The decision to initiate renal replacement therapy (RRT) implies a wide margin of uncertainty. Glomerular filtration rate (GFR) tells us the magnitude of renal damage. Proteinuria indicates the speed of progression. However, nowadays more than 50% of patients are still initiating RRT hastily, and it is life threatening.
HypothesisBy analysing Emergency Department (ED) frequentation and causes of a hurried initiation, we can better schedule the timing of the start of RRT.
MethodRetrospective and observational study of all CKD patients in our outpatient clinic. ED frequentation and hospitalization (Hos) time were reviewed during a 12-month period. We analyzed: (1) time at risk, purpose (modality of RRT), previous comorbidity; (2) causes of ED frequentation and Hos; (3) type of initiation: “scheduled” vs. “non-scheduled”, and within these “non-planned” vs. “potentially planned”.
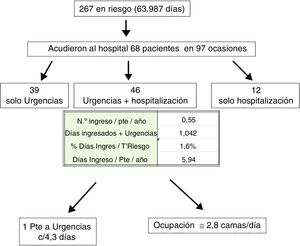
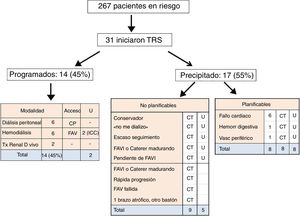
ResultsOf a total of 267 patients (time at risk 63.987 days, 70±13 years, 67% males, 38% diabetics), 68 (25%) patients came to hospital on 97 occasions: 39 only ED, 46 ED+Hos and 12 only Hos. ED frequentation was one patient every 4.3 days, and bed occupation was almost 3 per day. Main causes: 47% cardiopulmonary (1/3 heart failure), 11% vascular peripheral+cerebral, 11% gastrointestinal: 8/11 due to bleeding (all with anticoagulants/antiplatelet agents). Thirty-one (12%) patients initiated RRT: of these, 14 (45%) were scheduled (6 PD, 6 HD, and 2 living donor RTx), and 17 (55%) were not scheduled or were rushed, all with venous central catheter. Following the objectives of this study, the non-scheduled group were itemized into 2 groups: 9 non-planned (initial indication of conservative management or patient's refusal to undergo dialysis, and diverse social circumstances not controllable by the nephrologist) and 8 were considered potentially planned (6 heart failure, one gastrointestinal bleeding and one peripheral vascular complication). This last group (potentially planned), when compared with the 14 patients who started treatment in a scheduled manner, had significant differences in that they were older, with more previous cardiac events, and GFR almost double that of the other group. All of them started treatment in the ED.
ConclusionThis analysis provides us with knowledge on those patients who may benefit from an earlier preparation in RRT. We suggest that patients with previous cardiac events, especially with a risk of gastrointestinal bleeding, should start the preparation for RRT even with GFR rates of 20–25ml/min. In spite of the retrospective nature of this study, and taking into account the difficulties of carrying out clinical trials in this population, we propose this suggestion as complementary to the current recommendations for a scheduled start using this technique.
La decisión de empezar tratamiento renal sustitutivo (TRS) conlleva un amplio margen de incertidumbre. El filtrado glomerular (FG) nos dice la magnitud del daño. La proteinuria, la velocidad de progresión. A pesar de estas premisas, más del 50% de los pacientes continúan iniciando TRS de forma precipitada y con riesgo vital.
HipótesisAnalizando la frecuentación de Urgencias (Urg) y las causas determinantes de un inicio precipitado, podremos programar mejor el momento de iniciar un TRS.
MétodoEstudio retrospectivo, observacional, de la frecuentación de Urg y del tiempo de hospitalización (Hos) de todos los pacientes de la consulta ERCA, durante un período de 12 meses. Se analizó: 1) tiempo en riesgo, destino (modalidad de TRS), comorbilidad previa. 2) Causas de frecuentación de Urg y Hos. 3) Tipo de inicio: «programado» vs. «no programado» y, dentro de estos, «no planificables» vs. «potencialmente planificables».
ResultadosDe 267 pacientes (con un tiempo en riesgo de 63.987 días; 70±13 años; 67% varones; 38% diabéticos), 68 (25%) pacientes acudieron al hospital en 97 ocasiones: 39 solo Urg, 46 Urg+Hos y 12 solo Hos. La frecuentación de Urg fue de un paciente cada 4,3 días y la ocupación de camas fue de casi 3 diarias. Causas predominantes: 47% cardiopulmonar (1/3 insuficiencia cardíaca), 11% vascular periférico+cerebral, 11% digestivo: 8/11 por sangrado (todos con anticoagulantes/antiagregantes). Iniciaron TRS: 31 (12%): de estos, 14 (45%) de forma programada (6 DP, 6 HD y 2 TxR de donante vivo); 17 (55%) no programados o precipitados, todos con catéter venoso. Siguiendo los objetivos del estudio, estos últimos se desglosaron en 2 grupos: 9 no planificables (indicación inicial de manejo conservador o negativa del paciente a dializarse, y circunstancias sociales diversas no controlables por el nefrólogo) y 8 que consideramos potencialmente planificables (6 con fallo cardíaco, uno con hemorragia digestiva y uno vascular periférico). Estos últimos (potencialmente planificables), comparados con los 14 que iniciaron de forma programada, tenían significativamente mayor edad, más eventos cardíacos previos y el FG casi duplicaba al del otro grupo; todos entraron por Urg.
