La presencia de malnutrición es bien conocida en la enfermedad renal crónica (ERC). El descubrimiento en los últimos 15 años de los mecanismos fisiopatológicos que desencadenan este proceso, tales como la anorexia, el aumento del catabolismo proteico y la inflamación, ha generado la necesidad de una nueva denominación por la Sociedad Renal Internacional de Nutrición y Metabolismo (ISRNM): protein energy wasting syndrome (PEW). Los objetivos de este documento son proponer la utilización del término «desgaste proteico energético» (DPE) como una traducción más fiel del término anglosajón y actualizar los mecanismos patogénicos implicados que son inherentes al DPE. Simultáneamente revisamos las últimas evidencias epidemiológicas que ponen de manifiesto la relevancia de la malnutrición y su impacto tanto en la mortalidad como en la morbilidad en la ERC. Por último, destacamos la necesidad de redefinir los criterios diagnósticos del DPE para que sean aplicables a la población española con ERC. Los criterios establecidos por la ISRNM creemos que no son extrapolables a diferentes poblaciones, como ocurre por ejemplo con las diferencias antropométricas interraciales.
The presence of malnutrition in chronic kidney disease (CKD) is well-known. The discovery in the last 15 years of pathophysiological mechanisms that lead to this process, such as anorexia, the increase of protein catabolism and inflammation, has created the need for a new name by the International Society of Renal Nutrition and Metabolism (ISRNM): protein-energy wasting syndrome (PEW). This document’s objectives are to propose the use of the term “desgaste proteico energético” (DPE) as a more accurate translation of the English term and to update the pathogenic mechanisms involved that are inherent to DPE (PEW). We simultaneously review the latest epidemiological evidence that highlight the relevance of malnutrition and its impact both on mortality and morbidity in CKD. Finally, we point out the need to redefine DPE (PEW) diagnostic criteria so that they are applicable to the Spanish population with CKD. We do not think that the criteria established by the ISRNM can be extrapolated to different populations, as is the case, for example, with interracial anthropometric differences.
Chronic renal failure is characterised by nutritional disorders and systemic inflammation, which is accompanied by an increased catabolism, increasing morbidity and mortality. Nutritional disorders have been reported in the literature with numerous and confusing terms such as malnutrition, sarcopenia, cachexia and the malnutrition-inflammation-atherosclerosis syndrome. These terms describe a part of the problem but do not cover the many mechanisms that influence patient health and prognosis. In 2008, the International Society of Renal Nutrition and Metabolism (ISRNM) proposed that the term protein-energy wasting (PEW) be adopted as a unifying nomenclature and the starting point for a better knowledge and treatment of these problems in uraemic patients. The term PEW does not translate easily to Spanish and the Nutrition Working Group of the Spanish Society of Nephrology (S.E.N.) proposes to use the term “desgaste proteico energético” (DPE) as the most accurate translation of the English term.
The PEW syndrome is very common in kidney patients and it causes a deterioration in their quality of life and decreases short-term survival. However, regrettably, many hospitals still do not incorporate measures to evaluate and monitor the nutritional state of patients. Likewise, adequate nutrition is a strategy that is sometimes forgotten in the management of kidney patients.
We can define the PEW syndrome as a single pathological condition in which purely nutritional disorders converge with catabolic conditions. Both are pathophysiologically related, they are enhanced by each other and they create a vicious circle, which makes it difficult to distinguish between the two components in clinical practice. A diagnostic and therapeutic approach in patients with PEW must be multifactorial and we must try to treat each and every factor that we can identify, since nutritional repletion is insufficient as the only treatment, as it does not slow down underlying proteolysis. With the intention of providing a current view of all catabolic disorders covered by the PEW syndrome, we reported the main concepts, mechanisms and implications of this state.
CONCEPT AND TERMINOLOGY
PEW1 is defined as a pathological state where there is a continuous decrease or wasting of both protein deposits and energy reserves, including a loss of fat and muscle. Before introducing this new concept into our terminology, we should briefly consider the malnutrition-undernourishment concept and its difference with other terms such as the wasting syndrome, in order to understand the unifying nature of the term PEW.
The term “malnutrition” covers pathological states caused both by an excess and a deficiency of nutrients. However in uraemia, it is generally used to refer to undernourishment, i.e., the disorders derived from the deficiency of macro- and micronutrients2.
By “undernourishment”, we mean a body composition disorder characterised by an excess of extracellular water, frequently associated with a decrease in muscle and fat tissue, hypoproteinaemia and potassium deficiency, which interferes with the normal response of the patient to their disease and treatment. “Protein-calorie undernourishment” is caused whenever daily needs are not covered by the diet. It is often reversed with the recovery of intake and the resolution of the underlying problem. Protein-calorie undernourishment can be divided into three main clinical syndromes:
The defining feature of undernourishment is weight loss. Survival during fasting is related to the already existing fat storage volume. Changes in body composition are reflected as a severe increase in extravascular water, a decrease in fat deposits and a decrease in lean body mass. It is important to highlight that weight may increase during a severe acute disease, due to fluids passing into the third space. Abnormalities in uraemia in a certain manner reflect mixed malnourishment, although it presents with a moderate intensity and is not the result of an intercurrent acute condition, but rather, a low-intensity chronic inflammation.
