To the Editor,
In epidemiological studies we generally find a higher prevalence of chronic kidney disease (CKD) in women than in men, regardless of age.1,2 The study by Labrador et al assesses the prevalence of occult renal disease (defined as an estimated glomerular filtration rate (eGFR) below 60ml/min and serum creatinine within the normal range), and the authors found this condition in 43.5% of the women in a group with a mean age of 77 years.3
We therefore propose studying sex as a factor involved in GFR in a cohort of elderly patients with both normal and altered serum creatinine (sCr) levels. We will also analyse the effect of this factor in patients considered as carriers of occult renal disease.
Between January and April 2006, we conducted a cross-sectional study in a population with a mean age of 83 years (range: 69-97 years) that was recruited when patients came in for scheduled check-ups with the Geriatric Medicine and General Nephrology Departments at the General Hospital of Segovia. In this group, 38 patients had sCr within the normal range: Group 1, sCr ≤1.1mg/dl (range 0.7-1.1): 6 males and 32 females; 42 had altered sCr. Group 2, sCr >1.1mg/dl (range 1.2-3): 19 males and 23 females. In both groups combined, 68.8% of the patients were female; 37.3% of the total had diabetes mellitus, and 81.3% had arterial hypertension. GFR was estimated using the abbreviated MDRD method4 and the Cockcroft-Gault formula.5
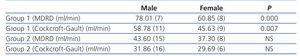
Table 1 shows the mean GFR given by the formulae, broken down by group and sex.
Out of the patient total, 56 (70%) had a GFR (MDRD) <60ml/min. Of the patients with a GFR<60ml/min according to MDRD, 18 had sCr within the normal range (100% female), while 38 had a baseline sCr>1.1mg/dl (15 males [39.5%] and 23 females [60.5%], P=.001.
The 18 patients with a normal sCr and GFR by MDRD <60ml/min (occult renal disease) had a mean age of 81.33±6 years.
In our study, we also found that eGFR (estimated using the two methods listed here) in women with sCr within the normal range was significantly lower than in men. However, these differences are not as pronounced in the patient group with altered sCr (Group 2). Our data therefore confirm a higher prevalence rate of CKD in women if they are evaluated by eGFR; this statement is especially true for the subjects in Group 1.
The differences in GFR between the sexes and study groups may lie within the mathematical formulae used to estimate GFR. The mathematical formulae used in our study are based on sCr, which involves the patient’s muscle mass and nutritional state. Therefore, these significant differences in GFR between the sexes among patients with a normal sCr are more likely to show women’s smaller muscle mass rather than their true GFR. It is also important to note that the MDRD formula was designed in patients with altered renal function and not validated in a healthy population: applying the MDRD formula to estimate GFR in individuals with a normal sCr may underestimate true GFR by up to 50%.6 On the other hand, when we use the MDRD formula in patients with altered renal function, the differences between males and females are less pronounced. This means that the resulting eGFR may successfully show the presence of kidney disease rather than the patient’s nutritional state and/or muscle mass.
In conclusion, sex is a factor to consider when checking for chronic kidney disease in the elderly. The systematic use of formulae based on creatinine levels can lead to healthy elderly women being considered carriers of occult renal disease.
Table 1. Mean estimated baseline glomerular filtration rates in the study group broken down by sex