Here we present the case of a 64 year-old male with a history of obesity, arterial hypertension, diabetes mellitus, and chronic atrial fibrillation, under treatment with oral anti-platelet drugs, who had had pain in the right lumbar fossa radiating to the groin for more than 24 hours, nausea and vomiting.
The patient was without fever and had a blood pressure of 140/90mm Hg. Heart auscultation revealed systolic murmur. The patient’s abdomen was soft and depressible, with pain in the left flank and hypochondrium and no succussion splash. The rest of the physical examination did not reveal any relevant findings.
Complementary tests also produced notable results including atrial fibrillation in the electrocardiogram, leukocytosis, elevated plasma creatinine, a marked increase in lactate-dehydrogenase (LDH) with normal transaminase levels,1-3 and microhaematuria. The urine culture test was negative, as well as parameters for autoimmune disease, immunoglobulins, and complement.
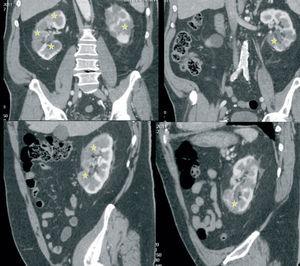
Due to the persistent abdominal pain and lack of concordance with digestive diseases, we performed an abdominal axial computed tomography that revealed segmental bilateral hypodense areas (Figure 1) with no lithiasis or dilation of the urinary tract. Together with the rest of the findings from examining the patient, this was suggestive of multiple renal infarctions, probably of an embolic origin.1
We then performed an echocardiogram that revealed dilated cardiomyopathy of an unknown cause and aortic stenosis.
After the evaluation, we started the patient on conservative treatment, maintaining therapeutic anti-coagulation,1-3 statins, and blood pressure control.
The patient’s clinical and biochemical progression was favourable.
Our final diagnosis was of cardio-embolic renal ischaemia in a patient with previous anti-coagulation treatment.
Conflicts of interest
The authors affirm that they have no conflicts of interest related to the content of this article.
Figure 1. Abdominal axial computed tomography