The term “cachexia” represents a complex metabolic syndrome associated with a chronic disease and it is characterised by a gradual loss of muscle tissue, accompanied or not by concomitant losses of fat reserves. Cachexia, however, represents an extreme degree of intake that is rarely observed in advanced chronic kidney disease (CKD).
The term “wasting” was proposed by the World Health Organization in 19883 and is defined as an involuntary loss of weight of more than 10% on the baseline value in the absence of an opportunistic infection, a tumour disease or chronic diarrhoea. It is a multifactorial syndrome and it is occasionally difficult to know the main cause. It is characterised by a disproportionate loss of lean mass due to specific abnormalities in metabolism as part of the body’s defence mechanism in response to a stress situation. When this situation is sustained, it leads to a depletion of proteins, especially musculoskeletal proteins, and is not recovered with intake, since this whole process is due to cellular metabolic changes.
It is very important to adopt common terminology is Spanish and we believe that the concept of DPE agreed on by the S.E.N. Nutrition Group accurately captures the spirit of the ISRNM’s nomenclature PEW. This term describes the mechanisms involved and consequently allows us to identify therapeutic targets, use the appropriate monitoring methods and choose the most effective therapeutic approach. We recognise that the term “wasting” is less clinically severe than “emaciation”, which may occur in patients with chronic kidney disease. However, in the choice of terms and acronyms, we must consider the advantage, using simpler language, of instilling in healthcare professionals the need to identify and treat these catabolic disorders. The terminology DPE avoids including terms such as malnutrition of catabolism, with the aim of not giving more importance to any one of the components. In these disorders, both undernourishment and muscle catabolism converge and are pathophysiologically related, and as such, it is impossible to distinguish one from the other in clinical practice. Therefore, DPE implies both accelerated protein (muscle) and energy (fat) loss.
MECHANISMS INVOLVED IN PROTEIN-ENERGY WASTING
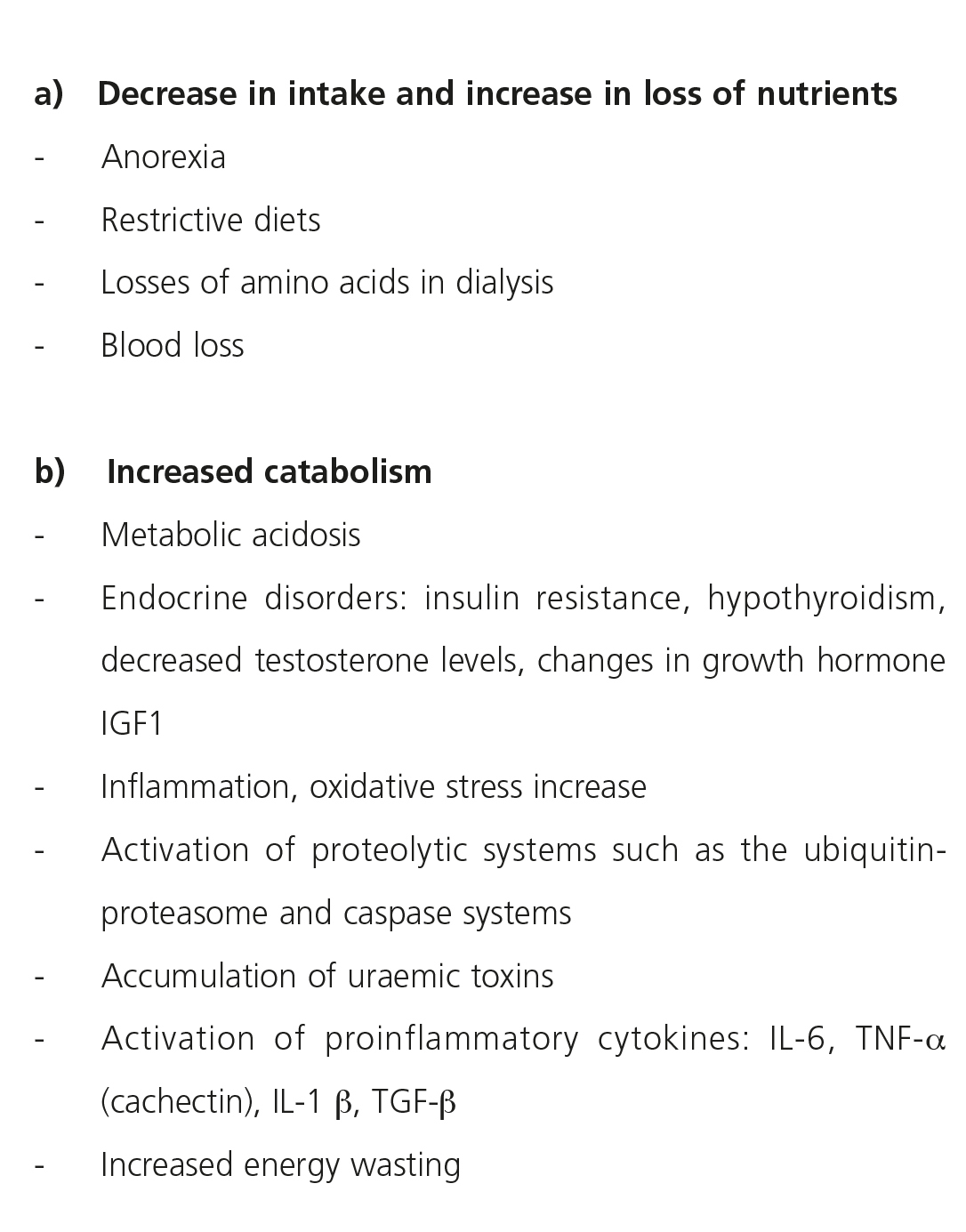
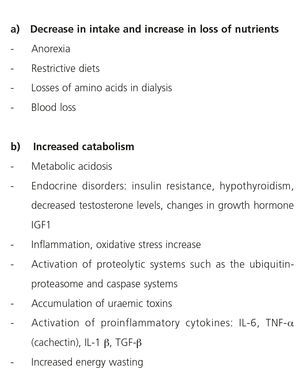
The disorders involved in renal failure malnutrition have recently been revised by the ISRNM4. Anorexia5 and the increase in protein catabolism6 result in an energy imbalance, with the final result of an increase in energy wasting7 and in the intake of energy storage sources.
