To the Editor,
Preeclampsia is a common complication of pregnancy (3%-10%) which is defined by the development of high blood pressure and proteinuria beginning at week 20 of the pregnancy. It is associated with a number of factors: family history, thrombophilia, diabetes, etc.1,2
With this in mind, we present the case of a 33 year old patient with a history of pulmonary thromboembolism, testing negative for blood clotting disorders (including lupus anticoagulant and anti-cardiolipin) but presenting a heterozygous deficiency in methylenetetrahydrofolate reductase enzyme gene (C677T) who developed partial HELLP syndrome during week 34 of gestation. The treatment approach consisted of administering hydralazine and alpha-methyldopa, and in the end, an emergency caesarean section. However, clinical resolution was only partial (with residual proteinuria of 113mg/dl in 24 hour urine sample).
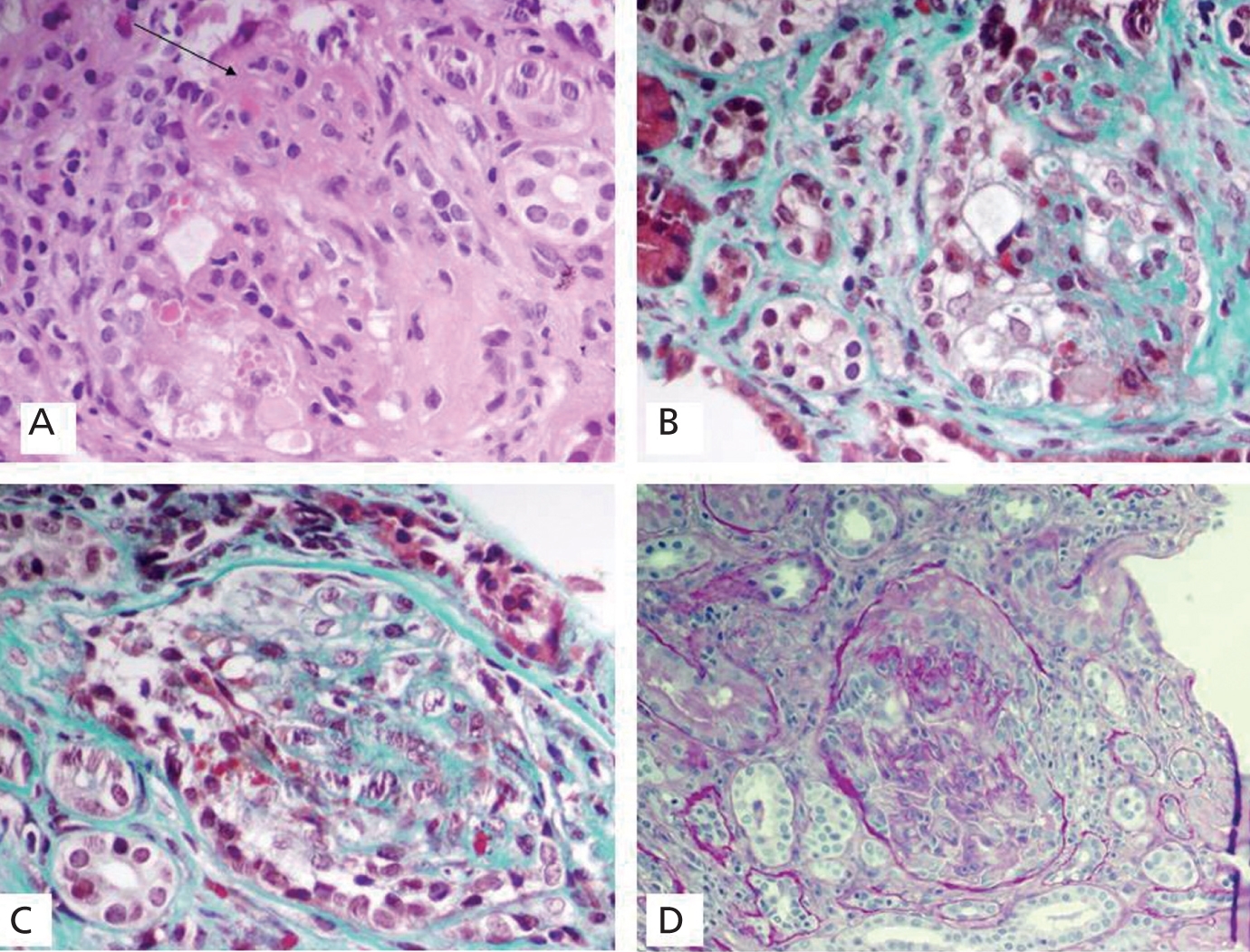
Four months later (during the lactation period), the patient suffered a new episode, characterised by inflammation in both ankles, hypertension and decreased renal function with no oliguria (urea 145mg/dl, creatinine 4.3mg/dl) and was then admitted in the nephrology department. Relevant test results were haemoglobin: 9.5g/dl; albumin: 4.3g/dl; microhaematuria; and proteinuria of 125mg/dl. The immunology study showed that she was positive for antinuclear antibodies (ANA 2.02 at titres of 1:80) with normal anti-DNA antibodies, antihistone antibodies and a complement levels. Anti-cytoplasmic antibodies (ANCA) were positive at low titres (26.4U/l) with anti-myeloperoxidase specificity (ANCA-MPO). However, the patient's condition started to improve spontaneously under conservative treatment, which allowed us to delay the renal biopsy until after the lactation period. The subsequent histopathological study described sclerosis in 40% of the sample, with obliteration of capillary lumens due to mesangial proliferation and endotheliosis, increase in mesangial material and capsular adhesions. Parietal epithelial cells were especially prominent and formed fibrous epithelial crescents in 4 glomeruli (30% of the sample). On the other hand, podocytes were very swollen with numerous protein reabsorption droplets. Predominantly lymphocytic inflammatory deposits and mild focal fibrosis were observed in the interstitium. Immunofluorescence revealed small diffuse deposits of IgG and C3 located in the mesangium with an intensity of 1+ (Figure 1).
Based on these data, we prescribed combination therapy with prednisone 1mg/kg/day and azathioprine 2mg/kg/day. Progress remained favourable; anaemia was corrected and renal function returned to normal levels (urea 41.2mg/dl, creatinine: 1mg/dl), as did autoantibody levels. However, the 24 hour urine test still revealed microhaematuria and proteinuria (203.5mg/dl). In order to screen for a possible pulmonary disorder, which is common in microangiopathies, pulmonary function tests were performed which showed decreased alveolar diffusion due to the capillary action.
Lastly, we re-considered the definitive diagnosis for this case based on the following premises: lack of criteria sufficient to indicate lupus or microscopic polyangiitis; self-limiting renal disease; lack of immunological specificity (concomitant presence of ANA and p-ANCA); histological changes partially compatible with preeclamptic damage (such as endotheliosis, mesangial proliferation and even interstitial fibrosis); and most of all, the course of the disease being related to childbirth.3 The final diagnosis was drug-induced p-ANCA vasculitis in conjunction with toxaemia. In this case, systemic symptoms may have been related to prior intake of hydralazine and/or methyldopa. In addition, its episodic nature fully coincides with the autoimmunity-promoting effect described in the literature for both drugs; in the case of hydralazine, this also seems to be linked to the development of some types of pulmonary-renal syndrome and ANCA-positive pauci immune glomerulonephritis.4,5
Conflicts of interest
The authors affirm that they have no conflicts of interest related to the content of this article.
Figure 1. Renal Biopsy. Preeclamptic lesions and fibrous crescents