Dear Editor:
Primary Antiphospholipid Syndrome (primary APS) is an illness that is characterised by thrombotic phenomena, which are due to the presence of antiphospholipid antibodies. In 25% of cases the kidneys can be affected; this can present as progressive kidney failure, proteinuria, sediment changes, renal infarction,1,2 and less commonly, acute renal failure.
We would like to present the following case: female patient aged 65 years diagnosed with primary APS 20 years ago. Her personal history included several miscarriages, bilateral deep vein thrombosis, recurrent thrombophlebitis and lacunar stroke. Before she was admitted, her creatinine level was 1mg/dl, platelet count was 166,000/mm3 and she was being treated with acenocoumarol.
She was admitted for symptoms of acute cholecystitis, for which surgery was required, and during post-operative period she experienced a fever of 38º C, lumbar pain and oligoanuria.
An analysis was performed that recorded an Hb level of 9.3g/dl, Ht at 26%, platelets 66,000/mm3, creatinine 8mg/dl, urea 112mg/dl, K 4.8mg/dl, Ca 7.8mg/dl, LDH 790 and CRP 280mg/dl.
The test showed positive for anti beta-2 glycoprotein antibodies (55u/ml), lupus anticoagulant (88s) and anticardiolipine IgG (66u/ml); the rest showed no changes.
Systematic urine analysis: proteinuria, 0.7-0.9g/day; microhaematuria; and leukocyturia with granular casts.
Obstructive pathology and renal vascular pathology was ruled out with an abdominal CT.
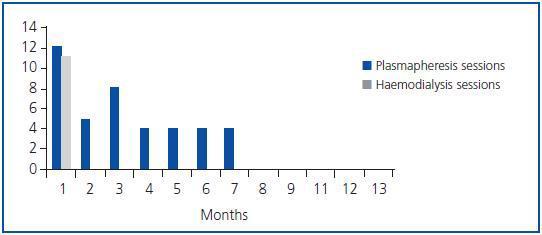
Evolution: thrombotic microangiopathy was detected from the renal biopsy. Eight plasmapheresis sessions were administered in 17 days and the diuresis recovered progressively, although haemodialysis was still necessary during the first month. The patient was discharged and the plasmapheresis sessions became less frequent (figure 1).
Three months later, the patient was admitted again due to decreased renal function associated with abdominalgia, choroidal ischaemia and positive antiphospholipid antibody titres. The profile was interpreted as a relapse of the disease and plasmapheresis sessions were started again and administered during four months, which led to improvement in renal function and the ocular condition.
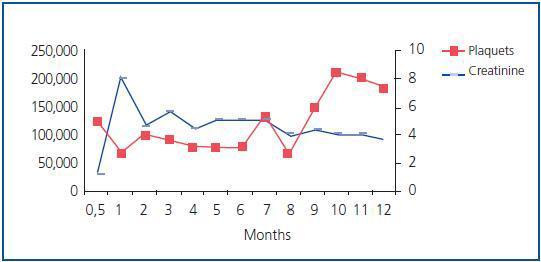
One year later, the platelets stabilised, the creatinine descended slowly (figure 2), and the antiphospholipid antibody titres were normal; there was no new thrombotic events.
The treatment of choice for primary APS is not well-defined2 and varies according to the clinical presentation. Some experts recommend high doses of anticoagulants,3 while others support the use of antiplatelet drugs or prophylactic anticoagulants in low doses. Other less successful treatments have used immunosuppressors and corticosteroids.3 For patients on anticoagulants who suffer thrombotic events that severely affect the kidneys and/or other organs, plasmapheresis is an option,4 as it was in our case.
Figure 1.
Figure 2.