Other pathophysiological mechanisms in CKD PEW are metabolic acidosis8, endocrine disorders9,10, inflammation11,12 and the activation of the ubiquitin-proteasome systems (UPS)13,14. At the same time, other aspects such as a restrictive diet, the loss of amino acids and micro-macronutrients15 due to dialysis techniques, blood loss, volume overload16 and other psychosocial factors change the energy balance.
Muscle mass loss (wasting)
The term sarcopenia defines a situation of major loss of muscle mass and strength and a multifactorial aetiology, where an intake deficiency may occur, as well as hormonal disorders, neuropathic damage, metabolic disorders and the presence of uraemic toxins17. It is a type of chronic muscular atrophy and in CKD, it is associated with PEW, limiting the independence of the patient and their quality of life. It compromises vital organs, with respiratory, musculoskeletal and heart muscle deterioration18. Decreased intake, metabolic acidosis, physical inactivity, diabetes and sepsis are associated factors in CKD that increase muscle proteolysis through increased catabolism, activation of different intracellular signals of muscle cell apoptosis and decreased synthesis. Several studies have shown significant atrophy of muscle fibres in CKD19-21 (Table 1).
One of the main mechanisms by which PEW is associated with muscle atrophy in uraemia is increased UPS-mediated protein catabolism and the activation of musculoskeletal myostatin. The UPS system degrades muscle proteins and myostatin is a member of the transforming growth factor β family, which inhibits cellular proliferation and muscle synthesis22. Intracellular activation of the caspase pathway and myostatin stimulate protein degradation, providing the substrate for the UPS and cell apoptosis. The extensive tissue damage leads to an increase in circulating actin, which may consume gelsolin (the protein that assembles and disassembles actin) and other proteins such as the vitamin D binding protein, which have a protective role23.
High circulating actin and low circulating gelsolin levels in patients on haemodialysis are associated with an increased risk of mortality. Increased protein catabolism and an accumulation of uraemic toxins would alter gelsolin synthesis, leading to a loss in the ability to assemble actin, platelet activation, endothelial dysfunction and an increased susceptibility to infectious complications24.
Another mechanism recently reported is resistance to insulin. Insulin-like growth factor 1 would activate the phosphoinositide 3-kinase pathway, altering protein metabolism and favouring an overregulation of myostatin with a decreased proliferation of satellite muscle cells25.
PROTEIN-ENERGY WASTING DIAGNOSTIC CRITERIA PROPOSED BY THE INTERNATIONAL SOCIETY OF RENAL NUTRITION AND METABOLISM
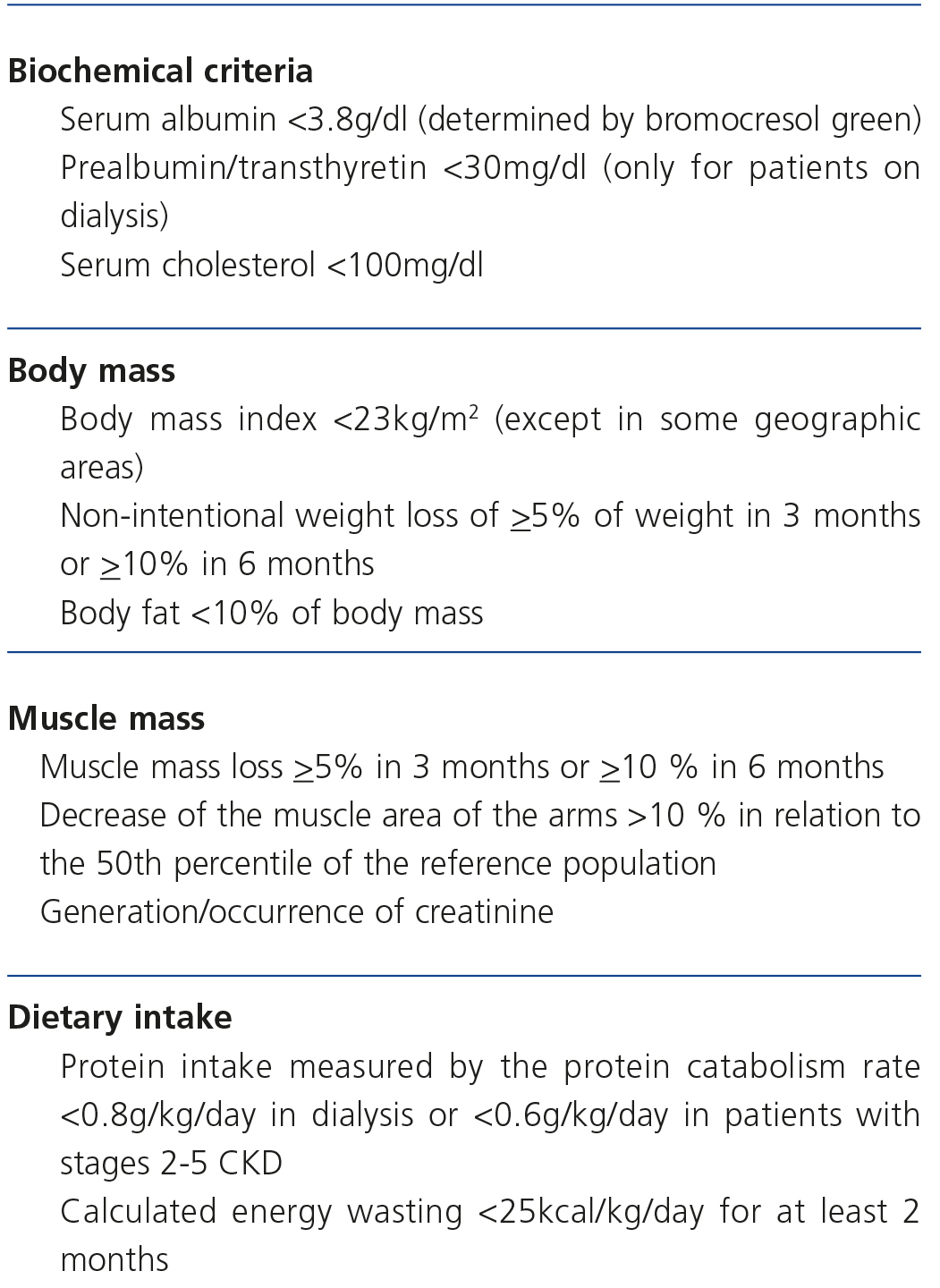
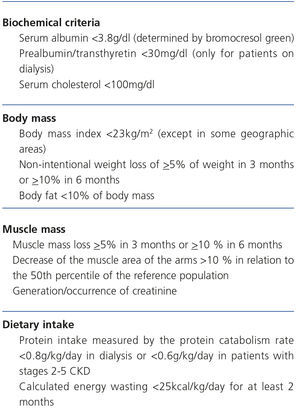