ConclusiónEste análisis nos aporta conocimiento sobre aquellos pacientes que pueden beneficiarse de una preparación más precoz en TRS: proponemos que en los enfermos con eventos cardíacos previos, especialmente con riesgo de sangrado digestivo, se inicie la preparación para TRS aun con tasas de FG de 20-25ml/min. A pesar de la naturaleza retrospectiva del estudio y ante la dificultad práctica de ensayos clínicos en esta población, proponemos esta medida como complemento a las recomendaciones actuales para un inicio programado en esta técnica.
It is well known that early programme for the initiation of renal replacement therapy (RRT) has a favourable impact on the patient's survival.1,2 However, the decision to start RRT implies a wide margin of uncertainty on these patients with a precarious health. It should be kept in mind that starting early may deprive the patient from a period of a time with a good quality of dialysis free. The fact is that it is being debated that early onset improves later survival.3–5 Therefore, the responsible doctor usually faces the difficult balance between starting too early, or too late; requiring a central venous catheter, often with vital risk.
The KDIGO Guidelines6 emphasize the initiation of RRT in symptomatic patients and/or in the presence of a glomerular filtration rate (GFR) of 5–10mL/min. In general, these situations result from late referral to the nephrologist.2,7–9 But this will not be our scenario; now will concentrate in patients being followed in of advanced chronic kidney disease outpatient clinics (ACKD). Usually these patients manifest a subjective feeling of being well, maintain a relatively high urinary output, and are especially reticent to be dialysed. However, frequently an adverse event forces an emergency hemodialysis through a catheter. The KDIGO Guidelines6 present an outline for the risk of end-stage renal disease. However, despite these premises, the proportion of patients who start precipitously and with a venous catheter is very high, around 50%, in most series.10–13 In addition, the DOPPS study reports unscheduled initiation rates with venous catheter between 23 and 70%.14
Our hypothesis is that the analysis of emergencies room visits and the causes that determine a precipitous onset of dialysis may help to optimize the plan to start RRT in a scheduled manner.
The objective of the present study is to analyze retrospectively, the frequency of emergency room visits and their relationship with the precipitated onset in RRT, in patients from our ACKD clinic (monocentric study) during a period of 12 months.
MethodThe study was performed in a ACKD outpatient clinic of a reference Hospital. The centre covers the health care of approximately 400,000 people. Clinical Records are available from 1994 to the end of 2015 from a total of 1,492 patients. The modalities of RRT offered to the patients are hemodialysis (HD), peritoneal dialysis (PD) and kidney and pancreas transplantation (Tx) from living or cadaveric donor. Inhabitants of this region are characterized for a high incidence of early onset of diabetes which has led to a high prevalence of diabetic nephropathy (DN) associated with high cardiovascular comorbidity.1,15–17
The ACKD clinics attend patients with GFR <30mL/min, and other candidates to receive RRT. Most patients come from other outpatient clinics, or after a hospital discharge of cases with potentially irreversible CKD. Patients, who return to dialysis after the loss of the kidney graft, are previously treated in the transplant clinic and they are not included in this study. The patients visit the emergency room or are admitted to the same hospital where patients are being followed as outpatient.
The standard protocols recommended by the Clinical Practice Guidelines are implemented in our clinic. Likewise, we consider important to instruct patients on the adjustment of drugs (diuretics, antihypertensives) both in case of hydrosaline retention and also prevent volume depletion (summer season, gastroenteritis, etc.).1,18 To optimize tracking and adherence to our recommendations, we recommend visits on demand and routine visits which scheduled bimonthly and quarterly and .a telephone number is provided to the patient.
