Content
To the Editor:
Paragangliomas are rare extra-adrenal tumours that emerge from the autonomic nervous system. They are classified as functioning or non-functioning tumours, depending on the production of catecholamines. It presents clinically as high blood pressure associated with vegetative symptoms.
CLINICAL CASE
We report the case of a 20-year-old male who presented with hypertensive emergency that had begun a year before, accompanied by profuse sweating, generalised flushing, headaches and occasionally, lower back pain. Blood pressure reached 230/110mmHg, often triggered by physical effort. A physical examination revealed malar rash and palmar erythema that disappeared with acupressure. Laboratory tests showed an increase in catecholamines and metanephrines in urine at 24 hours: noradrenaline excretion of 7515.77nmol/24h (<504), dopamine of 4298.84nmol/24h (<3237) and normetanephrine of 39676nmol/24h (<2424).
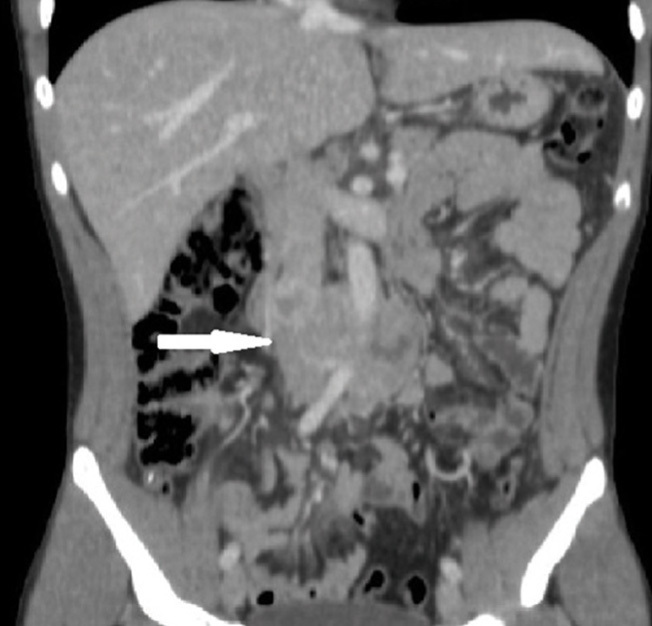
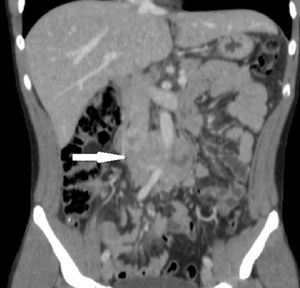
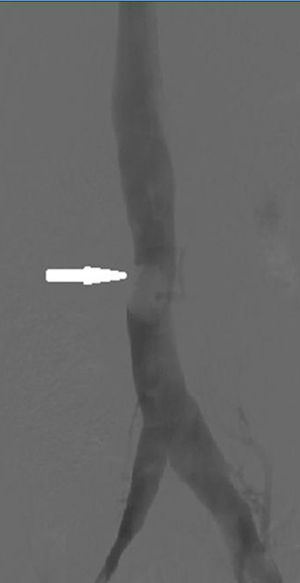
An abdominal ultrasound revealed a retroperitoneal mass of about 8cm of heterogeneous echogenicity and marked vascularisation. Given these findings, a computerised axial tomography (CAT) scan of the abdomen and pelvis was performed that confirmed the existence of a retroperitoneal mass of 8 x 4cm above the aortic bifurcation that infiltrated the inferior vena cava and bordered 180° of the aorta, covering the inferior mesenteric artery (Figure 1). Given the findings of the CAT scan, a cavography was performed to evaluate resectability, revealing an infrarenal intracaval filling defect 2cm in diameter (Figure 2).
Suspecting paraganglioma of the organ of Zuckerkandl, beta-adrenergic blockade was produced and we subsequently performed a surgical en bloc resection of the tumour; we partially sectioned the anterior vena cava to remove the intracaval tumour. The postoperative course was uneventful, the symptoms disappeared and plasma and urine catecholamine and metanephrine levels normalised.
The anatomopathological diagnosis confirmed the suspicion of well-delimited and encapsulated paraganglioma, with a low proliferative index (Ki 67: 5-7%). The patient was referred to the Medical Oncology department, where a 123I-MIBG scintigraphy was requested that showed no signs of residual or distant disease. In the absence of data that justified adjuvant chemotherapy, it was decided to follow up the patient periodically.
DISCUSSION
Paragangliomas are very rare tumours, with an overall incidence estimated at between 0.2 and 0.5 cases per 100 000 inhabitants/year.1 They are extra-adrenal pheochromocytomas that emerge from the chromaffin cells of the sympathetic ganglia located in the retroperitoneum, more commonly near the beginning of the inferior mesenteric artery (organ of Zuckerkandl2) and chest, or the parasympathetic ganglia adjacent to the aortic arch, neck and basal ganglia. They are generally single tumours that are predominant in males between 30 and 45 years of age.
Between 30% and 60% secrete catecholamines and have paroxysmal or sustained hypertension, associated with the classic triad: palpitations, headaches and profuse sweating. Those who do not secrete may have pain or abdominal mass, but they are often found incidentally.3
The diagnosis of functioning paragangliomas is biochemical when they show an increase in plasma and urine catecholamines or metabolites at 24 hours that is two or three times above their normal limit. For the location diagnosis, CAT or MRI is usually performed with sensitivity of around 98%-100%. The 123I-MIBG scintigraphy is very useful in locating extra-adrenal tumours and detecting multiple tumours.4
Proposed criteria for poor prognosis are distant metastasis, vascular or capsular invasion, a high mitotic index, a tumour size greater than 10cm or postsurgical recurrence.5 Retroperitoneal paragangliomas are malignant in 30% to 50% of cases, metastasising in 20% to 42% to areas such as lymph nodes, bone, lung and liver.6 The 5-year survival rate for patients with metastatic paraganglioma is approximately 50%.
Aggressive surgical resection is the treatment of choice, since there is a positive correlation between the possibility of complete exeresis and prognosis. Previously, alpha and beta inhibition was performed (10-14 days) to avoid hypertensive emergency. Surgical resection is also indicated for tumour recurrences. If the tumour is unresectable, the tumour mass can be reduced by chemotherapy or radiotherapy, although these would only be palliative treatments.7
Despite the rarity of paragangliomas, it is important to bear them in mind in the differential diagnosis of high blood pressure, especially in young patients, due to their malignant potential and the effects of catecholamine secretion on the cardiovascular system. Early diagnosis and aggressive treatment are critical in addressing these neoplasms.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Figure 1. Computerised tomography of the abdomen and pelvis (sagittal section)
Figure 2. Cavography