Antecedentes: La enfermedad renal crónica (ERC) se entiende actualmente como un importante problema de salud pública global, que requiere una nueva aproximación. Objetivos: Mostrar los resultados de la implantación de una consulta de rápida resolución para el manejo de la ERC. Métodos: Se han analizado de manera retrospectiva los resultados obtenidos durante un período de seis meses, entre septiembre de 2011 y febrero de 2012. Las variables estudiadas han sido la edad de los pacientes, el origen de las propuestas, la causa de las remisiones, el destino inicial dado a estas y el destino final de los pacientes. Resultados: Un 9,61 % de las propuestas recibidas se ha remitido a Atención Primaria sin consulta presencial. Un 28,05 % de los pacientes han sido evaluados inicialmente en la consulta de alta resolución y un 62,33 % se ha citado directamente para el resto de las consultas. Del 28,05 % inicial, tras el proceso de evaluación, ajuste e información acerca de la enfermedad un 70 % ha sido remitido nuevamente a Primaria para seguimiento, y el otro 30 % se ha citado para su seguimiento en consultas. Por tanto, del total de propuestas se ha seleccionado un 70,65 % de pacientes para seguimiento por Nefrología y un 29,35 % para seguimiento por Atención Primaria. Por otro lado, se ha disminuido la demora para primeras visitas a menos de la mitad. Conclusiones: La consulta de alta resolución se ha mostrado como un instrumento eficiente en el manejo de la ERC. Su implantación ha permitido, consumiendo un mínimo de los recursos asistenciales, seleccionar para seguimiento a largo plazo a aquellos pacientes de mayor riesgo de progresión y cardiovascular pero ofreciendo también una evaluación inicial, ajuste de tratamiento e información a los que serán seguidos por Atención Primaria, y disminuir la demora en primeras visitas de manera significativa.
Background: Currently, chronic kidney disease (CKD) is understood as global important public health problem, a situation that requires a new approach. Objectives: To show the results obtained after implementing a quick resolution consultation for CKD management. Methods: Results were analysed during 6 month time period. Results: A total of 9.61% of received proposals were referred to primary care without in-person visits. In addition, 28.05% of patients were initially evaluated through high resolution clinics and 62.33% were directly referred to other clinics. From the initial 28.05% mentioned, once evaluated, treatment adjusted and informed about the disease, 70% were referred over to primary care for monitoring and the remaining 30% were given specialist appointments. As a consequence, 70.65% of patients were selected for monitoring by nephrology from all proposals received, and 29.35% for primary care monitoring. We observed a significant decrease in the delay until the first medical appointment. Conclusions: Quick resolution consultations demonstrated to be an efficient tool for CKD management. Its implementation allowed both low consumption of health care resources, selected patients with high risk of progressive cardiovascular disease for long term monitoring, and offered not only an initial evaluation and adjustment of treatment with information provided to those who would be monitored by primary care, but also diminished primary care delays significantly.
INTRODUCTION
Ten years have passed since the publication of the definition and classification of chronic kidney disease (CKD) by the KDOQI group,1 which constituted a revolution in the world of nephrology. During this time period, our field has come to understand the importance of CKD due to its high prevalence,2,3 associated cardiovascular risk,4-10 and economic costs.11-13 In addition, the incidence and prevalence of patients on renal replacement therapy continues to increase.14 In this context, CKD is currently perceived as an important global public health issue15,16 that requires a new approach.17-21 We have also learned during these recent years that it is possible to slow progression and reduce cardiovascular risk through early measures.16
The dissemination and application of this classification system has thus produced a clear benefit in the form of detection of CKD in earlier stages than in the past. In turn, this improved detection of CKD necessitates a change in management strategies that involves coordination with primary care providers as an essential component. In this context, several studies and treatment protocols have been published.22-25 In 2007, we published the preliminary results of the implementation of a joint management protocol for CKD between primary care providers and nephrologists in Department 5 of the Health Agency of Valencia.22 In this article, we present the results of a second initiative carried out in order to approach the issue of CKD: quick resolution consultations.