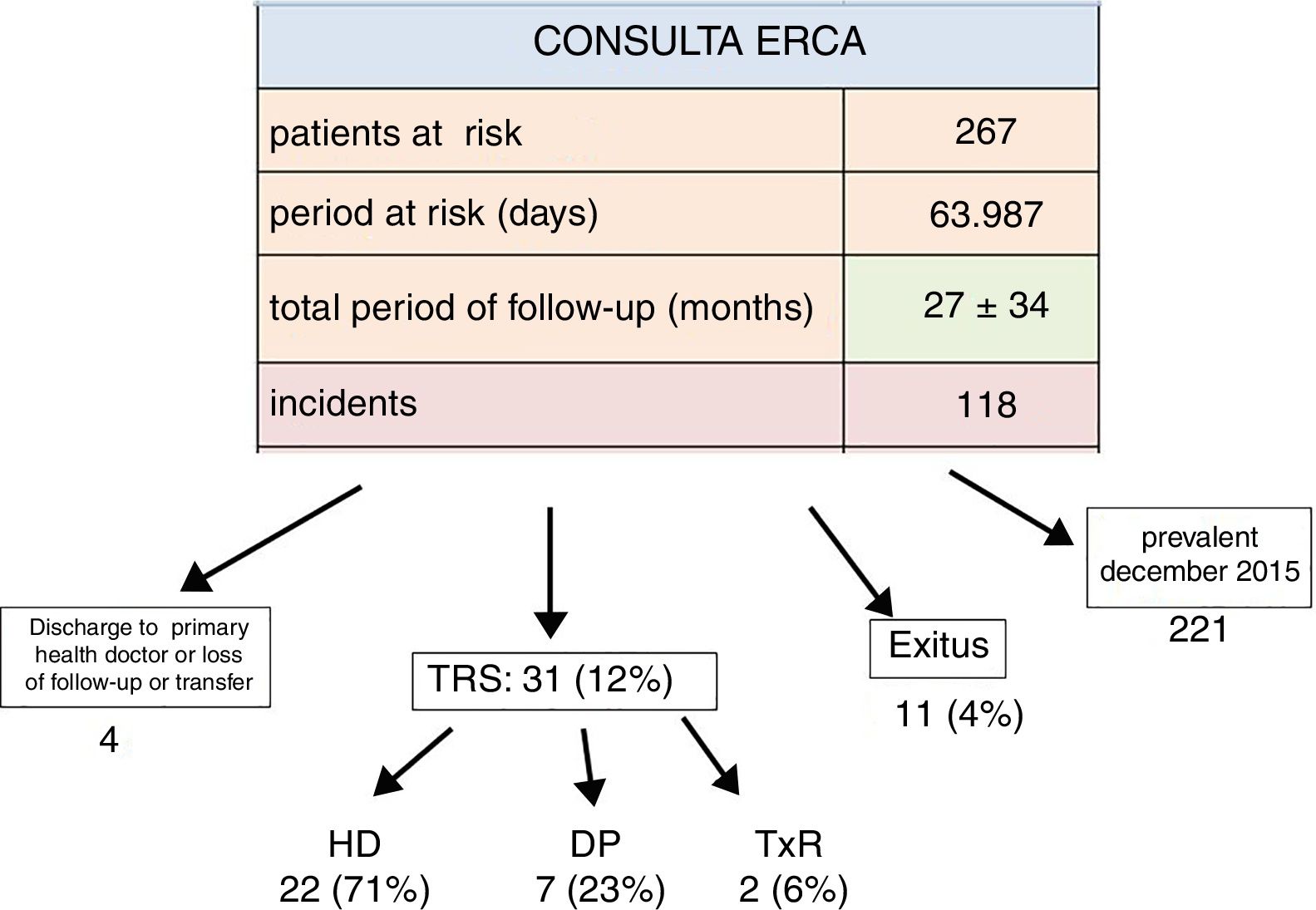
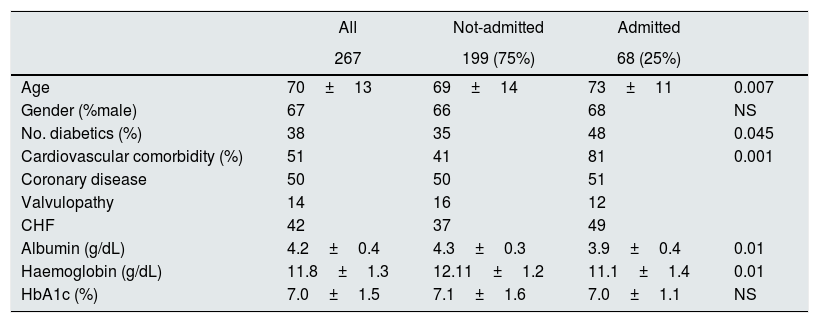
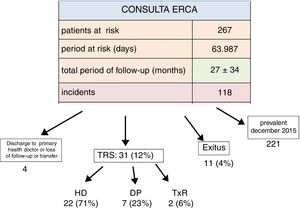
DesignRetrospective, observational and single centre study of the frequency of emergency room attendance and time of hospitalization of all patients of the ACKD outpatient clinic (monocentric study) during a period of 12 months. Fig. 1 shows the number of patients attended in consultation during 2015, the period of time at risk and the outcome during this period. As compared with previous years (only as a reference), we found that the average age of patients was increasing, with more male predominance, and the high rate of ND was maintained as the primary cause of renal disease among incident patients15,16 (Table 1).
Patients at risk and outcomes in the clinic of advanced chronic kidney disease (ACKD) during 2015.
PCD: primary care doctor. LFU: loss of follow-up. RRT: renal replacement therapy. HD: hemodialysis. PD: peritoneal dialysis.
TxR: kidney transplant. Time at risk: period of time in days, when patients are in ACKD consultation during 2015.
General demographic data, cardiovascular comorbidity and relevant biochemical parameters, grouped according to whether they had been in ER or admitted to the Hospital during 2015.
| All | Not-admitted | Admitted | ||
|---|---|---|---|---|
| 267 | 199 (75%) | 68 (25%) | ||
| Age | 70±13 | 69±14 | 73±11 | 0.007 |
| Gender (%male) | 67 | 66 | 68 | NS |
| No. diabetics (%) | 38 | 35 | 48 | 0.045 |
| Cardiovascular comorbidity (%) | 51 | 41 | 81 | 0.001 |
| Coronary disease | 50 | 50 | 51 | |
| Valvulopathy | 14 | 16 | 12 | |
| CHF | 42 | 37 | 49 | |
| Albumin (g/dL) | 4.2±0.4 | 4.3±0.3 | 3.9±0.4 | 0.01 |
| Haemoglobin (g/dL) | 11.8±1.3 | 12.11±1.2 | 11.1±1.4 | 0.01 |
| HbA1c (%) | 7.0±1.5 | 7.1±1.6 | 7.0±1.1 | NS |
CHF: congestive heart failure.