An important development is the consideration of the PEW syndrome as a single pathological condition in which undernourishment and hypercatabolism converge. An effective therapeutic approach to PEW cannot only be carried out by nutritional repletion, since this would not resolve proteolysis. A syndrome of a multifactorial origin requires diagnostic criteria and comprehensive therapy. The ISRNM has recommended diagnostic criteria (Table 2). It is necessary to fulfil at least one criterion in three of the four categories proposed (biochemical, body mass, muscle mass and intake criteria)1 (Table 2).
These criteria are initially attractive due to their multifactorial scope (analytical, anthropometric and nutritional), but when we try to apply them to clinical practice, they become confusing. Leinig et al.26 did not find any patient who had abnormalities in three of the four categories specified by the ISRNM and when the PEW syndrome was defined as abnormalities in two of the four sections, a prevalence of 17% was found, which is abnormally low if we compare it with the 65% prevalence when it is diagnosed by subjective global assessment (SGA). Another example of the questionable validity of these criteria is found in the study by Drechsler et al.27, in which they analysed the relationship between PEW and cardiovascular mortality and mortality from other causes in a cohort of 1255 diabetic patients on regular haemodialysis. They observed that no patient fulfilled the PEW criteria proposed by the ISRNM. In this case, the authors redefined the ISRNM criteria, considering there to be PEW if the body mass index (BMI), albumin and serum creatinine were below the median in the patients studied. This article has limitations resulting from the fact that the whole study population was diabetic, with a consequential association with obesity, and as such, after the adjustments, there was a 16% prevalence of PEW.
We believe that the ISRNM criteria have limitations that we must take into account. In prospective studies, these criteria should still demonstrate their superiority to other possible diagnostic combinations before their implementation becomes widespread. Recent observations illustrate this by suggesting, in a population of 570 patients on haemodialysis, that only the presence of hypoalbuminaemia had a similar or higher mortality prediction value than the sum of several malnutrition markers proposed by the ISRNM28. However, we often forget that the prediction of mortality does not necessarily equate to a diagnosis of malnutrition, and the cut-off points suggested are often based on survival analysis. Secondly, the cut-off points of the parameters proposed derive from American populations, and this leads us to wonder whether or not they can be extrapolated to other geographic areas and lifestyles such as those of Europe, Asia, or in our case, Mediterranean countries. Thirdly, the dialysis population is increasingly older and it is difficult to separate the nutritional and body composition changes that occur with age from malnutrition resulting from uraemia. For these reasons, it is logical to think that the PEW diagnostic criteria in CKD must be adapted and altered in different demographic contexts (age, race), clinical situations (obesity, diabetes, moderate and advanced CKD, dialysis and transplantation) and contextual situations (lifestyle, geographic location and culture)29.