METHOD
The nephrology department of the University Clinical Hospital of Valencia provides 3 consultations 5 days per week (a total of 15 appointments per week), and given the current economic situation and the lack of physical space available in the hospital, it appears unlikely that this number would increase in the near future. In January 2011, coinciding with a partial reorganisation of the medical appointments system, the nephrology quick consultation programme was started, referred to as “quick consultations.” To summarise, one could say that the primary objective of the quick consultation is to select those patients who, due to a low risk of progression, could be treated in the primary care setting following a rapid evaluation process in nephrological consultations, providing information on the disease and adjusting treatments. Quick consultations were started as a trial in September 2010, and as a general protocol in 2011.
The results obtained during a six-month study period (September 2011 – February 2012) were retrospectively reviewed and analysed after consultations had been consolidated. The study variables included patient age, origin of the requests for consultations, reasons for referral, and initial destination and final destination of each patient (referral to primary care or referral to nephrology for monitoring).
RESULTS
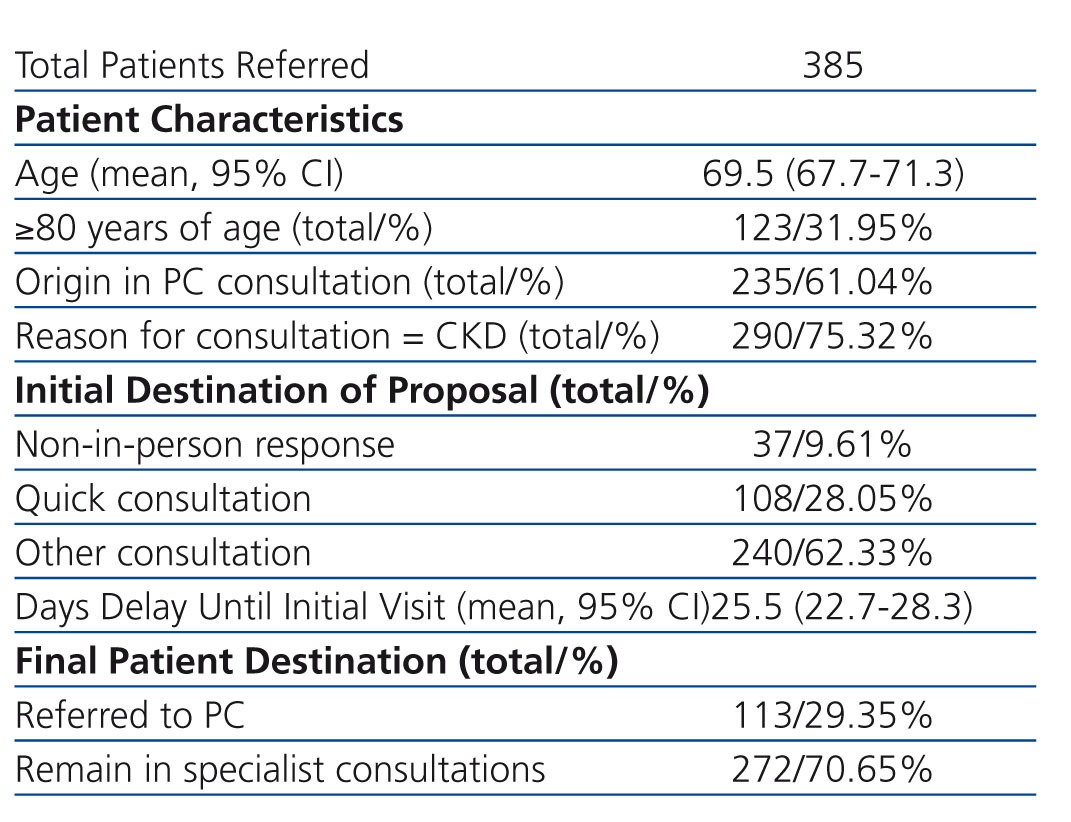
During the six-month study period, a total of 385 requests were submitted for nephrological consultations. Table 1 summarises the primary characteristics of the referred patients, the initial destination for each request, the delay until the first visit, and the final destination of each patient. As shown, the majority of requests were derived from primary care physicians, and the reason for consultations was CKD (stable patients, having previously detected deterioration in renal function) in three-fourths of all cases.
