La espondilodiscitis es una infección del cuerpo vertebral y los discos adyacentes, cuya forma de diseminación más frecuente es la vía hematógena. Se trata de una entidad rara pero con una incidencia global en aumento, debido principalmente al incremento de bacteriemias en portadores de dispositivos intravasculares, como el utilizado en pacientes en tratamiento renal sustitutivo con hemodiálisis. Su diagnóstico es difícil por presentarse con síntomas inespecíficos, por lo que para un diagnóstico precoz y preciso es necesario el uso de la resonancia magnética. El tratamiento antibiótico empírico temprano y el abordaje multidisciplinario mejoran el pronóstico de esta infección potencialmente grave. Presentamos una serie de casos diagnosticados de espondilodiscitis en nuestra Sección de Nefrología.
Spondylodiscitis is an infection of the vertebral body and adjacent intervertebral discs, whose most common means of spreading is the haematogenous route. It is a rare disease but its overall incidence is increasing, mainly due to increased bacteraemia in patients with intravascular devices, such as that used in patients on renal replacement therapy with haemodialysis. Its diagnosis is difficult due to non-specific symptoms and as such, for early and accurate diagnosis, MRI is necessary. The early empirical antibiotic treatment and the multidisciplinary approach may improve the prognosis of this potentially serious infection. We report a series of cases diagnosed with spondylodiscitis in our Nephrology Unit.
INTRODUCTION
Spondylodiscitis (SD) or vertebral osteomyelitis (OM) is an infection, normally bacterial, which affects the vertebral bodies (spinal and cortical) and their respective intervertebral discs, with osteomyelitis in adults being around 2-7%; said infection produces a progressive inflammatory reaction that leads to the destruction, instability and subsequent ankylosis of these structures.1
Its incidence is approximately 2.4 to 6 cases/100 000 people/year, with a mortality rate of around 5%. However, these numbers are raising due to increased life expectancy, the use of immunosuppressive therapy and especially the increased use of intravascular devices (IVD).2 The most common form of spread is haematogenous and it primarily affects the lumbar vertebrae due to its greater vascularity. It is associated with myeloradicular involvement in 20% and with endocarditis in 4-15% of cases.1,3 A single bacterium can be identified in almost 90% of cases, with a predominance of gram-positive cocci (60-75%), with Staphylococcus aureus being the main cause (30-45% methicillin resistant).4,5
Haemodialysis patients have higher rates of infectious SD due to development of bacteraemia associated with the use of IVD (1.5-5.5 episodes per 1000 catheter days), of which 1.3% will develop this infection at some point, and it is three times more common with the use of a central catheter than with an arteriovenous fistula.6
METHODOLOGY
We reviewed the medical records of patients diagnosed with SD or OM, hospitalised in the Nephrology service of the Hospital General Universitario of Ciudad Real in the past four years (2008-2012).
RESULTS
We obtained a series of 6 nephrology patients diagnosed with SD or OM, 5 associated with haemodialysis through an indwelling jugular catheter (IJC) and one with immunosuppressive (IS) treatment (Table 1).
CASE 1
A 64-year-old female with a history of type 2 diabetes mellitus (DM), high blood pressure (HBP) and stage V chronic kidney disease (CKD) secondary to membranoproliferative glomerulonephritis type I in haemodialysis with IJC. She was transferred from her centre due to severe incapacitating pain in the back region, for almost a month, increasingly interfering with her dialysis sessions and associated with fever episodes. The analysis showed significant leukocytosis and an elevated erythrocyte sedimentation rate. Bone scintigraphy was performed, which described pathological uptake at D10 suggestive of acute infection, and as such MRI was performed and confirmed the diagnosis of SD D9-D10. Empirical treatment was begun with vancomycin and ceftazidime. Subsequently, despite the treatment, the clinical situation did not improve, and she was assessed by doctors from Neurosurgery, who decided to perform discectomy and arthrodesis; methicillin-sensitive Staphylococcus aureus (MSSA) was identified in both blood cultures and in the surgical sample. She was discharged with antibiotic treatment by vancomycin and ceftazidime in accordance with antibiogram, analgesia with fentanyl patches and dorso-lumbar corset. However, the clinical and analytical situation worsened and a new scintigraphy was performed with marked leukocytes showing pathological uptake at the central catheter. It was replaced by a femoral catheter, which had a complication with a thrombotic episode. It was adjusted with antibiotics and supportive treatment on several occasions with little response. Finally, evolution was poor and the patient died.
