El dolor es un síntoma muy prevalente en hemodiálisis, pero pasa frecuentemente inadvertido. Los escasos estudios sobre el dolor en diálisis hacen únicamente referencia al dolor crónico. Para conocer las características del dolor intradiálisis y las del dolor crónico fuera de diálisis, se administraron diversas escalas de medición validadas, a un grupo de 27 pacientes en hemodiálisis: la Escala Visual Analógica, el Pain Management Index, el McGill Pain Questionnaire, y el Brief Pain Inventory, primero durante la sesión y posteriormente fuera de la misma. La etiología más frecuente del dolor intradiálisis fue la de tipo isquémico, y la del dolor crónico el musculoesquelético. La prevalencia del dolor intradiálisis fue mayor. El valor medio de la escala visual analógica fue ligeramente superior en el dolor intradiálisis. El valor medio del Pain Management Index fue superior en el dolor crónico. El McGill Pain Questionnaire mostró valores similares en ambas situaciones. Sólo en el dolor crónico el tiempo de permanencia en diálisis se relacionaba con la escala visual, el índice cualitativo total y el número de palabras escogidas, y los niveles de PTHi con la escala visual y la interferencia con el desplazamiento. Recibieron analgesia el 11% de pacientes para el dolor intradiálisis, y el 74% para el dolor crónico. Se concluye que el dolor en diálisis es muy frecuente y su manejo resulta inadecuado, y que las escalas utilizadas se han mostrado útiles para evaluar el dolor en diálisis. Respecto al dolor intradiálisis, el dolor crónico se muestra menos prevalente e intenso, mejor tratado, mayoritariamente de origen musculoesquelético y relacionado con el tiempo en diálisis y el hiperparatiroidismo.
Pain in haemodialysis is very common, although frequently underdiagnosed. Chronic pain in dialysis has been scarcely evaluated, and intradialytic pain has not been specifically analyzed. Our aim was to compare intradialytic versus chronic pain characteristics in the same group of twenty-seven hemodialyzed patients, to investigate whether there were or not differences between them. Several validated scales were used: a) Analogical Visual Scale, defines pain intensity from 0, no pain, to 10, the worst pain; b) Pain Management Index, that results from subtracting pain level from analgesic use, ranging from – 3 (inadequate) to + 3 (adequate management); c) McGill Pain Questionnaire, which defines three items: pain related qualitative index, number of words chosen, and present pain intensity; and d) Brief Pain Inventory, which analyses influence of pain in patient’s life, was only aplicable to evaluate chronic pain. Tests were administered firstly during the dialysis session for evaluating intradialytic pain, and another day out of the session to evaluate chronic pain. Ischemic pain was the most common during the session (37%), whereas muscle-skeletal was more frequent out of the session (77%). Prevalence of pain was higher during the session (92.5% vs 77.7%, p <0.05). Number of weekly sessions with pain was 1.78 ± 1.2. Analogical visual score was slightly higher during the session with respect to chronic pain (3.28 ± 2.22 vs 2.67 ± 2.13, p = NS). Pain Management Index scores were significantly different (intradialytic: -0.81 ± 0.76, chronic pain: -0.12 ± 0.94). McGill test scores were similar in both situations. Only in chronic pain, time on dialysis correlated significantly with analogical visual scores, pain related index and number of words chosen, and parathyroid hormone levels with analogical visual scores and interference to displacement score from Brief Pain Inventory. Farmacological treatment was prescribed in 11% of patients with intradialytic pain (63.1% of responders) compared to 74% for those with chronic pain (53.1% of responders). In conclusion, pain in hemodialysis is very frequent and becomes undertreated. Pain scales used have been shown to be useful in this setting. Several differences appear between intradialytic and chronic pain. Chronic pain is less frequent and intense, better treated, mainly derived from a muscle-skeletal source, and it is related to time on dialysis and to secondary hyperparathyroidism.
INTRODUCCIÓN
Pain is one of the most significant public health issues affecting society today, generating concern for both public health system users and professionals. It is the most common reason people consult health care practitioners and is associated with high health care and social costs.1 It manifests itself as an unpleasant emotional experience, an activity linked with perception that is the result of a complex process formulated by the individual, involving sensory input and psychological, social and cultural variables, making this a unique and personal experience. Often there is no correlation between the stimulus or the damage that occurs in the tissue and the level of suffering expressed by the individual experiencing it, which highlights the multidimensional nature of pain2 and the importance of taking all these factors into consideration when studying and assessing this concept.