A total of 31.95% of referred patients were 80 years of age or older. Comparing the patients given appointments for a quick consultation to all others, this group comprised older patients: 53% were older than 80 years (vs. 18%).
As regards the destination of the proposal, 9.61% were responded to in the absence of the patient, as a nephrological consultation was not considered to be necessary. These patients did not comply with the criteria for patient referral decided upon for the management of CKD and patients with pathologies whose analysis and follow-up corresponded to other specialties, particularly urology. In addition, 28.05% of proposals were flagged as first visits for quick consultations, and the remaining 62.33% were for other consultations. Of the 108 total first visits carried out in the quick consultation context, 76 (70.4%) were returned to primary care and 32 (29.6%) were passed on to nephrology, considering that these patients could benefit from a short to mid-term monitoring schedule. In this manner, of the total group of initial proposals, 29.35% were returned to primary care and the remaining 70.65% were transferred to nephrology for monitoring.
A mean 25.5 days (95% confidence interval [CI]: 22.7-28.3 days) passed between the patient’s arrival at the hospital and the first visits, and this value was below 31 days for 78% of all cases. We can compare these data with those provided by the hospital during time periods prior to the implementation of the quick consultation programme, although we must keep in mind that the data collection process was not the same for all data sets and so these are not completely comparable. In this manner, the mean wait time in 2008 was 76.5 days, in 2009 was 59 days, and during the nine months prior to the implementation of the quick consultation programme (2010), the mean wait time was 52.1 days.
DISCUSSION
As mentioned, in 2007 we published the preliminary results from the implementation of a joint management programme between primary care and nephrology in Department 5 of the Valencia Health Agency for CKD.22 This department includes two hospitals, a specialty clinic, and 16 basic health zones that attend a total of 357 225 inhabitants.26 The population is quite concentrated, and no distant centres of population are found. The protocol was revised and modified based on the results from this pilot study, in particular the criteria for referral to nephrology after we observed that prior criteria sent too many patients with very low levels of risk for progression to nephrology clinics. In 2010, we again carried out this analysis in order to take into account the novel advancements in the treatment of CKD (target blood pressure values, new anti-diabetics, etc.) and periodically hold meetings between nephrologists and primary care physicians at each health centre in order to disseminate and reinforce the established protocol and to resolve any issues that might arise. The application of this protocol has allowed for organising the flow of patients between primary care and nephrology, unifying and coordinating the treatment of CKD, and establishing better communication between these two specialties. However, despite being reasonably satisfied with the functioning of this programme, we see the same deficiency in the KDOQI guidelines as many other authors,27-36 in the form of an insufficient diagnostic capacity. This issue is accentuated in elderly patients.37,38 In order to address this issue, we created the quick nephrological consultation programme towards the end of 2010, with the following organisational scheme and objectives.
Justification and objectives of the quick nephrological consultation programme
Despite clearly improving the detection and care of this pathology, the current classification and definition system of CKD does not allow for screening for individuals with a greater risk of progression and cardiovascular complications among elderly patients and those in initial stages of disease. Many older patients with mild kidney damage and a low risk of progression are classified in the same stage as individuals at a much higher risk. This tendency to over-diagnose provokes anxiety in the patient and family, since a diagnosis for kidney disease is given in a situation that is not in actuality quite as severe, and also tends to produce referrals to nephrological consultations for patients who, despite complying with the criteria for referral established as a general protocol, will not benefit from hospital monitoring and could be perfectly well attended through primary care. This is exacerbated by the tendency to retain these patients in nephrology clinics once started. Once incorporated into a consultation regimen, many patients remain there sine die, even though their state of stability and low severity of disease could facilitate adequate care through primary care facilities. In order to provide a solution to these issues, a new initiative has been started: “quick” nephrological consultations, whose objectives include:
Functioning of a quick consultation programme
Quick consultations are carried out one day per week (thus consuming only one-fifteenth of the resources destined for nephrological consultations in the department) and provide a double function:
- General organisation of consultations. All proposals are received, evaluated one by one, and separated into rejections, suitable for quick consultations, or distributed among other consultations. In addition, this protocol resolves the issues that appear in setting patient appointments, all activity is monitored, and delays to the system are registered.