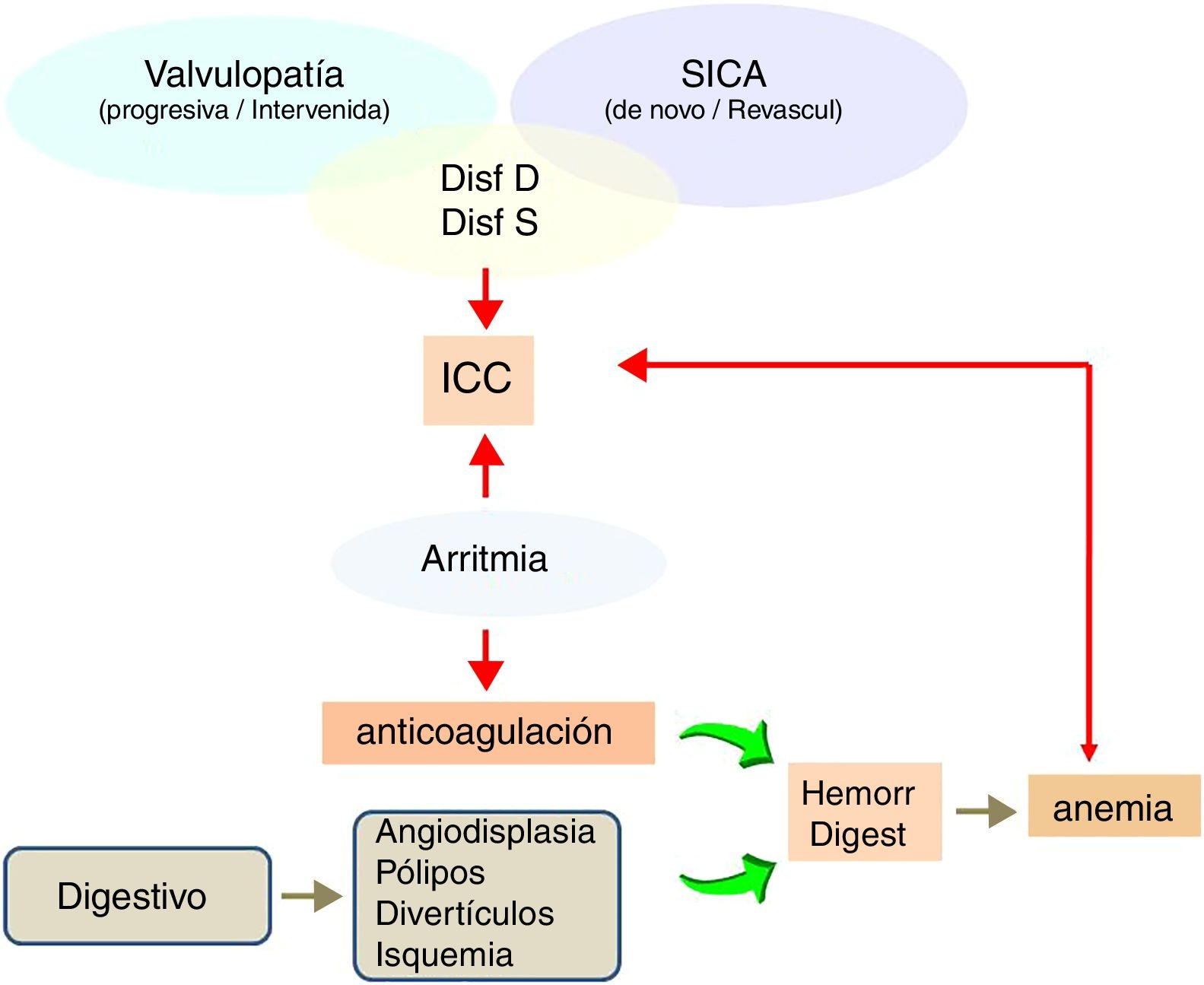
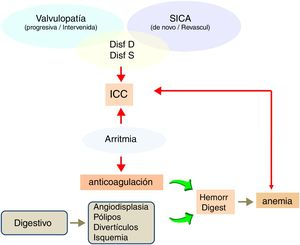
The diagnoses of comorbidity and relevant biochemical parameters were extracted from the patients electronic records. A cardiologist followed up all the patients with previous cardiovascular comorbidity. The diagnoses of congestive heart failure (CHF) was based on clinical data and a previous echocardiography. Also, to assess cardiac function the cardiologist recommended stress or pharmacological tests, and catheterization. The coincidence of several factors was highlighted, often coexisting the diagnosis of arrhythmia, a variable degree systolic or diastolic dysfunction, underlying coronary disease; pulmonary hypertension, and the aggravating effect of previous pulmonary disease (history of smoking, with diagnosis or suspicion of chronic obstructive pulmonary disease). Likewise, the accompanying gastrointestinal pathology (angiodysplasia, diverticula, polyps, etc.), was a clinical concern due to the frequent use of anticoagulants and anaemia due to digestive haemorrhage.
