The rapid and unprecedented spread of severe acute respiratory syndrome coronavirus disease 2019 (COVID-19) has significantly limited our understanding of this disease. As the pandemic continues to evolve,1 cardio-pulmonary symptoms predominate, however new atypical manifestation of COVID are increasingly recognized.
To alert clinicians regarding a novel presentation of COVID-19. We present the first reported case of SARS-COV2 induced syndrome of inappropriate diuretic hormone (SIADH) manifesting as new-onset seizures.
A previously healthy 75-year-old man presents with a witnessed episode of new-onset seizures. Per family accounts, the episode lasted three minutes with tonic-clonic movements of all extremities, followed by a period of confusion. He had endorsed worsening fatigue and headaches with a declining appetite over the preceding two weeks. There was no history of cough, respiratory symptoms, sick contacts or prior similar episodes. Travel history was significant for a trip to California two weeks prior. He denied any medication, health supplement or illicit substance use. Past medical, surgical and family histories were unremarkable. On examination, the patient was obtunded and afebrile (37.3°C). He appeared visibly dyspneic, with an SpO2 of 85% on room air and RR of 34/minute, but remained hemodynamically stable. Lung auscultation revealed scattered bilateral crackles while the neurological exam was non-focal. Clinically the patient appeared euvolemic. Computed tomography of the brain was unrevealing with no additional explanation for his prolonged altered mentation. Chest-radiography revealed bilateral air-space opacities.
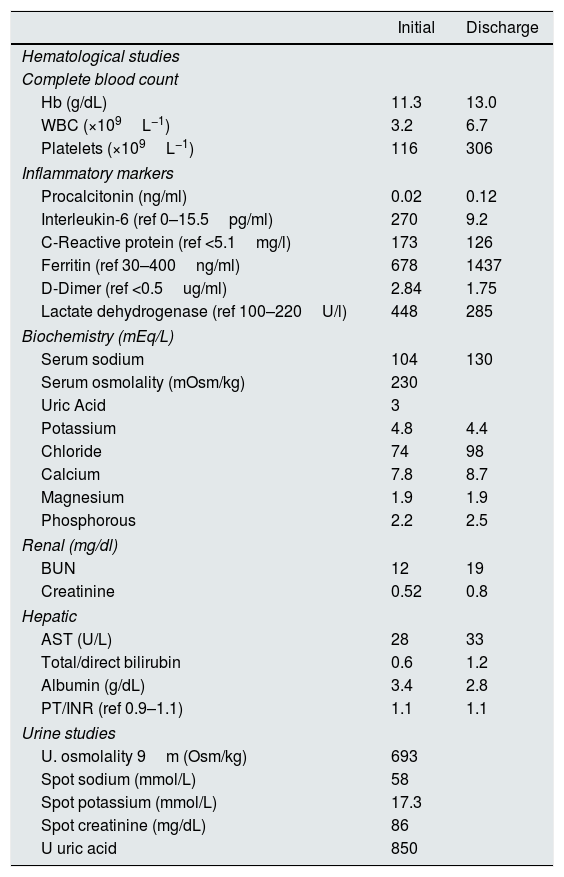
Labs indicated mild leukocytopenia (3.2×109L−1) with lymphopenia (0.6×109L−1) and a profound hyponatremia of 104mEq/L. Renal and liver parameters were normal. Workup of his hyponatremia revealed a serum and urine osmolality of 230mOsm/kg and 693mOsm/kg respectively with a urine sodium of 58mmol/L. TSH and cortisol levels were normal. Inflammatory markers were significantly elevated as summarized in Table 1. Influenza polymerase chain reaction (PCR), respiratory viral PCR panel, legionella urine antigen and blood cultures were all negative; however, the COVID-19 PCR assay was subsequently found to be positive.