- Health care. For this type of appointment, patients are selected primarily for monitoring in primary care after an initial evaluation. These are stable patients with mild-moderate renal pathologies who do not require in-hospital care, or patients whose age and comorbidities would be best cared for in the primary care setting, thus avoiding patient transfers. As such, the population attended in quick consultations is primarily composed of somewhat elderly patients who have been diagnosed with CKD, but who have a low risk of progression. This low risk is estimated based on patient age, comorbidities present, and previous laboratory analyses available through a digital database. These data are suggestive of low risk of progression, stable glomerular filtration rates, and an absence of diabetes or significant proteinuria. We have also observed that this diagnosis often produces a great deal of anxiety for the patient and the patient’s family, especially in the form of doubts regarding entry into a dialysis programme.
Patients are given appointments with a maximum delay of two weeks since receiving the request, although the majority of patients are seen the following week; this is what gives the name “quick consultation.” After the initial evaluation, the patient may:
- Be returned to his/her primary care physician for continued monitoring in this setting. The patient now has the results from an initial evaluation, and if new problems develop in the future, another referral can be processed.
- Be given another appointment in the quick consultation for a second or third evaluation, after requesting diagnostic tests or making changes to treatment regimens, in order to determine the final destination of the patient.
- Be transferred to another consultation based on results from initial consultations that indicate that the patient might benefit from long-term monitoring.
FINAL CONSIDERATIONS AND CONCLUSIONS
Based on the objectives set at the beginning of this project, we believe that they have been met to a high degree. We have improved the general organisation of the consultation system. All proposals and all issues that appear are channelled through the quick consultation system. We have achieved a more ideal system for assigning patients to the different sub-consultations (pre-dialysis, glomerular, general nephrology), grouping certain pathologies such as polycystic kidney disease and oncohaematological renal pathologies into certain offices within the general department of nephrology, allowing for a more in-depth analysis of these specific entities, as well as scientific output derived from the grouping of patients in similar circumstances. We have also achieved a more equitable distribution of workload, thus avoiding overloading certain health care professionals as compared to others. We have observed a decrease (or at least, avoided an increase) in health care workload for other consultations, and the delay until an initial visit has decreased significantly. Approximately 7 out of every 10 patients were returned to primary care for monitoring of renal pathologies, adjusting treatment regimens, and providing information regarding the patient’s disease and prognosis. The remaining patients have passed on for follow-up in other consultations after completing the initial evaluation. We have not performed any surveys, but the majority of the patients that have passed through this programme have expressed their satisfaction with the short wait times and the quality of the health care and information received. In any case, this is a completely subjective description. As regards cost, we do not have specific data, but it would be logical to imagine that costs would decrease, since the total number of patients in follow-up programmes would decrease.