Initiation of RRTPatients were divided into 3 groups: (1) Programmed: they started with access to dialysis or received early TxR, in a planned manner. (2) Not planned: those patients who due to special, social, health or clinical circumstances, were outside the control of a nephrologist, and started dialysis using venous catheter in a precipitated manner. These circumstances are specified in the Results. (3) Abrupt and/or urgent initiation due to clinical events, however that could have benefited from an advance programming in RRT. This is the group of special interest in the analysis of the frequency of emergency room visits.
Emergency Room visitsEmergency frequentation and/or hospitalization was obtained from the electronic records of the hospital.
All patients had a clinical history at admission and clinical evolution, with analytical data and imaging studies. Information collected included the reason to attend the emergency room (ER), the clinical services involved in the care of the patient, the evolution and the final outcome of the patient. The patients were initially assessed by the emergency doctor, and thereafter by the nephrologist and any other specialist.
StatisticsGiven the nature of the study, does not involve a statistical analysis. Only some parameters are described as mean and standard deviation.
ResultsIn Fig. 1 it is highlighted that 31 patients (12%) initiated RRT; and 11 (4%) died. Of these 11 deaths, five occurred during the emergency assistance, four due to cerebral vascular event and one was of cardiac origin.
Frequentation of Emergency Room and HospitalizationIn Table 1 it is shown the basic data of patients at risk during 2015; patients were grouped into those admitted to the hospital at least on one occasion, and those who were not admitted during that period. Sixty eight out of the 267 patients went to the Emergency Room or were hospitalized (25%). These 68 patients visited the hospital on 97 occasions: 50 once, 10 twice, 6 three times, one four and one five times. The patients who were hospitalized were adult, with high proportion of DN and high cardiovascular comorbidity. The values of haemoglobin and albumin were significantly lower in those admitted, but within a range close to normal. The control of diabetes based on HbA1c levels was not different between groups.
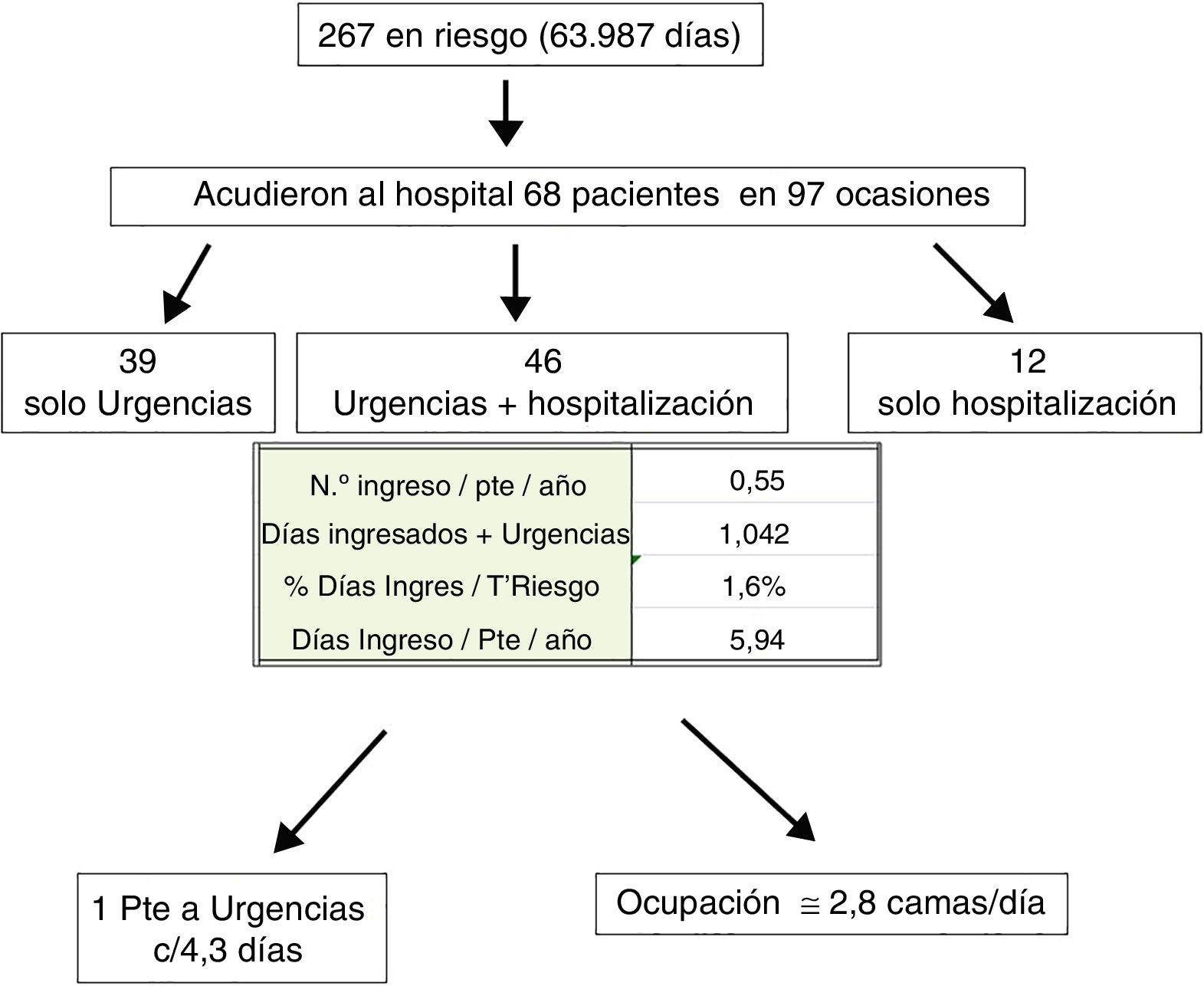
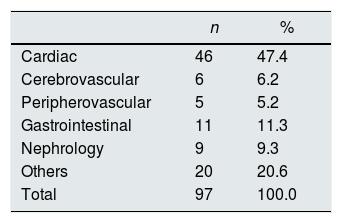
Fig. 2 shows that from the 97 hospital, visits 85 (87%) were to the ER, and 46 (47%) were hospitalized. Twelve patients were hospitalized without going to ER; none of them required RRT during hospitalization.