In conclusion, although the criteria proposed by the ISRNM reinforce the complex nature of the PEW syndrome, they are based on tests/measurements that may be questionable individually-speaking30 and, moreover, their diagnostic or prognostic validity have still not been demonstrated. However, we consider that highlighting, for the first time in this definition, the multifactorial nature of PEW and the need to use different complementary nutritional state markers has been an important step forward.
PREVALENCE OF PROTEIN-ENERGY WASTING
In the dialysis population, PEW traditionally has a wide prevalence of 18%-75%26. Without a doubt, the imprecision of these figures prevents us from drawing valid conclusions. One of the problems is the variety of assessment and monitoring tools and of cut-off points that have been used to obtain these figures. Hypoalbuminaemia has been defined in the literature with figures of <4, <3.8 or <3.5g/dl, with the added difficulty of its estimation being changed according to the methodology employed (bromocresol purple or bromocresol green). As such, we should not be surprised that prevalence varies to a great extent with the methodology employed for its estimation. We are given an example of this by two studies in Brazil26 and Europe28. The prevalence of PEW varied between 23% and 74%, depending on whether it was defined by biochemical tools (albumin, creatinine), anthropometric tools (arm perimeter, BMI) or nutritional tools (SGA, energy/protein intake). The same occurs with other multi-centre studies, such as those carried out in the United States, in which a prevalence of 38%31 has been reported. Lastly, and no less importantly, PEW prevalence in different countries is a reflection of the economic situation, the degree of development and the prevalence of malnutrition in the general population, making it impossible to refer to a general prevalence in the dialysis population. This also applies to prevalence in different regions, with varying resources, of the same city or country.
In Spain, the first studies on the prevalence of malnutrition date back to 1994 and in 29 patients on chronic haemodialysis the nutritional state was analysed using anthropometric measurements such as the triceps skin fold, arm muscle circumference, BMI, visceral proteins (albumin), the normalised protein catabolic rate (nPCR) and protein intake32. They observed that in a sizeable proportion of patients (65%), the reduction of fat and protein reserves was greater than that which the relative body weight indicated (only deficient in 38%). In the same year, the first and only tables of anthropometric parameters of a Spanish population on haemodialysis were published (761 patients)33,34. In the sample studied, prevalence of malnutrition defined according to anthropometric parameters and biochemical markers (albumin, transferrin, lymphocyte count) was 52% in males and 46% in females. The predictors of malnutrition were old age, comorbidity index, male sex, time on haemodialysis and nPCR. The multi-centre Dialysis Outcomes and Practice Pattern Study (DOPPS) displayed major differences between countries in the monitoring of nutritional parameters, with Spain being one of the most deficient in the recording of these parameters35. As such, the nPCR was only recorded in 20% of dialysis units in Spain, compared with 90% in Germany and furthermore, there was only a nutritionist in 20% of units in Spain, compared with 85% in the United Kingdom. In contrast, there were no significant differences in the results of serum albumin (3.98g/dl), creatinine (9.1mg/dl) and BMI (23.9kg/m2) with the other European countries. However, the prevalence of moderate malnutrition according to the SGA scale was lower in Spain that in other countries such as France (11% versus 18%).
We must point out that the aforementioned studies included stable patients, and as such, there was a bias to eliminate critically or acutely ill patients, who probably had PEW. This leads us to believe that PEW prevalence may even be greater than that which we outline here. As such, in a recent analysis of our unit, we observed PEW prevalence, according to ISRNM criteria, of 37%, which increased to 41.1% when patients were followed up for two years36. Although the sample size was relatively small, the study included all patients in the dialysis unit (without exclusions) and we used all the ISRNM PEW criteria.
The latest S.E.N. advanced CKD nutrition guidelines published in 200837 recommend assessing the nutritional state using nutritional, biochemical, anthropometric and protein-energy intake tests.
CLINICAL IMPLICATIONS
The mortality rate of CKD patients, particularly cardiovascular mortality, is higher than in the general population38-41. This high mortality rate persists in spite of correcting traditional cardiovascular factors, such as hypotension, dyslipidaemia, left ventricular hypertrophy and improving dialysis techniques42. PEW may be considered a new risk factor, underlying the phenomenon of reverse epidemiology, where markers that in the general population are associated with a lower probability of cardiovascular events, such a decreased BMI or low cholesterol levels, are associated with a higher presence of cardiovascular disease and lower survival in dialysis patients43.