Laboratory investigations.
| Initial | Discharge | |
|---|---|---|
| Hematological studies | ||
| Complete blood count | ||
| Hb (g/dL) | 11.3 | 13.0 |
| WBC (×109L−1) | 3.2 | 6.7 |
| Platelets (×109L−1) | 116 | 306 |
| Inflammatory markers | ||
| Procalcitonin (ng/ml) | 0.02 | 0.12 |
| Interleukin-6 (ref 0–15.5pg/ml) | 270 | 9.2 |
| C-Reactive protein (ref <5.1mg/l) | 173 | 126 |
| Ferritin (ref 30–400ng/ml) | 678 | 1437 |
| D-Dimer (ref <0.5ug/ml) | 2.84 | 1.75 |
| Lactate dehydrogenase (ref 100–220U/l) | 448 | 285 |
| Biochemistry (mEq/L) | ||
| Serum sodium | 104 | 130 |
| Serum osmolality (mOsm/kg) | 230 | |
| Uric Acid | 3 | |
| Potassium | 4.8 | 4.4 |
| Chloride | 74 | 98 |
| Calcium | 7.8 | 8.7 |
| Magnesium | 1.9 | 1.9 |
| Phosphorous | 2.2 | 2.5 |
| Renal (mg/dl) | ||
| BUN | 12 | 19 |
| Creatinine | 0.52 | 0.8 |
| Hepatic | ||
| AST (U/L) | 28 | 33 |
| Total/direct bilirubin | 0.6 | 1.2 |
| Albumin (g/dL) | 3.4 | 2.8 |
| PT/INR (ref 0.9–1.1) | 1.1 | 1.1 |
| Urine studies | ||
| U. osmolality 9m (Osm/kg) | 693 | |
| Spot sodium (mmol/L) | 58 | |
| Spot potassium (mmol/L) | 17.3 | |
| Spot creatinine (mg/dL) | 86 | |
| U uric acid | 850 | |
Based on the patient's clinical and biochemical data, he was diagnosed with severe symptomatic hyponatremia secondary to syndrome of inappropriate antidiuretic hormone secretion (SIADH) in the setting of COVID-19 pneumonia.
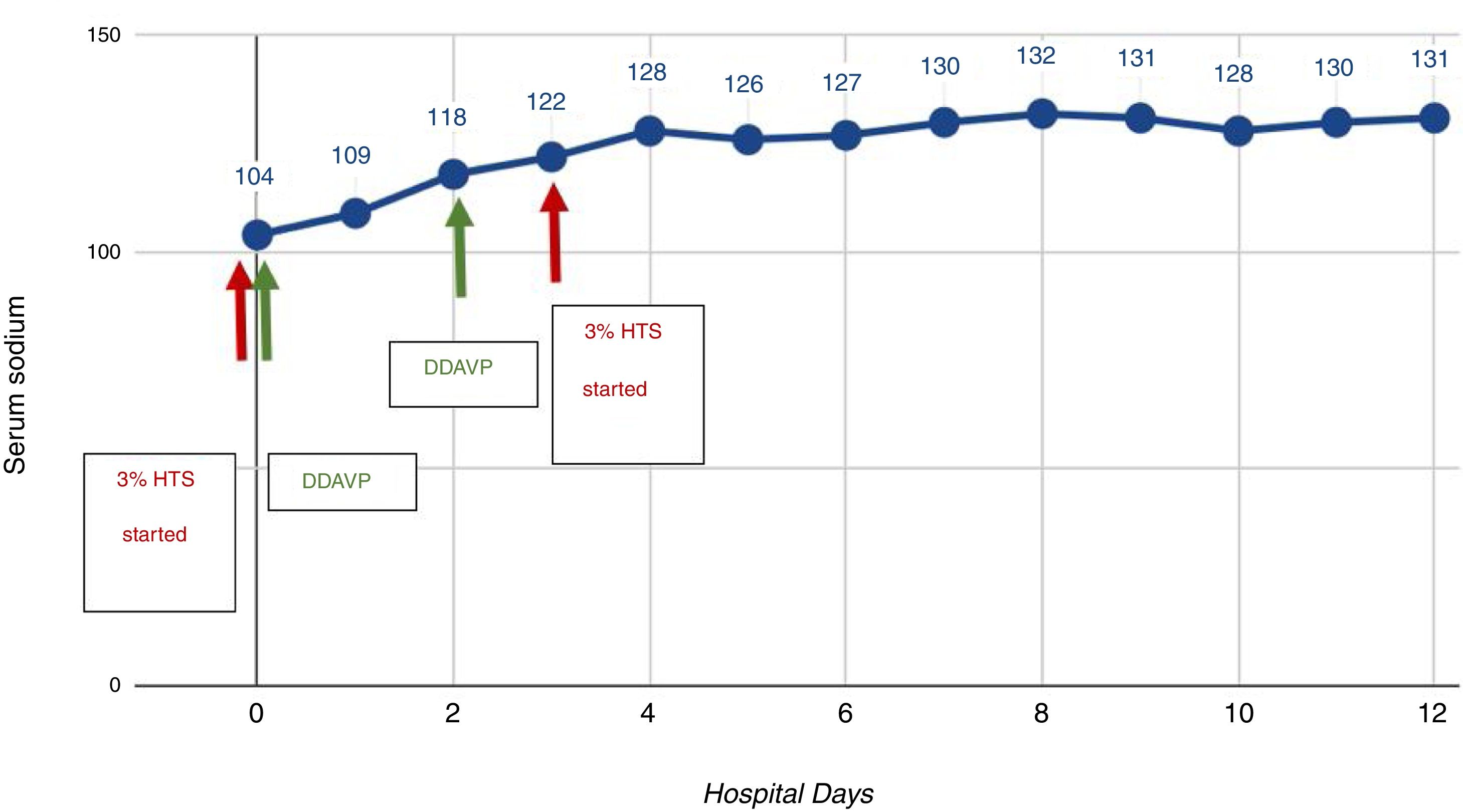
In view of his severe symptoms, 3% hypertonic saline (HTS) infusion was initiated with concomitant fluid restriction. We utilized a pro-active DDAVP strategy (DDAVP 2mcg iv q8h as needed) to minimize overcorrection in the setting of his high risk of osmotic demyelination. He demonstrated a dramatic clinical recovery with symptom resolution and normalization of sodium on day 4 of hospitalization as indicated in Fig. 1. The remainder of his hospital course was unremarkable.