The visits to ER of this population was one every 4.3 days, which is 1.6% of the time at risk of the patients in medical consultation. Likewise, there were almost 3 hospital beds occupied daily.
The causes of ER frequentation and Hospitalization are described in Table 2. Almost half of the patients had and event of cardiac or cardiopulmonary origin, dyspnoea was the predominant manifestation(67%) (frequently referring to “shortness of breath”), orthopnoea, most cases were grouped under the heading of congestive heart failure (CHF), pulmonary oedema or respiratory failure. All had been included within the so-called cardiorenal syndrome.19 Added to 11 admissions that were due to peripheral or cerebral vascular causes, the hospitalizations of cardiovascular origin reached almost 58%.
Another important cause of admission was gastrointestinal (GI) disturbance, which accounted 11% of the hospitalizations. It is remarkable that 8 were for some type of GI bleeding, all undergoing anticoagulation or antiaggregant therapy. Half of these patients had symptoms of heart failure. Also, there were two other hospitalizations precipitated by cerebral vascular bleeding who were also on anticoagulants.
Nine patients were admitted in the Nephrology service with deterioration of renal function, of which six started dialysis. Some patients were also admitted in “others” speciality wards due to various pathologies and none of them required dialysis.
There was a high percent of patients on anticoagulant/antiaggregant medication; among not hospitalized patients, 65% received anticoagulation/antiaggregant therapy and among hospitalized patients a78% were on anticoagulation/antiaggregant therapy The proportion of those receiving acenocoumarol (Sintrom®) was significantly increased in hospitalized patients (24% vs 11%, p<0.007).
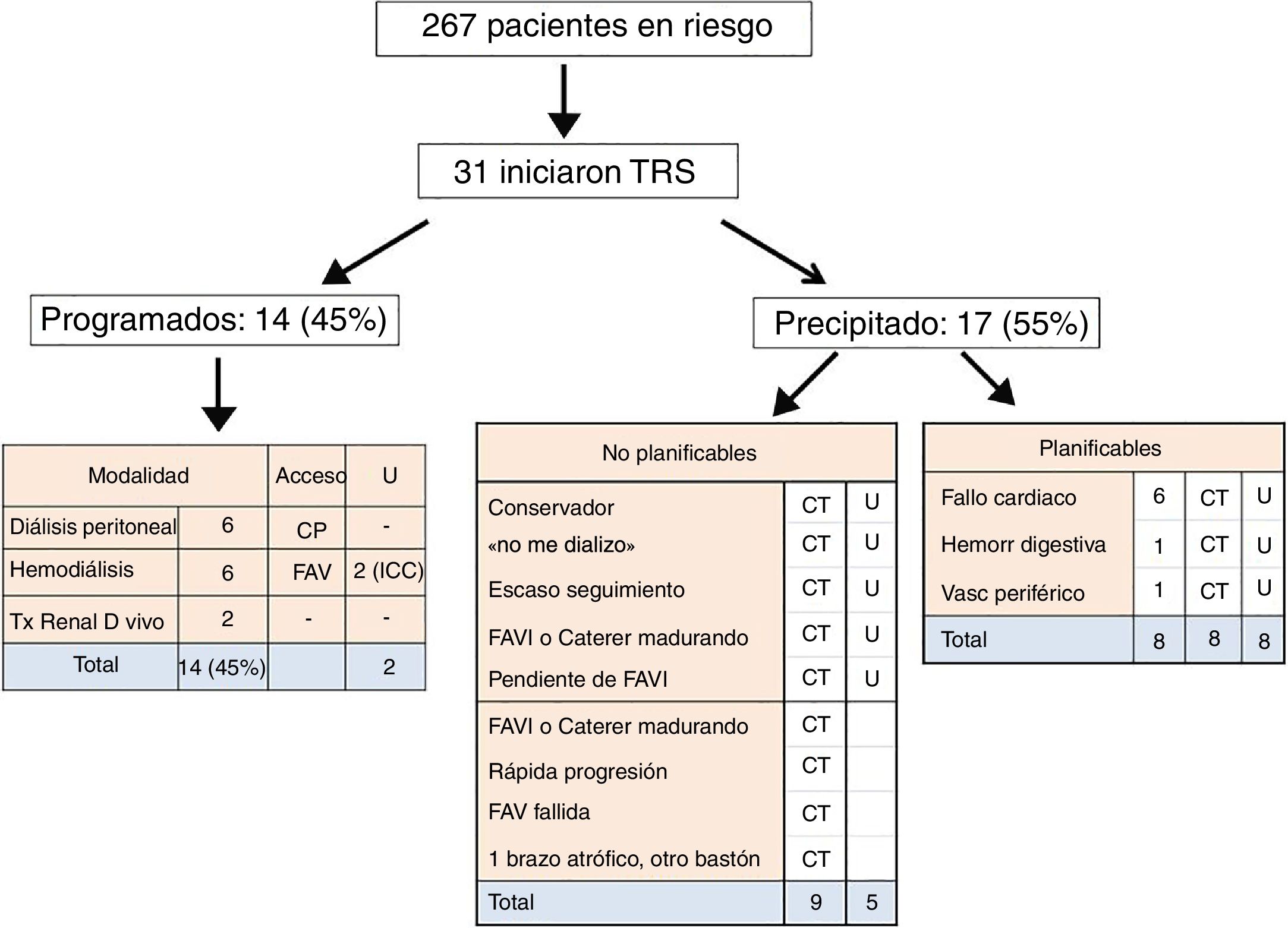
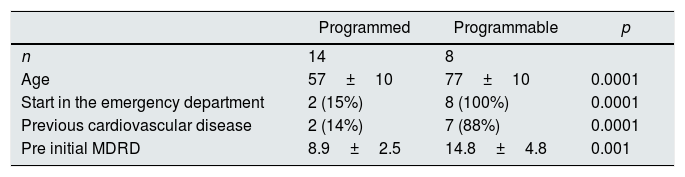
Initiation of renal replacement therapyRenal replacement therapy (RRT) was initiated in 31 patients (Fig. 3). In Fourteen (45%) patients the type of RRT had been planned and had arteriovenous fistula (AVF) or a functioning peritoneal catheter or an anticipated Kidney transplant. However, two of them started HD after visiting ER due to CHF. Nine of the patients who had a precipitous initiation of hemodialysis with a venous catheter, were on circumstances that can be consider virtually unavoidable.
Proportion of patients who started RRT, scheduled vs. unscheduled or precipitated initiation. Within this later group, patients were grouped in “unable to programme RRT” and “programmable RRT”. PC: peritoneal catheter. CHF: congestive heart failure. TC: tunnelled catheter