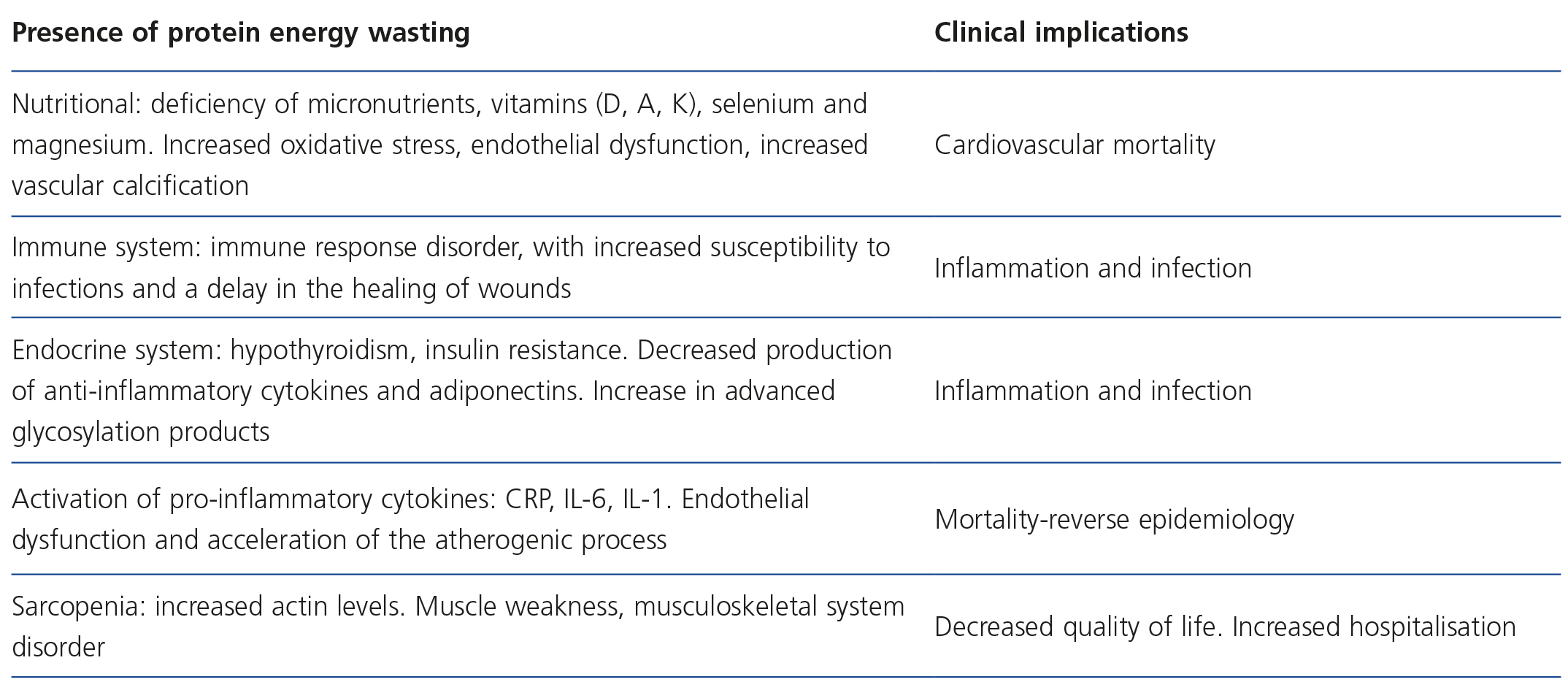
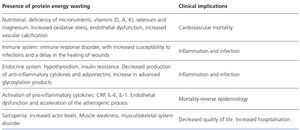
The presence of PEW in renal patients leads to the activation of compensatory mechanisms and the deregulation of others, which affects different organs and systems, including the immune, endocrine, musculoskeletal, adipose tissue, haematopoietic and gastrointestinal systems and causes poor adaptation to the inflammatory cascade activation44,45, leading to an increase in overall mortality (Table 3).
Protein-energy wasting and cardiovascular mortality
In patients with advanced CKD, malnutrition and the presence of PEW are significantly related to cardiovascular mortality46,47. Nutrients are necessary for the body to function correctly. Dietary restrictions in uraemic patients that limit potassium, phosphorus or sodium intake, amongst others, may lead to deficiencies of other essential nutrients if there is no dietary advice from healthcare staff. Essential nutrients are necessary for tissue synthesis and energy production, whilst being coenzymes in most enzymatic reactions in the body. Specific nutritional deficiencies, such as selenium, magnesium or vitamin D deficiencies, so common in kidney patients, have negative consequences on the antioxidant and anti-inflammatory capacity and on mineral and bone metabolism. As such, PEW is associated with a higher risk of infection and death due to infectious causes29,48. Deficiency of vitamins A, K and D is associated with greater cardiovascular mortality in haemodialysis patients49,50. Up to 80% of haemodialysis patients have a vitamin K deficiency due to insufficient intake (140µg/day versus 200µg/day in healthy patients). Subclinical hepatic vitamin K deficiency increases vitamin K-dependent non-carboxylated inactive proteins and may contribute to an increased risk of bone fractures and vascular calcification. Vitamin K supplements (menaquinone-7) decrease non-carboxylated proteins in haemodialysis patients and prolonged treatment can increase vascular elasticity51-53.
PEW promotes increased muscle catabolism in uraemic patients, both due to the lack of circulating nutrients and due to the combined effect of systemic inflammation, metabolic acidosis, uraemic toxins and other factors. The result is a loss of muscle mass, which also affects the muscle tissue of the arteries and heart, with direct associations being found between malnutrition, arterial stiffness and abnormalities in myocardial structure. Continuous vascular distension resulting from salt and water overload aggravates this process and promotes ventricular hypertrophy. An example of how pure undernourishment leads to cardiovascular system abnormalities is found in the Minnesota experiment, conducted in 1944 during World War II. The aim was to better understand the pathophysiology of the undernourishment to which the Jews were subjected in the concentration camps. 36 volunteers underwent a controlled reduction in intake that resulted in a total loss of 25% of their weight. Undernourishment caused a decrease in cardiac volume of 17%, with reduced cardiac output, bradycardia, hypotension, and a decrease in peripheral oxygenation and in myocardial contractility54.