In recent years, several studies have been published in the field of haemodialysis and kidney transplants on the quality of life of patients. Pain is highly prevalent in this field and its negative impact on the quality of life of those it affects is evident.3,4 However, there is very little literature that refers to the characteristics of pain affecting haemodialysis patients. A Canadian study5 described how 50% of haemodialysis patients experienced pain. It also observed that very few patients were given analgesic treatment to control the pain. Greater access to haemodialysis therapy, the fact that the population of haemodialysis patients is ageing and the increased duration of dialysis in part, may explain why haemodialysis patients are regularly experiencing pain, in particular chronic pain. It is accepted that pain is an inevitable part of life for haemodialysis patients. Symptoms like headaches, muscle cramps and other less specific complaints are common in haemodialysis units. Arteriovenous fistulas may cause ischaemic or neuropathic pain, and complications associated with venous catheters may also be a source of pain. Moreover, there are chronic complications associated with haemodialysis like ischaemic diseases, neuropathies and renal osteodystrophy, among others, that may also be a source of chronic pain for these patients. There are no studies that separately analyse the pain experienced by patients during the dialysis session and the chronic pain they feel outside the session. Pain assessment for dialysis patients can be quite vague since there are no instruments specifically designed for identifying the needs of these patients. In studies carried out over the last few years5,6 scales and questionnaires that have been validated for other disciplines, especially the palliative care of terminal cancer patients, have been used.
The aim of this paper is to describe the pain experienced by haemodialysis patients during the session (intradialytic pain) and outside the session (chronic pain) in order to evaluate whether there are any differences between the two. The prevalence, severity, aetiology, location of pain and pain management as well as its impact on the life of patients was analysed by applying different validated questionnaires and scales used in assessing pain in cancer patients.
MATERIAL AND METHODS
This was a descriptive, cross-sectional study which included all patients that received haemodialysis for more than one month in our Haemodialysis Unit (n = 38). Patients who voluntarily decided not to take part in the study (n = 4) and those who were unable to respond correctly to the questionnaires because of mental or intellectual impairment were excluded (n = 2). Similarly, patients whose full assessment records were not available because of death, transfer to another region or transplant during the study period were also excluded (n = 5).
Finally, 27 patients, 13 of which were men and 14 women, whose average age was 66 ± 13.6 (m ± sd) and who received haemodialysis during a period of 66.4 ± 61.3 months were analysed. The pain rating scales were applied to all these patients in the first phase of the study during the dialysis session, and again afterwards outside the session. This is carried out outside the dialysis room during an outpatient’s appointment. Before using the different scales, the patient was asked whether they were experiencing pain or not. If the answer was no, the patient was told that that corresponding Visual Analogue Scale (VAS) score should be 0 (no pain). If the answer was yes, then the pain was classified using the rest of the instruments. In order to do this the patient had to be able to locate, describe and grade the pain they were referring to. The scales described in this study were applied to patients who experienced pain.
Firstly, the VAS was applied to evaluate the intensity of the pain experienced at the moment which ranged from “no pain” to “unbearable pain”. The patients moved the scale themselves to the point that represented the pain they were feeling, and this corresponded to the numbers on the back that ranged from 0 (no pain) to 10 (maximum pain). Three VAS evaluations were carried out on each patient during the final hour of haemodialysis, during the first, second and third weekly session in three consecutive weeks. The mean value obtained was then calculated. All the VAS assessments were done by the same interviewer. The VAS that is included in the McGill questionnaire was used to assess pain outside the session. The VAS has been validated for chronic and experimental pain.7,8
Secondly, the Pain Management Index (PMI) was calculated according to the descriptions in the literature.9 Values were then assigned according to the level of analgesia provided: 0 indicates no prescribed analgesics; 1. non-opioid analgesics; 2. weak opioids; and 3. strong opioids. The absence of pain received a score of 0, mild pain 1, moderate pain 2 and intense pain 3. The PMI is calculated by subtracting the level of pain from the level of prescribed analgesia in order to obtain values ranging from -3 to +3. Negative PMI scores indicate inadequate treatment and 0 and positive scores indicate a more acceptable level of treatment. The PMI is a scale that has been validated for assessing pain in cancer patients.9
Afterwards, patients were given a validated pain questionnaire, the McGill Pain Questionnaire (MPQ),10 which evaluates the quantitative and qualitative aspects of pain like the location, grade, temporal characteristics and intensity. The patient chooses from a long list of words that describe different types of pain and define the subjective experience of the pain felt. These words are grouped together in several categories which form four large groups: sensory, affective, evaluative and miscellaneous. Seventy-eight words were included in the original version, although different validated versions may vary. The Spanish version contains 66 words.11 Three scores are obtained from this questionnaire: - Number of Words Chosen (NWC): total number of words describing the pain chosen by each patient. - Pain Rating Index (PRI): the score obtained by assigning corresponding values to each possible answer (these are in order of increasing intensity), and adding the points of the words chosen by the patient. - Present Pain Intensity scale (PPI), which the patient should use to grade their pain as anything from “mild” (1 point) to “unbearable” (5 points).