CASE 2
A 75-year-old male with a history of long-standing HBP, vesicular lithiasis with an episode of pancreatitis, infrarenal abdominal aortic aneurysm and stage V CKD due to multicystic dysplastic kidney, using IJC. He was transferred from his dialysis centre due to 3 weeks of progressive inflammatory pain at the lumbosacral level radiating to the lower limbs, associated with fever and general malaise. In the admission workup, leukocytosis or alterations in acute phase reactants were not observed. Bone scintigraphy was performed, which showed pathological uptake at L3-L4 compatible with SD, which was confirmed with MRI, which also showed multiloculated paravertebral collection surrounding both vertebral bodies. Empirical treatment was begun with vancomycin and ceftazidime with good clinical evolution. Analgesia with fentanyl patches and dorso-lumbar corset were recommended. He was assessed by doctors from Neurosurgery, who did not consider surgery necessary. Subsequently, he was discharged with vancomycin and ceftazidime in dialysis because blood cultures were negative. Approximately one month after discharge, he presented a complication with abdominal sepsis due to cholangitis with choledocholithiasis, highlighting marked leukocytosis, a notable increase in acute phase reactants and extended-spectrum beta-lactamase Escherichia coli positive blood culture. He was admitted to the Intensive Care Unit, where he died a few days later.
CASE 3
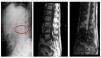
A 63-year-old-male with a history of long-standing DM, liver disease due to hepatitis C virus, pulmonary tuberculosis, peripheral arterial disease and stage V CKD on haemodialysis, who received renal transplant with recurrence of renal dysfunction, restarting haemodialysis with IJC. He came to the Emergency department following 5 days of severe lower back pain with apparently mechanical characteristics associated with fever of 38°C on occasions. The analysis emphasised high leukocytosis with left shift, C-reactive protein of 12.9 and procalcitonin of >10. A bone scintigraphy was performed, where increased uptake foci were not observed, suggesting infectious-inflammatory process. However, the MRI showed images compatible with L3-L4 SD with paravertebral abscess (Figure 1). Blood cultures were positive for vancomycin-sensitive Staphylococcus epidermidis, linezolid and co-trimoxazole. The use of lumbar corset, analgesic treatment with fentanyl patches and antibiotic coverage are prescribed, initially with intravenous vancomycin in dialysis for 3 months, which was changed to daptomycin due to persistent clinical symptoms. After nearly 6 months of treatment, significant clinical improvement, negative blood cultures and near normalisation of acute phase reactants was achieved. The patient remains on haemodialysis without any other significant complication.
CASE 4
An 80-year-old male with a history of HBP, chronic obstructive pulmonary disease, dyslipidaemia, diagnosed with nephrotic syndrome by minimal change glomerulonephritis with impaired renal function (stage IV CKD) for two years and chronic treatment with prednisone 30mg/day and cyclosporine 50mg/day. He was hospitalised because of malaise due to bacteremia and urinary infection by methicillin-resistant Staphylococcus aureus (MRSA), and was treated with daptomycin. Subsequently, significant lower back pain began with inflammatory characteristics associated with fever, leukocytosis with left shift and a C-reactive protein of 40; bone scan was performed without evidence of inflammatory disease, but the MRI shows signs of D6-D7 SD with a small left paravertebral collection, and as such, intravenous daptomycin treatment is carried out for about 4 weeks. Pain control was achieved with fentanyl patches and semi-rigid corset. Subsequently the patient is switched to orally-administered linezolid and rifampicin to complete 8 weeks, achieving negative blood cultures, decreasing C-reactive protein down to 1.7 and showing significant clinical improvement.
CASE 5
A 38-year-old female with a history of obesity, HBP, hypothyroidism and stage V CKD with a single functioning kidney, secondary to vesicoureteral reflux, on haemodialysis for 3 years, with IJC. She was admitted due to fever, analysis and radiology compatible with left basal pneumonia. During her hospitalisation, she developed bacteremia with MSSA positive blood culture, and therefore she started antibiotic therapy with ceftazidime, levofloxacin and it was decided to withdraw IJC. Subsequently, she complained of severe back pain radiating to the ribs which was not controlled with standard analgesia, so MRI is performed with findings consistent with SD at D8-D9. Analgesia was recommended (fentanyl patches), corset, and on discharge, antibiotic therapy with orally administered levofloxacin and rifampicin was continued for six weeks, with negative blood cultures, significant clinical improvement and normalisation of acute phase reactants being obtained. To date, no other complication has arisen.
CASE 6
An 81-year-old female with a history of hypertension, hyperuricaemia, dyslipidaemia, coronary disease of 2 vessels with percutaneous revascularization and stage V CKD on haemodialysis for 8 years, with IJC. She has had lower back pain for the last 20 days progressing in intensity, which was incapacitating and radiated to both legs, with a fever of 38.5°C in the last week. Antibiotic therapy was initiated empirically with vancomycin and ceftazidime. Subsequently, given the persistence of lower back pain, an MRI was performed, finding objective signs of SD in L5-S1 compromising L5 spinal root nerves with left predominance. Enterococcus faecalis was isolated in the urine culture, and as such antibiotic therapy was changed to vancomycin and cefotaxime, intensifying analgesia with fentanyl patches and a corset was used due to the risk of compromising the spine. She was assessed by doctors from Neurosurgery, who decided on conservative management, given the favourable clinical response and normalisation of blood parameters. She is currently on haemodialysis without any other significant incidents.
