur study shows after performing ABPM, 4 out of 10 patients diagnosed with RHTN do not really have such a diagnosis. So we consider ABPM the recommended reference standard for the diagnosis of true RHTN and, in addition, it allows us to readjust medical treatment in each patient. The systematic search for target organ damage is recommended, especially albuminuria which is simple and inexpensive, with a high predictive value for RHTN (85%). Considering microalbuminuria, LVH and retinopathy together, the predictive value of RHTN is 95% and could be useful in those circumstances in which it is necessary to prioritize patients in whom ABPM should be performed.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Poveda García MI, del Pino y Pino MD, Alarcón Rodriguez R, Rodelo-Haad C, Parrón Carreño T. El valor de la MAPA y de los parámetros de lesión subclínica de órgano diana en el diagnóstico de hipertensión refractaria. Nefrologia. 2019;39:67–72.