Haemophagocytic syndrome (HS) or haemophagocytic lymphohistiocytosis is an uncommon disease characterised by a hyperactive and inefficient immune response to antigen presentation. Its origin is the inherent (primary) or acquired (secondary) incapacity of cytotoxic T-lymphocytes and natural killer (NK) cells to prduce cell lysis.1–4 This immune dysregulation gives rise to a marked proliferation of histiocytes and lymphocytes that invade various organs (spleen, liver, lymph nodes, among others), leading to overproduction of cytokines and consequently systemic inflammatory response syndrome (SIRS), multiorgan dysfunction, and even death.5 It has been suggested that COVID-19 possesses HS-like pathogenic mechanisms,6 so the latter is included in its differential diagnosis. Acute kidney failure is a common manifestation associated with multi-system involvement of this syndrome, and is associated with a worse prognosis.7 Given the coincidence in the time of the diagnosis of this case and the peak of the SARS-CoV-2 outbreak in our community, we believe its discussion is relevant.
A 51-year-old male with normal renal function and a history of hypertension attended the emergency room due to intermittent fever and weight loss of three weeks’ duration associated with jaundice and choluria in the days prior to hospital admission. In the physical examination he presented cutaneous and conjunctival jaundice. The blood work showed a serum creatinine of 3.4 mg/dl (estimated glomerular filtration rate (eGFR) by CKD-EPI 19.8 ml/min/1.73 m2), plasma sodium 126 mEq/l, plasma osmolality 271 mOsm/kg, pancytopenia (leukocytes 1,000 U/l, Hb 9.62 g/dl and platelets 50,900 U/l), triglycerides 689 mg/dl, ferritin 33,511 ng/mL, AST 218 U/l, ALT 113 U/l, LDH 1.751 U/l, GGT 223 U/l, ALP 962 U/l, total bilirubin 9.29 mg/d. (direct bilirubin 9.21 mg/dl) and fibrinogen 139 mg/dl. The urinalysis found microhaematuria with 25 red blood cells (5–10 per field), fractional excretion of sodium 2.7% and proteinuria 1.48 g/24 h. The SARS-CoV-2 PCR study was negative and serology for bacteria, autoimmunity and a blood smear were unremarkable. Nevertheless, haemophagocytes were found in bone marrow (BM) aspirate. In addition, BM biopsy revealed signs compatible with T-cell non-Hodgkin lymphoma and the viral load in blood of the Epstein-Barr virus was 644,558 copies, with a BM culture also positive (454,386 copies). The CT of abdomen showed hepatosplenomegaly and mediastinal, retroperitoneal, iliac and inguinal adenopathies. According to the HScore,8 the probability of HS was greater than 99%. A lymph node biopsy was performed that revealed extranasal NK/T lymphoma. Specific treatment was started with fluid therapy adjustment, two doses of rituximab, three doses of gammaglobulin and two doses of etoposide and, from a nephrology point of view, the patient presented gradual improvement of kidney function, reaching a serum creatinine level of 1 mg/dl (eGFR CKD-EPI 86.8 ml/min/1.73 m2) and proteinuria of 1.1 g/24 h 20 days after our first assessment.