Given its complexity, the MPQ was applied by an interviewer that read the questionnaire instructions to the patient and answered any questions regarding terms that were difficult to understand. All the questionnaires were applied by the same interviewer and completed during the haemodialysis session and outside of it. The higher the questionnaire score, the more intense the pain and the greater the subjective perception of the harmfulness of the pain.
The fourth scale used was the Brief Pain Inventory (BPI), which is a tool that was only used for assessing chronic pain outside the session. It explores the main characteristics of pain like intensity, location, impact on daily life, psychological distress, impact on social isolation and relationships. This scale has been validated for patients with neoplasias and other diseases.12 The validated Spanish version has also been published.13 This scale, which has been recommended by the European Association for Palliative Care,14 is mentioned in the clinical guidelines for pain relief in cancer patients published by the WHO15 and has also been validated for patients experiencing other types of pain.16 Its general use for rating pain has also been established.17 The higher the score obtained in this scale, the higher the level of pain experienced by the patient.
All these scales have previously been used to assess pain in haemodialysis patients.5
Apart from the questionnaires, other specific data related to the pain experienced only during haemodialysis was collected, like temporal characteristics of pain during the session and the number of sessions during which pain was felt. Compliance with treatment was assessed in an interview with the patient and non-compliant patients were those who did not adhere to the prescribed analgesic treatment.
STATISTICAL ANALYSIS
The statistical analyses were carried out using the Graphpad Prism programme version 2. The results are expressed as the mean ± standard deviation. The demographic variables and other factors like duration of dialysis, cause of pain, primary kidney disease and different comorbidities were hypothesized to potentially influence the different pain measurement scales. The comparison of the independent groups was carried out using the Student’s t-test or the Mann-Whitney U test as necessary. Spearman’s rank correlation coefficient was calculated. P-values of <0.05 at both ends were considered statistically significant.
RESULTS
Patient profile and prevalence of pain
Patient characteristics can be found in table 1. Patients were most commonly over 65 years old, married and suffering from diabetes and high blood pressure. The average of the three VAS scores during the dialysis session was 0 in only two cases (7.4%) (patients who felt no pain), and was above 0 for the rest (92.5% of patients experienced intradialytic pain). The prevalence of pain outside the session was significantly lower (77.7%, p < 0.05). The number of days per week with pain was 4.75 ± 2.5, which was mainly experienced during the day (43.7%) or during the day and night (34.3%). The number of painful weekly sessions was 1.78 ± 1.2. The duration of the pain was less than one hour in 55% of cases and lasted the whole session in only 15% of cases.
Causes and location of pain
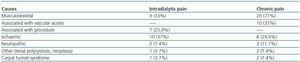
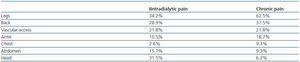
The causes of pain can be found in table 2. During the session, ischaemic pain, pain associated with the procedure and musculoskeletal pain were most prevalent (approximately 30% each). Pains associated with the procedure included cramps, headaches and pain relating to vascular access. By contrast, outside the session pain was predominantly musculoskeletal. Several sources of pain were identified in some patients: in three patients (11.1%) during the session and in thirteen patients (48.1%) outside the session. Table 3 shows the distribution of the locations of pain. Pain, in particular chronic pain, was most commonly located in the legs.
Severity of pain and pain management
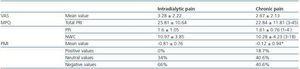
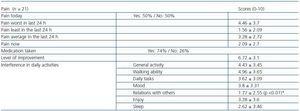
The scores of the different scales applied can be found in tables 4 and 5. The intensity of intradialytic pain was slightly greater although it was not statistically significant. A high percentage of patients (74%) took analgesics and 53.1% noticed a significant improvement in pain. Of the daily activities, the one that was least affected by pain was relations with others (p < 0.05), compared with general activity and walking ability.
