In December 2019, several cases were detected in Wuhan of pneumonia related to a novel coronavirus,1,2 called SARS-CoV-2.3 Since then, the virus has spread as a pandemic. The disease it produces is officially known as COVID-19.3 The Sociedad Española de Nefrología (SEN) [Spanish Society of Nephrology] has published an action protocol with the objective of limiting the spread of the virus.4 To adapt to such recommendations, the Haemodialysis Unit at the Hospital Universitario de la Ribera [Ribera University Hospital] decided to modify its way of operating and organisational structure. So, in order to eliminate unnecessary steps in the management of patient flow, it was decided to consider the principles of lean manufacturing5 adapted to health care.6,7 This philosophy involves the creation of an information system for the status of tasks, so that orders are responded to when required and to the extent necessary, thus offering the best product quality in the shortest time and cost possible. In addition, it is based on a smooth but continuous workload – which allows for a reduction of stress – and on a constant flow of information that enables immediate responses.
Based on the principles of lean manufacturing, “not infected” and “no contact” were defined from the patient's perspective as a product or value. The next step was to identify unessential processes within a system in crisis, with limited resources and information exchange. To do this, the exclusivity of tasks within the flow chart was eliminated and an information centralisation system was developed with the following structure:
- -
Document 1 (Excel® document).
- •
Sheet 1: Identification of suspected cases, confirmed cases and their contacts. List of pending and performed tasks related to the taking of samples and their results.
- •
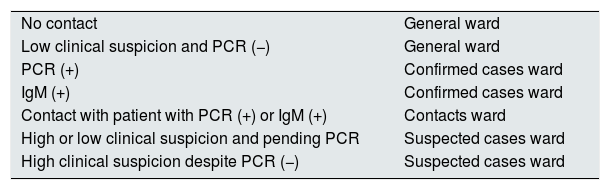
Sheet 2: Map of wards and beds. Visualisation of the available beds represented by boxes that, organised in tables, provided a general image of the different haemodialysis wards and shifts. Each box included the name of the patient occupying the bed, with relevant notes if applicable. A table included in said sheet reminded the user of the distribution of the wards according to the results of PCR or serology for SARS-CoV-2 (Table 1).
Table 1.Distribution of patients according to PCR or serology result for SARS-CoV-2.
No contact General ward Low clinical suspicion and PCR (−) General ward PCR (+) Confirmed cases ward IgM (+) Confirmed cases ward Contact with patient with PCR (+) or IgM (+) Contacts ward High or low clinical suspicion and pending PCR Suspected cases ward High clinical suspicion despite PCR (−) Suspected cases ward
- •
- -
Document 2 (Word® document). List of identified patients, classified as "low" or "high" suspicion according to clinical, laboratory and radiological criteria.8–10
This system accompanied a contingency plan by which human healthcare resources were reorganised in order to minimise their loss. Thus, there were only two doctors in the Haemodialysis Unit at the same time, one of them on a 14 h shift and the other on a 24 h shift.
If the infection of a patient by SARS-CoV-2 was likely, dialysis was ordered in the area of suspected patients, the data were recorded on sheet 1 of the Excel® document, and the individual transfer of the patient and possible contacts was ordered. On sheet 2 the bed map was modified. The Word® document collated the clinical, laboratory and radiological criteria by which the classification into high or low suspicion had been decided. The flow of patients in relation to the wards varied according to the results of the tests. At the end of the afternoon shift, the layout of the bed map was sent to the Ambulance Station.
All documents could be consulted through a VPN connection, which allowed any physician to verify or modify the proposed strategy. The nursing or auxiliary personnel present in the dialysis ward had continuous access to the information, which made it possible to avoid errors in the classification of patients.