Hypoalbuminaemia is the most common and most frequently used biomarker for measuring PEW in dialysis and it is a powerful prognostic marker of morbidity and mortality55,56. Furthermore, hypoalbuminaemia has been associated with the de novo development and recurrence of congestive heart failure in patients on haemodialysis and peritoneal dialysis57. In the 4D study carried out in a cohort of 1255 diabetic haemodialysis patients, we investigated the effect of PEW on mortality after four years. The presence of PEW (defined as BMI 26.7kg/m2, serum albumin <3.8g/dl and creatinine <6.8mg/dl) doubled the risk of overall mortality, death due to infections and sudden death of cardiac origin, but it was not related to a higher incidence of heart attacks. The presence of non-arteriosclerotic cardiovascular disease in this study was greater in patients with PEW as a cause of the cardiovascular events27.
The hormonal abnormalities associated with uraemia, such as subclinical hypothyroidism58 or low T3 syndrome59, are associated with inflammation and malnutrition60 and may contribute to cardiovascular disease. As such, an independent association has been observed between hypothyroidism and cardiovascular mortality in haemodialysis patients61,62. In patients with subclinical hypothyroidism and failure, the administration of synthetic T3 improved the neuroendocrine profile, with a significant decrease in levels of norepinephrine and B-type natriuretic peptide (pro-BNP) compared to the placebo. Furthermore, we observed an increase in diastolic volume of the left ventricle with increased cardiac output, without observing an increase in preload63. The decreased synthesis of other anabolic hormones such as testosterone64 is also associated with greater muscle loss65, endothelial dysfunction66, anaemia, resistance to erythropoietin67 and mortality68.
PROTEIN-ENERGY WASTING, INFECTION AND HOSPITALISATION
Uraemia is considered to be acquired immunodeficiency state69 and patients with CKD have a high risk of infection70. In the HEMO study, infection was the first cause of death (23%) and the risk of death associated with an infection during hospitalisation was 15%. The factors that predispose CKD patients to infection according to the HEMO study were old age, hypoalbuminaemia, immunosuppressive therapy and catheters as vascular access71. In parallel, in the DOPPS29 study, infection was the cause of 55% of death in haemodialysis patients and it was related to hypoalbuminaemia, low nPCR and cachexia.
The definition of the malnutrition status according to the concept of PEW leads to a deficiency of the immune system and an abnormal response in the patient, and as such, it is associated with greater susceptibility to infections and a slow recovery from injuries72. The deficiency of certain micro-macronutrients favours a state of immunodeficiency. Some amino acids such as arginine and glutamine act and favour the immune response73. A severe zinc, vitamin B6 (pyridoxine), vitamin C and folic acid deficiency74-76 alters the immune response, decreases the production of antibodies, causes polymorphonuclear leukocyte or lymphocyte dysfunction and delays the scarring and curing of injuries. Haemodialysis patients with PEW are exposed to a greater risk of infection and its complications, increasing mortality77. For example, in infection by the hepatitis C virus, the presence of hypoalbuminaemia and a high result in the MIS (malnutrition inflammation score) scale is independently associated with active infection and increased viral replication78.
In hospitalised patients, a deficient nutritional state delays recovery, prolongs hospitalisation, increases the rate of infections and re-admissions and increases dependency upon discharge and the need for institutionalisation. In dialysis patients with prolonged and complicated hospitalisation, there is a rapid decrease in albumin and weight loss, particularly in those who have previously been undernourished, elderly patients and those with comorbidities and anorexia79. The recommendations of the guidelines on the prevention and management of hospital undernourishment may be useful in hospitalised patients with CKD, since they include the use of supplements and parenteral nutrition to improve the nutritional situation80.
PROTEIN-ENERGY WASTING AND INFLAMMATION
Several studies have observed an independent association between inflammatory conditions, commonly measured by an increase in C-reactive protein (CRP), IL6, IL1 and TNF-α, with the risk of cardiovascular mortality in haemodialysis patients81 and in the general population82.
Inflammation is associated with both anorexia and an increased protein catabolism83,84 and it seems to be the connection that explains the relationship between PEW and mortality in CKD.
The relationship between malnutrition and inflammation in patients with CKD may be one of the causes of mortality associated with malnutrition. Moreover, PEW may also be the result of chronic inflammatory states in patients with renal failure85,86.
PROTEIN-ENERGY WASTING AND QUALITY OF LIFE
An aspect that is sometimes underappreciated by nephrologists, but which is increasingly important in clinical practice, is the impact of nursing on the degree of patient functionality. The impact of CKD on overall patient functioning can be recorded in quality of life surveys such as PROs (patient-reported outcomes) and Qo1 (health related quality of life) surveys, which assess the mental and functional state of the patient. CKD is associated with a poor QoL and this leads to a higher risk of mortality87. QoL has also been related to malnutrition markers, where worse values for QoL are associated with low levels of albumin, plasma creatinine, loss of LBM (lean tissue, mainly muscle tissue) and a high percentage of fat88. An improved QoL has become one of the objectives in dialysis patients.