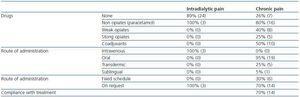
The medication given to patients can be found in table 6. The percentage of patients that took analgesics for chronic pain was much higher (74 compared with 11%). A placebo was not administered to any of the patients. Intravenous paracetamol improved pain in 63.1% of cases. Most patients with chronic pain who were taking analgesics were being treated with paracetamol. Some of them were taking weak opiates (tramadol or codeine), and a small percentage were taking strong opiates (buprenorfine). The use of coadjuvant medication (sertraline or gabapentin) was recorded in half the patients.
Relationships between the different variables
Intradialytical pain. There was no correlation between the different comorbidities analysed, age, sex, duration of haemodialysis, analytical variables and any of the scales used to measure pain during the session.
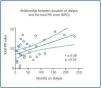
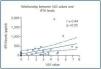
Chronic pain. There was no correlation between patients’ clinical characteristics and the different pain rating scales, except for duration of dialysis which correlated with the VAS score (r = 0.36, p <0.05), total PRI (r = 0.38, p < 0.05, figure 1) and the number of words chosen in the MPQ (r = 0.39, p <0.05). Similarly, plasma iPTH levels were associated with the VAS score (r = 0.44, p < 0.05, figure 2), total PRI (r = 0.32, p = 0.05), and interference with walking ability from the BPI (r = 0.35, p < 0.05).
DISCUSSION
Our study shows a high prevalence of pain experienced by haemodialysis patients, particularly during sessions (92.5%), but also outside of them (77.7%). This data supports the findings of numerous studies5,6,18,19 that present pain as a common and generalised symptom that affects the daily lives of both dialysis patients and health care professionals, although before this study such a high percentage of cases had never been described, particularly during the dialysis session. Other studies on pain during haemodialysis indicate a prevalence of between 3720 and 50%,5,21 which is similar to the prevalence of chronic pain among the general population, which ranges between 29.6 and 50%, according to different studies,22-25 although the variability of dialysis pain is very wide (between 8 and 82%).18 The varying characteristics of the populations selected in the different studies (age comorbidity, geographical location), as well the different methodology used, may explain this variability to a certain extent.
With regard to causality, a high percentage of patients experienced musculoskeletal pain, which was the most common type of chronic pain found in this and other patient series,5,26 and even among the general population.27 Ischaemic pain and pain associated with the procedure during the session was also recorded. This study was intended to be sensitive to dialysis pain and its findings may be the most accurate in reflecting the influence that the time chosen to collect data has on results. A previous study5 describes a lower percentage of patients with this type of pain, possibly because of the different methodology used which involved patients filling out the questionnaires themselves at home instead of during the session and with the help of an interviewer, as was the case in our study. As a result, the setting in which the information is collected is a factor that could potentially influence the patient’s response, which would justify further research aimed at standardising the methodology used to assess pain experienced by dialysis patients.
Another characteristic that was evaluated was pain intensity, which was similar both during dialysis and outside of it with the vast majority of patients reporting mild to moderate pain. Unlike other studies5 in which up to 55% of cases patients describe the pain as severe (VAS > 7.5), in our study only 7.8% of patients experienced intense pain during the session and none did outside the session. These percentages are more similar to levels of intense pain recorded among the general population which range between 1 and 14%.27,28 This difference in part may be attributed to the method used to obtain the data, differences in patient management (the use of medications was greater in our study compared with those already mentioned) or other factors. A statistically significant relationship was observed between the duration of HD and the intensity of chronic pain, as well as with its qualitative characteristics, irrespective of the age and sex of patients. Although these relationships are not referred to in all the studies reviewed, there is data in the literature that indicates similar findings.5 It is logical that prolonged duration of haemodialysis could favour the development of certain diseases like renal osteodystrophy or dialysis-related amyloidosis, which could result in pain. iPTH levels are associated with VAS and MPQ scores, as well as with the increased interference of pain in walking ability, which is one of the variables in the BPI. We did not find any reference to these associations in the literature reviewed. It seems reasonable to accept that hyperparathyroidism could be accompanied by pain that is more intense, has a higher qualitative score and also interferes with patient movement. These findings should be confirmed in future studies.