ER: start from the Emergency Room.
The second group is the most important for our analysis, since we consider that they were susceptible to earlier programming, thus avoiding the implant of a catheter. In these patients the initiation of dialysis was precipitated by cardiovascular causes.
Comparison of these two groups is shown in Table 3, the 14 patients stating dialysis in a programmed manner with AVF, peritoneal catheter in place or anticipated renal transplant. There were 8 additional patients that had to start regular hemodialysis using tunnelled catheter; they were seen in the ER and it is important to keep in mind that 80% had a history of previous cardiac events and three patients had 2 or 3 hospitalizations due to the same cause during the last year. However, the GFR measured in the outpatient clinic was twice as high as high as those who initiated dialysis on scheduled basis; thus, such a rapid progression of the kidney damage was not expected.
Comparison of patients that started on a scheduled basis versus those that we consider not programmed, but potentially programmable.
| Programmed | Programmable | p | |
|---|---|---|---|
| n | 14 | 8 | |
| Age | 57±10 | 77±10 | 0.0001 |
| Start in the emergency department | 2 (15%) | 8 (100%) | 0.0001 |
| Previous cardiovascular disease | 2 (14%) | 7 (88%) | 0.0001 |
| Pre initial MDRD | 8.9±2.5 | 14.8±4.8 | 0.001 |
CV: cardiovascular; MDRD: Modification of Diet in Renal Disease Study equation.36
We know that the GFR and proteinuria are the best markers of kidney damage and progression of disease.20–25 The GFR reflects magnitude of damage, and proteinuria is associated to the rapidity of progression.26–28 However, although its predictive value is unquestionable, they do not prevent a hasty start in a considerable proportion of patients.
A revision of the literature reveals that despite efforts to achieve a programmed initiation of RRT, more than half of the patients start RRT precipitously through a central venous catheter.10–13 The objective proposed by guidelines and documents is that 80% of the incidents in dialysis should start dialysis with a definitive access; however this objective appears to be difficult,29 although it is a priority in the management of this population. The increased age and increasing comorbidity, especially cardiovascular comorbidity, may not allow to achieve this objective despite the efforts by the professionals. In fact, heart failure is the main cause of hospitalization in patients 65 years and older, with a high rate of readmissions.30 The recent study by Ronksley PE and col31on renal patients confirm that 52% of emergency frequentations were due to CHF episodes.
