Chronic kidney disease due to AA amyloidosis is one of the main complications of Familial Mediterranean Fever (FMF).1 In 2009, in the journal Nefrología, we presented the case of a 38-year-old woman of Armenian origin with severe nephrotic syndrome due to AA amyloidosis as a form of onset of FMF (with heterozygous M680I and M694V mutations in the MEFV gene). Given the severity of her proteinuria at diagnosis, deterioration in renal function and intolerance to antiproteinuric drugs, we started treatment with colchicine, at doses of 0.5mg/8h/day, and infliximab, at doses of 5mg/kg IV at baseline, at 2 weeks and subsequently every 2 months. In the clinical follow-up performed in the first year of treatment to evaluate her response to this, we reported partial remission: clinical improvement and improvement in renal function, but with persistent nephrotic proteinuria.2
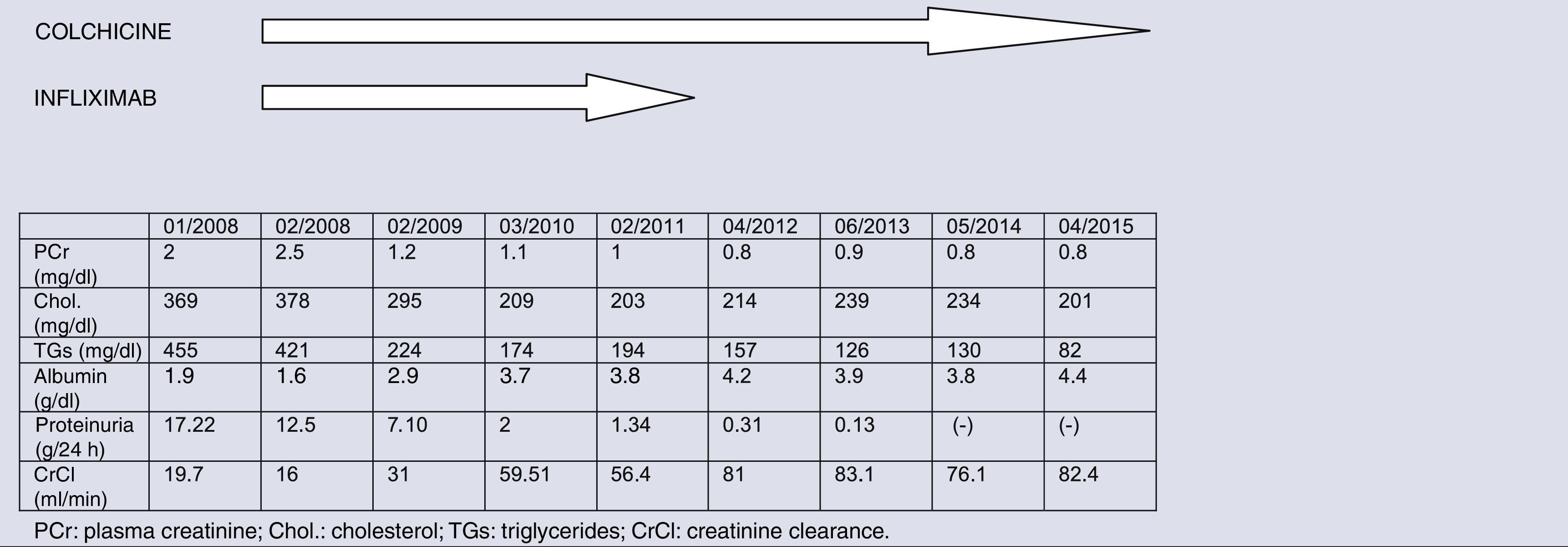
In this report we describe her mid-term clinical course. In the following 6 years, the patient has remained asymptomatic with no new episodes of hydropic decompensation or hospital admissions. Table 1 shows the clinical course of both her laboratory values and the treatment followed. Starting from the second year of treatment, colchicine was sustained continuously at doses of 1mg/day. Given that her proteinuria progressively decreased, infliximab doses were increasingly spaced out, to intervals of 4–6 months, and this treatment was permanently suspended in 2011.
As a result of combination therapy with colchicine and infliximab, in the acute phase of diagnosis of AA amyloidosis due to FMF, clinical improvement and improvement in renal function were achieved, but nephrotic proteinuria persisted. Subsequent follow-up required us to modify our initial conclusions: her clinical improvement was maintained, without any new hydropic decompensation, in the context of resolution of her proteinuria.
Treatment with colchicine is effective in preventing amyloidosis in Armenian patients with FMF.3 In cases of colchicine resistance or intolerance, anti-TNF agents may be effective to treat these patients and manage symptoms associated with FMF.4,5 In our case, given the initial severity of nephrotic syndrome, together with the findings of AA amyloid in the renal parenchyma and the M694V mutation associated with the most serious cases, combination therapy was decided upon, with a partial response in the first year and subsequently a complete response sustained over time. Perhaps this combination treatment, as it prevented the onset of new autoinflammatory episodes associated with FMF, would prevent more amyloid from being deposited in the renal tissue and, furthermore, progressive regression of the amyloid accumulated. In this case, we cannot confirm this, lacking new histology. However, the signs and symptoms may suggest it, as resolution of her proteinuria was achieved. In this regard Kutlugün et al. also reported in the literature 2 cases of complete remission of nephrotic syndrome with colchicine 1.5mg/day, sustained for a period of close to 30 years.6
In conclusion, the main kidney complication (chronic kidney disease) associated with AA amyloidosis due to FMF could be prevented through a resolution of proteinuria, which could be achieved with initial intensive combination therapy (colchicine+anti-TNF agent) and subsequent maintenance with colchicine.
Please cite this article as: Heras M, Saiz A, Fernández-Reyes MJ, Molina A, Astrid Rodríguez M, Callejas R. Remisión completa de síndrome nefrótico en mujer con amiloidosis renal por fiebre mediterránea familiar. Nefrologia. 2016;36:331–332.