DISCUSSION
The incidence of SD has increased in recent years; among the factors that determine this incidence increase are higher life expectancy in the population, the use of IS treatment and mainly the involvement of intravascular devices.3,7
Our series of SD cases consists of 6 patients, with equal involvement regarding sex, contrary to what is described in literature, where there is a predominance of males over females in a ratio of 2/11.6 Moreover, the average age of our series is similar to that described in other case series (50-70 years).6,8,9
The distribution of our patients according to associated risk factors was: 5 patients on haemodialysis with IJC and one with pharmacological immunosuppression (corticosteroids plus cyclosporine); this association has been reported in several articles, which describe that patients with nephropathy, on haemodialysis6-8 and/or IS treatment9,10 constitute a subpopulation at risk of developing bacteremia and subsequently SD symptoms. The existence of a condition characterised by fever, inflammatory upper and/or lower back pain and general malaise were the most common clinical symptoms in our series of cases, and as such, the development of these symptoms in these patients must also lead us to suspect this disease.5,9
In a blood test, an increase in acute phase reactants is usually observed in 80% of cases, being mainly the erythrocyte sedimentation rate and C-reactive protein. Its steady decline is an excellent marker of adequate response to treatment, with levels decreasing between the first-second week.3 In our patients, we found a marked increase in C-reactive protein at the time of diagnosis, with a subsequent decrease as the weeks of antibiotic treatment progressed.
Blood cultures usually identify the bacteria at the root in 70% of cases, the results of tissue samples obtained in CT-guided biopsy have a sensitivity of 62-91% and a specificity close to 99%.2 In our case series, the cultures were positive in 5/6, which identified the bacteria and selected the most appropriate antibiotic for treatment. Staphylococcus aureus was the most common bacteria isolated, similar to that reported in literature.1,7,11 Also, because the SD stems from bacteraemia, the development of associated infective endocarditis can reach 30% in these patients3,6,12, so echocardiogram was performed in 6 cases, without noting the existence of verrucas that suggested said infectious process.
Although the use of bone scintigraphy provides relevant information in such cases, it has low sensitivity and specificity compared with MRI, which was crucial to the diagnosis and extension in all our patients; this is supported in current literature, which describes resonance as the initial imaging test on suspecting SD and blood analysis for its high sensitivity and specificity, and the earliness in detecting pathologic changes; its usefulness in follow-up is still debated.5,13,14
Medical treatment in most cases is conservative, with intravenous antibiotics for 4-6 weeks. Subsequently, it is recommended that treatment be continued orally 12-24 weeks depending on clinical evolution and inflammatory markers. Opiate analgesia is also important in the first weeks as well as orthopaedic means for immobilisation of the affected area for about 8-12 weeks.4,15,16 Vertebral involvement is in an area of low antibiotic penetration, so high doses are required intravenously; the highest penetration is achieved with fluoroquinolones, lincosamides, rifampicin and cotrimoxazole; those with the lowest penetration are the beta-lactams, glycopeptides and aminoglucosides.1 Given the need to start antibiotic treatment early, the articles recommend empirical guidelines covering gram-positive and gram-negative consisting of vancomycin (given the increasing prevalence of MRSA) associated with a cephalosporin (cefotaxime, ceftazidime, ceftriaxone or cefepime) or a fluoroquinolone. Also, the association with rifampicin in cases of MRSA should be considered for its high effectiveness, demonstrated in literature,6,7 and thereafter, the ideal treatment depends on the specific isolated microorganism.5 This therapeutic approach was followed in our series of cases, with a relatively acceptable response which depended on the associated comorbidities and early diagnosis. Neurosurgical management is indicated in cases of marrow involvement (severe or rapidly progressive root), poor response to drug treatment, significant bone involvement associated with instability or deformity, intraspinal abscess, the need for correct diagnosis and histopathological and bacteriological and persistent and uncontrolable pain.17 In our series of cases, only surgical management was considered in the first case.
The severity involved in SD and the high mortality rate associated (5-25%)4,6,8,11 makes the early diagnosis and treatment the major determinant of prognosis. In our series, there was a mortality rate of 33.3% (2/6), higher than the average mortality reported in literature. However, other series, as that described by Garcia-Frias at the 40th Meeting of the Andalusian Society of Nephrology in May 2012, reported a mortality rate higher than ours of 57% (4/7).
CONCLUSION
The incidence of infectious SD is increasing, mainly due to the increased use of intravascular devices in haemodialysis patients, with this population constituting a risk group that should be closely monitored, given the high mortality associated with this disease. Early diagnosis and treatment are the most important therapeutic and prognostic weapons. MRI is the primary imaging test for confirming the diagnosis, and antibiotic therapy, the removal of the central venous catheter, rest with a discharge prosthesis and effective analgesia, are its most appropriate forms of treatment, with a coordinated approach being necessary with the Services of Rheumatology and Infections.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. Characteristics of the patients who developed spondylodiscitis
Figure 1. Radiology and MRI