The rapid rise and spread of COVID-19 in the US have posed a significant challenge to the healthcare system. At this time, understanding of its clinical presentation is largely based on data from China and Singapore. A meta-analysis of nearly 46,000 patients indicates that upper respiratory and flu-like symptoms predominate with less common complaints including headache, dizziness, abdominal pain, anosmia, diarrhea, nausea, and vomiting.2 In this paper, we present the first report of COVID-19 related SIADH presenting as new onset seizures in the absence of fever or overt respiratory symptoms.
SIADH in the setting of pneumonia has been extensively studied and reported. Several potential mechanisms have been postulated including extensive cytokine release, hypoxemia, nausea and stress.3 Additionally, inflammation (IL-6 in particular) itself has been reported to directly impair osmoregulation leading to hyponatremia.4
Increasingly evidence indicates a propensity for hyper-inflammation and cytokine release with COVID-19 infections.5 This has manifested as Acute respiratory distress syndrome, myocarditis and overt cytokine storm which are becoming increasingly well recognized associations.
We hypothesize that milder forms of hypercytokinemia and hyper-inflammation could result in a number of less dramatic atypical presentations including SIADH. Elderly populations are particularly susceptible due to impaired free water excretion and late recognition of symptoms. A high index of suspicion and awareness of this association is essential to mitigate SIADH related complications as cases of COVID-19 continue to rise.