Haemophagocytic syndrome is characterised by an aggressive but ineffective response to a noxious substance. Its importance during the current pandemic arises from that fact that it has high mortality and requires high diagnostic suspicion, given its similarity with severe SARS-CoV-2 infection and Systemic Inflammatory Response Syndrome (SIRS) secondary to sepsis, trauma or autoimmune/autoinflammatory processes.6,9 Renal involvement in this syndrome may result in acute kidney failure (the most common form of presentation), glomerulopathy,10 or thrombotic microangiopathy (TMA).11 The presence of acute kidney failure has an incidence that varies from 8% to 62%, according to different series.7 Aulagnon et al.7 found that up to 78% of cases presented a multifactorial cause, the most common were acute tubular necrosis, hypoperfusion, use of nephrotoxic agents and tumour lysis syndrome. A 86% presented acute kidney failure ≥2, and 59% required renal replacement therapy. There are cases reported in kidney transplant recipients, generally triggering by viral infection, as in the case being presented.12,13 In our patient, the acute kidney failure was likely secondary to acute tubular necrosis in a context of renal hypoperfusion and hyperbilirubinaemia with a subsequent gradual recovery of renal function. Proteinuria may be present, even in nephrotic ranges, as is described by Thaunat et al.10; in this collection of cases the glomerulopathies involved were: minimal changes, focal segmental glomerulosclerosis and TMA. In our case, no renal biopsy was performed due to the high risk of bleeding, a common problem in this type of pathologies.7
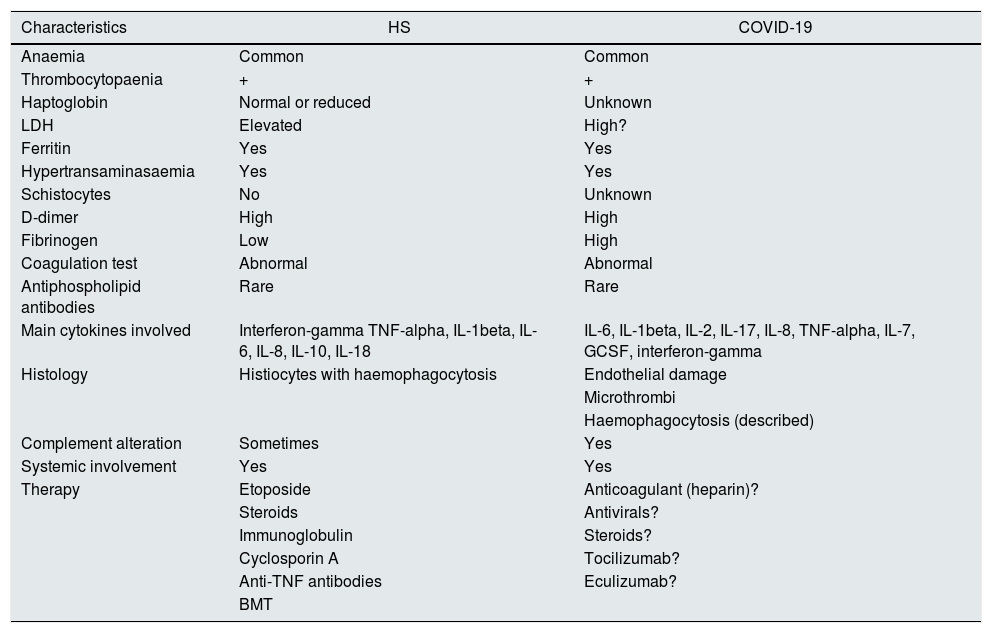
To conclude, the Hemophagotic Syndrome is a rare entity that require a high degree of clinical suspicion for its diagnosis. Moreover, since it shares clinical characteristics with SARS-CoV-2 infection, we believe it is necessary to consider it within the differential diagnosis (Table 1).6,11,14 As nephrologists, we need to be aware that renal involvement is common and it is associated with a poor prognosis. The possibility of renal biopsy may be considered after careful assessment of the risk-benefit ratio.
Comparison between haemophagocytic syndrome (HS) and COVID-19 (adapted from Valga et al.).
| Characteristics | HS | COVID-19 |
|---|---|---|
| Anaemia | Common | Common |
| Thrombocytopaenia | + | + |
| Haptoglobin | Normal or reduced | Unknown |
| LDH | Elevated | High? |
| Ferritin | Yes | Yes |
| Hypertransaminasaemia | Yes | Yes |
| Schistocytes | No | Unknown |
| D-dimer | High | High |
| Fibrinogen | Low | High |
| Coagulation test | Abnormal | Abnormal |
| Antiphospholipid antibodies | Rare | Rare |
| Main cytokines involved | Interferon-gamma TNF-alpha, IL-1beta, IL-6, IL-8, IL-10, IL-18 | IL-6, IL-1beta, IL-2, IL-17, IL-8, TNF-alpha, IL-7, GCSF, interferon-gamma |
| Histology | Histiocytes with haemophagocytosis | Endothelial damage |
| Microthrombi | ||
| Haemophagocytosis (described) | ||
| Complement alteration | Sometimes | Yes |
| Systemic involvement | Yes | Yes |
| Therapy | Etoposide | Anticoagulant (heparin)? |
| Steroids | Antivirals? | |
| Immunoglobulin | Steroids? | |
| Cyclosporin A | Tocilizumab? | |
| Anti-TNF antibodies | Eculizumab? | |
| BMT |
BMT: bone marrow transplant. GCSF: granulocyte colony-stimulating factor.
Funding
The authors did not receive financial support for the research, auditing and/or publication of this article.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Please cite this article as: Santana Quintana A, Valga F, Vega Díaz N, Fernández JM, Quevedo Reina JC, Rincón Tirado M, et al. No todas las tormentas de citoquinas son por COVID-19: Síndrome hemofagocítico con afectación renal, secundario a linfoma extranasal y virus de Epstein-Barr. A propósito de un caso durante la pandemia. Nefrologia. 2020. https://doi.org/10.1016/j.nefro.2020.07.004