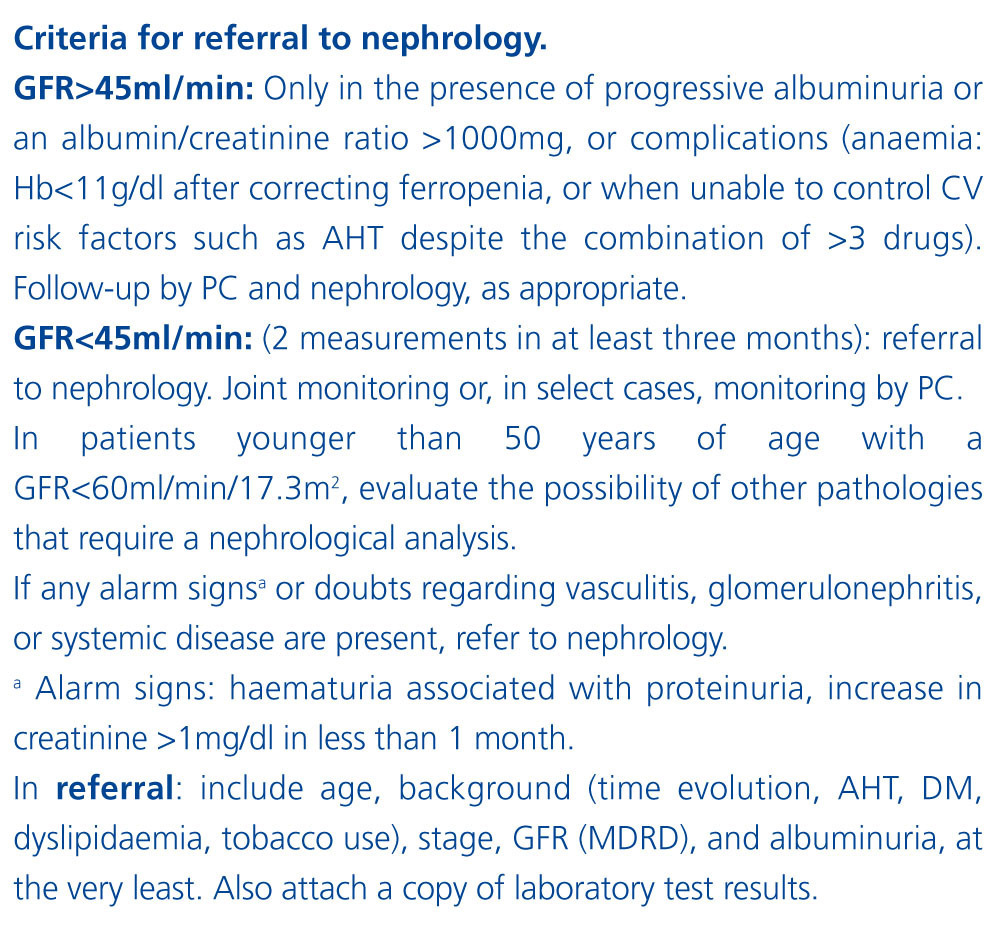
We observed a large proportion of patients referred to the consultation at an age >80 years. It has been shown that many of these patients have a low risk of progression.37,38 In our joint management protocol for CKD, the factors taken into account for referral from primary care to nephrology include estimated glomerular filtration rate and proteinuria, but not age. Figure 1 displays the component of the protocol pertaining to criteria for referral of patients. We believe that some of these patients would benefit from a nephrological consultation, as our experience has shown. In any case, the majority of these patients are seen in quick consultations and the majority of these are returned to primary care for monitoring.
We understand that this is not the only solution to this problem, but we are convinced that CKD is currently a very important public health issue that poses a challenge for health care professionals, requiring a different approach from traditional methods and close coordination between primary care and nephrology for proper management. Another interesting possibility is virtual doctor’s visits, in which information provided by the primary care provider through an online database can be managed by the nephrologist, who can give medical advice as necessary. This system has the advantage of not requiring patients to physically attend nephrology clinics, as well as reducing wait times and costs.25 However, the nephrologist does not obtain the same information and cannot perform an evaluation of the same quality and scope as in a visit in person to the clinic. It is also impossible for the nephrologist to maintain an independent database on these patients, instead relying on primary care physicians for all information. The choice of one system or another (or a combination of both) should be made on an individual basis and adapted to the situation in each department or health area, primarily based on the available resources, population attended and its geographical distribution, and the availability of a single, joint digital information system shared by primary care and medical specialties. In any case, we believe that it is essential to detect patients with a low risk of progression, selecting them for monitoring in primary care while also ensuring proper treatment and provision of information regarding their disease.
To conclude, we can affirm that quick resolution nephrological consultations have been shown to be an efficient tool for approaching the issue of CKD. The implementation of such a programme has allowed for minimising the consumption of hospital resources, screening a good deal of the referred patients, selecting certain individuals with a relatively high risk of progression and cardiovascular issues for long-term monitoring, and still providing an initial evaluation with adjustments to treatments provided and information given followed by monitoring in the primary care setting, while also significantly reducing the wait time until being attended at an initial consultation. Of course, there may be other approximations for reaching these same goals, but this method has been shown to work well and adapt to the realities of our department.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. Summary results
Figure 1. Criteria for patient referral from primary care to nephrology