Another index that was evaluated was the Pain Management Index, which has already been applied to haemodialysis patients5 in other studies and obtained similar results to ours. A significantly higher mean score and percentage of positive values were obtained when this index was used to assess chronic pain. Better treatment of chronic pain was recorded when compared with intradialytic pain. This finding coincides with the high compliance with treatment described. One study described how a yoga-based exercise programme improved pain, fatigue and sleeping disorders affecting haemodialysis patients.29 More studies that evaluate the specific role of non-pharmacological techniques in the treatment of patients with chronic pain should be carried out. Our findings clearly indicate that pain is undertreated during the session, in contrast with the data obtained from a group of patients undergoing treatment for pain caused by metastatic cancer.9 The medication administered was highly effective (63.1% noticed an improvement). The contrast between this data and the PMI score leads us to conclude that very few episodes of pain experienced by our patients were actually detected and treated at that particular moment in time. Health care professionals should adopt a more active approach to detecting pain, which means that they should use instruments for assessment that help them to detect pain before it is mentioned by the patient if they want to establish a personalised programme of treatment and pain relief.
The values obtained with the McGill Pain Questionnaire do not differ from those published in other studies, we were also unable to identify any differences between intradialytic and chronic pain in any of the qualitative characteristics that are analysed in this questionnaire. Therefore, we believe that the application of this evaluative pain rating scale does not appear to be useful for these kinds of patients, within the context of the methodology used in this study. Nevertheless, it may be useful in evaluating the effects of a specific treatment method for pain experienced during dialysis.
Our findings coincide with those of another study5 which did not find any correlation between the results of the different indexes with factors like age or sex and different analytical variables. When it comes to personalising treatment, correlating pain intensity and the cause of pain might be useful in determining analgesic strategy to apply. However, in this study we could not establish any correlation between these factors, perhaps because of the limited number of patients in the sample or the coexistence of various sources of pain in some cases. It would be interesting to explore this subject in more depth using a larger sample of patients.
There are some limitations in this study. On the one hand, it is important to remember that pain is a multidimensional symptom and the psychological aspect plays a very important role in the experience of pain. The relationship between depression and pain has been widely documented in patients with metastatic neoplasias,9 and also in haemodialysis patients,19 however a methodological analysis of this relationship is still beyond our reach. Further studies that shed more light on the subject of dialysis patients are required, and an analysis of the possible role that neuropsychological therapies could have in treating chronic pain is needed, given that the assessment and treatment of chronic pain involves a multidimensional evaluation of all the symptoms that haemodialysis patients experience.30-32
On the other hand, we must emphasise that the instruments used for assessment in this study were not designed specifically for the evaluative needs of haemodialysis patients. These instruments would need to be validated for larger populations of haemodialysis patients and would also need to include patients receiving other renal replacement therapies like peritoneal dialysis and kidney transplant patients. Finally, the results of this study cannot be universally applied to all dialysis patients, given that the sample in this study was limited and involved a very small number of patients from a single centre. Also, this study did not include any control individuals. We must take into account the fact that there is not enough literature on the subject and that new studies that evaluate the use of drugs and other pain control methods are necessary.
In conclusion, despite the advances in recent decades in the field of haemodialysis, haemodialysis patients continue to experience pain in their lives. There is a very high prevalence of pain, particularly during haemodialysis sessions and pain management is inadequate. According to this study, the intensity of pain is mild to moderate, it is felt everyday, particularly during the day and lasts for a prolonged period of time, which limits the patient’s ability to perform certain everyday activities, like walking and affects their general activity. There are significant differences between intradialytic pain and chronic pain outside the session, the latter being less prevalent and intense, better treated, mainly musculoskeletal and associated with the duration of dialysis and hyperparathyroidism. The scales used haven proven to be useful although limited in evaluating pain experienced by these patients. Despite all of this, there is still a long way to go and pain detection and follow up measures need to be introduced in our daily practice. Our approach to this symptom should be analysed in order to achieve optimal pain control for dialysis patients.
Table 1. Characteristics of pain
Table 2. Causes of pain
Table 3. Location of pain
Table 4. Scores from the different scales for patients with pain: VAS, MPQ and PMI
Table 5. Intensity of pain according to the scores of the BPI (chronic pain)
Table 6. Medication taken
Figure 1.
Figure 2.