The prevalence of mental states of depression and anxiety is high in dialysis patients89. They face situations such as hospitalisation, anxiety due to changes in dialysis, dietary and water restrictions and the adaptation of dialysis to their daily lives. The fear of inability, disability and a lower life expectancy are at the heart of these changes in frame of mind. New methods and tools are being developed to measure depression and anxiety and it has been acknowledged that anxiety is under-diagnosed90.
REVERSE EPIDEMIOLOGY IN RENAL FAILURE: IMPLICAIONS OF NUTRITIONAL STATE
In the evaluation of morbidity and mortality risk factors in CKD patients, we often observe paradoxically opposed trends to those observed in the general population. A clear example is obesity, which in observational studies, appears to be a protective factor against mortality in the final stages of CKD. This is what is known as the reverse or paradoxical epidemiology uraemic obesity phenomenon. The cause of these reverse epidemiology phenomena is the devastating effect that PEW has on short-term survival, which does not leave enough time for other traditional risk factors to act in long-term mortality91. The most striking examples of this include the case of hypercholesterolaemia, which has a reverse association with mortality in uraemic patients. When patients are divided according to whether they do or do not have PEW, we observe that in the presence of PEW, hypercholesterolaemia is a protective factor, while in the absence of PEW, it is a risk factor. In a situation of energy consumption affecting the patient, cholesterol temporarily becomes a marker of the body’s fat reserves, and when there is more fat, the patient can resist this energy consumption for longer.
The same reasoning applies to the paradox of obesity. Dialysis patients, independently of the method used, have an inversely proportionate relationship between BMI and mortality92, differing from the general population, in which this relationship is U-shaped (both extremes, malnutrition and obesity have increased mortality)93. In this instance, obesity involves an excess energy state that helps patients resist PEW. However, long-term obesity is a risk factor related to inflammation, atherosclerosis and calcification, for example94. This is due to the endocrine nature of adipocytes and the ability to regulate these processes by cytokine and adipocytokine secretion95. Endocrinologically active fat, fundamentally that which accumulates in the abdomen, promotes these processes. As such, the amount of total fat (reflection of the health of energy reserves) and abdominal fat (participating in obesity-associated risk) may have opposite effects on patient risk96.
Another explanation of the reverse epidemiology of BMI in uraemia is the inability of the BMI to distinguish between muscle mass, body fat distribution (abdominal versus peripheral) and hypervolaemia. Therefore, we were recently able to observe that a BMI >30kg/m2 was not capable of distinguishing excess body fat in 65% of dialysis patients43. Recent studies highlight that the type and distribution of fat, more than the total fat, is a determining factor of risk97. Specifically, the accumulation of abdominal fat is a risk factor and is associated with greater secretion of pro-inflammatory adiponectins98. It has been reported that both leptin and visfatin are activators of cardiovascular disease and are endothelial dysfunction risk factors99,100. Observational studies based on creatinine kinetics suggest that the protective effect of BMI in haemodialysis patients is due to its indication of greater muscle mass101. In dialysis patients, it is perhaps necessary to conserve both tissues, fat and muscle. In this respect, a low arm muscle circumference percentile as an indicator of muscle mass and a low triceps skin fold as an indicator of fat tissue are related in equal measure to higher mortality in haemodialysis patients102. Lastly, the risk of mortality increases whenever BMI, creatinine and weight progressively decrease, but if weight decreases and creatinine increases, the risk of mortality is reduced103.
CONCLUSION
The term protein-energy wasting or PEW attempts to unite in one sole pathological condition the many nutritional and catabolic disorders that occur in CKD and which lead to a gradual and progressive loss of both muscle and fat mass. It is a common syndrome, particularly from stage 4-5 CKD, which is present in 30%-60% of dialysis patients. The clinical consequences of PEW may be severe and require rapid and effective treatment, since it is associated with increased overall and cardiovascular mortality, an increased number of infections and admissions and many other comorbidities. The devastating effect of PEW causes paradoxical epidemiologies that are explained by competition between short- and long-term risk factors.
ACKNOWLEDGEMENTS
ISCIII-RETIC REDinREN/RD06/0016 and 12/0021, PIE13/00051, Spanish Society of Nephrology, Swedish Research Council, Research Activity Intensification programme (ISCIII).
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
KEY CONCEPTS
- Protein-energy wasting is defined as a pathological state where there is a continuous decrease or wasting of both protein deposits and energy reserves.
- The pathophysiological mechanisms involved in PEW are anorexia and increased protein catabolism, which lead to an energy imbalance, with the final result of increased energy wasting.
- For a correct diagnosis of PEW, we require the assessment of biochemical and body composition markers and a calculation of muscle loss and dietary intake.
- The presence of PEW is associated with an increased cardiovascular risk, a risk of infection, hospitalisation and mortality, inflammation and a decreased quality of life.
- The presence of PEW is explained by the known reverse epidemiology phenomenon, in which traditional risk factors appear as protection factors.
Table 1. Causes of developing protein-energy wasting in chronic kidney disease
Table 2. Diagnostic criteria for protein-energy wasting proposed by the International Society of Renal Nutrition and Metabolism
Table 3. Underlying clinical impacts of the protein-energy wasting syndrome that lead to higher mortality