There is abundant information about the importance of early referral to the nephrologist, so the initiation of dialysis is organized.2,8–10 But also, transcendent circumstances have been verified, beyond the moment of deriving the patient.12,32 A study similar to ours, by Gomis-Couto and col,12 analyzed the causes of not programmed initiation of dialysis, although they did not address the emergency room attendance. These authors emphasize that unexpected incidents and the accelerated aggravation of the ERC as the most non-preventable variable. But very important, the authors note that the greatest area for improvement lies in the delay in performing vascular access. In another study, Mendelssohn DC and col32 highlighted that 37% of patients started dialysis while hospitalized, and 54% with a temporary catheter; and that this is independent of early or late referral. In this regard, Bhan V and col33 emphasize that the delay in performing vascular access in fast progressors is an important preventable obstacle for a programmed initiation of dialysis.
The period of preparation to start RRT is variable among the centres, but not less than the two months required for maturation of AVF or for peritoneal catheter ready to use or even more time in the anticipated TxR.
The analysis of the frequency of ER visits and the reasons for precipitated initiation of dialysis may provide useful information. By reviewing the literature, we found that the issue of early initiation of dialysis was not approached from this perspective. The present study has provided information about the use of Hospital Emergency Services by patients with ACKD. Out of a population at risk of 267 patients, the frequency of ER visits was one every 4 days approximately, and the occupation of hospital beds was almost 3 beds/day. We did not find similar information from other sources, but the annual analysis should allow to analyze annual changes, and evaluate the results after improving strategies.
Our study also shows that despite the high age and comorbidity, the proportion of patients who died or who started RRT appear to be low (Fig. 1), however we have no other data to compare. This observation may s be similar – or better – in other health areas, but in any case, what indicates is that progress in health care entail a greater survival, a greater use of resources, and very importantly, generates an extraordinary health care expense that must adapt to these growing demand.34,35
The next step was to analyze the circumstances that precipitated the unscheduled initiation of dialysis and make an attempt to advance in the preparation of these patients. As also observed by Gomis-Couto A and col,12 there are situations as frequent as unavoidable described in Fig. 3 that precipitates the need for dialysis. The most characteristic cases are those patients that state “I will not be dialyzed” an idea that changes a soon as they find themselves in the ER symptomatic and at risk of losing their life, sudden renal deterioration due to an unpredictable intercurrent process; and failure or delay in preparation for access for dialysis. Other potential causes described in the study by Gomis-Couto A,12 such as acute renal failure that di not recover renal function or late referral to the nephrologist, have not occurred, since our practice receives patients that have already passed that filter.
The most interesting part of our study was the search of those cases that could have benefited from an early planning for dialysis. There is a sum of “extrarenal” factors which have been decisive for the hasty and not programmed beginning of dialysis; cardiovascular events accounted for six out of ten visits to the ER with precipitated start of hemodialysis with catheter (Table 2). This should warn the nephrologist of the need to speed up the preparation of patients with this clinical profile; despite the frequent subjective sensation of well-being between events, and with levels of renal function “acceptable”. In these cases, the most characteristic were the repeated episodes of CHF, the result of a frequent combination of underlying coronary disease, valvular disease and heart rhythm disorders; that frequently coexisting with chronic lung disease and gastrointestinal pathology. The last one is very important, since the frequent prescription of anticoagulants or antiaggregants, increases the risk of gastrointestinal bleeding, anaemia and heart failure.
The blood parameters (haemoglobin and serum albumin) were slightly lower in those patients that frequently visited the ER, but within a range close to normal, hence being helpful in warning about these events. Fig. 4 shows a diagram of the most frequent comorbidity profile that leads the ACKD patient to go to the Emergency Service symptomatic and initiate dialysis in a precipitated and unscheduled manner.
Coming back to our hypothesis, this analysis of the frequency of ER visits provides additional information to the glomerular filtration and proteinuria as the main variables of renal risk. As a corollary, we suggest that in circumstances illustrated in Fig. 4, especially if they have led the patient to attend the emergency department repeatedly in the last year, preparation for RRT should begin even with glomerular filtration rates of 20–25mL/min. Very especially for those patients with resistant proteinuria of medium-high range (more than 1.5g/24h and very especially if it is persistently greater than 2.5g). The early preparation of these cases does not imply initiating dialysis immediately, but giving priority to the preparation of the chosen modality.
Despite the retrospective nature of the study, and given the practical difficulty of preparing and obtaining results from prospective studies, we propose this opinion as a complement to the current recommendations for a scheduled initiation in technique.
Conflicts of interestThe author has no conflicts of interest to declare.
Please cite this article as: Lorenzo Sellarés V. Análisis de la frecuentación de Urgencias en consulta ERCA (enfermedad renal crónica avanzada): enseñanzas para optimizar el inicio programado en tratamiento renal sustitutivo. Nefrologia. 2018;38:622–629.