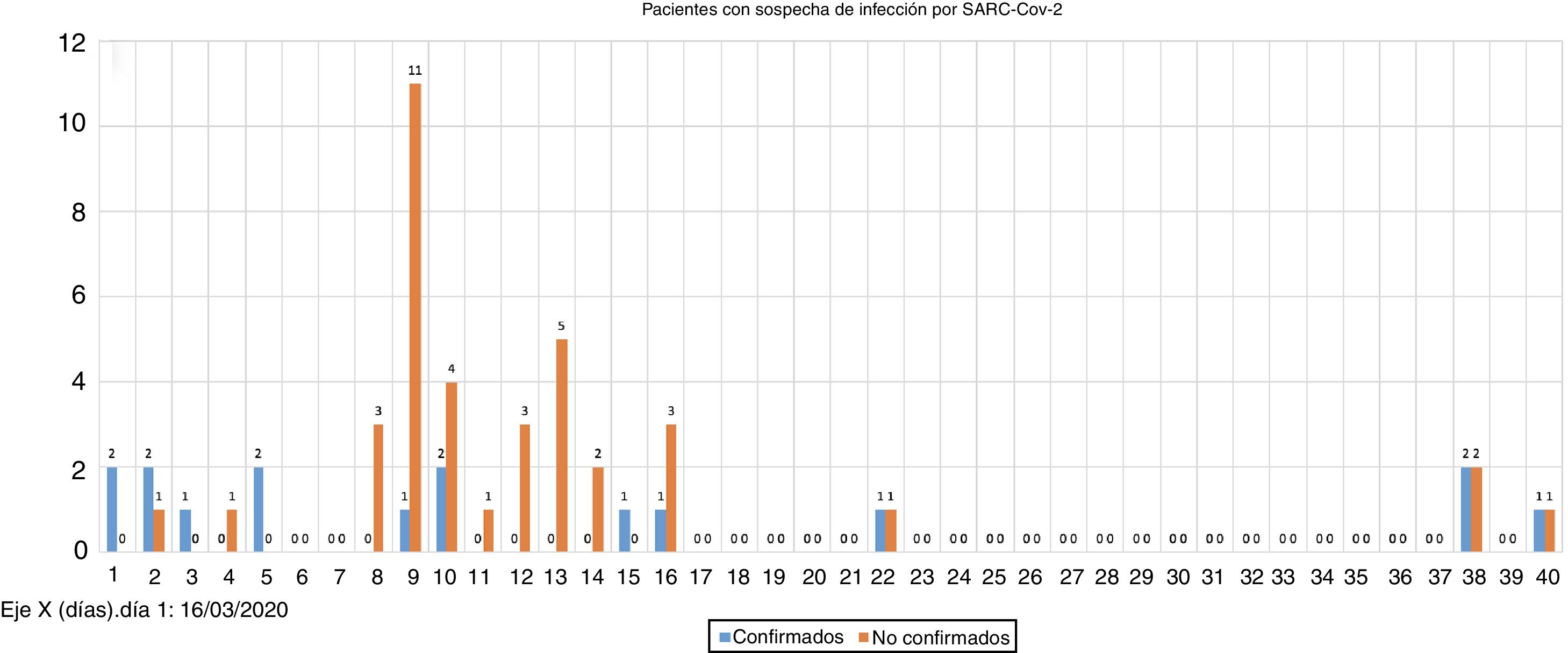
As of 17 May, 2020, 16 cases positive for SARS-CoV-2 were counted (8.2% of all patients, 29.6% of all evaluated patients) (Fig. 1). Three of the positive patients (18.75% of cases) had negative initial results despite high clinical suspicion. Of these, two cases presented with bilateral pneumonia.
Thirteen of the positive patients (81.25 %) were usually transferred in a collective ambulance. Twenty-eight patients were identified as contacts during the transfer, but an association was only observed between one patient and two of their four contacts, who were detected as positive at 35 days by screening, both being asymptomatic.
The number of healthcare personnel on sick leave reached 23.6%. Of the total of 72 workers, three nephrology specialists, 10 university nursing graduates and four nursing assistants were infected.
In short, the work system was simple and dynamic, allowing real-time consultations, offering a general picture of the situation and avoiding classification errors. With all this, and despite the number of healthcare personnel on sick leave, the management of the Unit was kept uniform and the spread of the virus among patients was limited.
Please cite this article as: Ribés Cruz JJ, Bea Reyes E, Graña Fandos J, Blanco Mateos Y, Aparicio Aliaga M, Aznar Artiles Y, et al. Crisis por COVID-19: aplicando los principios de la manufactura esbelta dentro de una Unidad de Hemodiálisis. Nefrologia. 2021;41:474–475.