To the Editor,
Haemophagocytic syndrome is a rare clinical condition characterised by a generalised, benign proliferation of histiocytes with significant haemophagocytic activity.1-3 The aetiology of these symptoms can be separated into two groups: primary or genetically determined, or secondary: virus, bacteria, fungus, parasites, neoplasia, collagen, immunodeficiency or drugs.1-7 Clinical symptoms include fever, hepatosplenomegaly, lymphadenomegaly, neurological symptoms, oedema and rashes.1,2,8,9 The most important laboratory findings are: pancytopaenia, hypertriglyceridaemia, hypofibrinogenaemia, hyponatraemia, hypoproteinaemia, increased levels of hepatic enzymes, increased amount of LDH and ferritin, pleocytosis in LCR and defective activity of natural killer (NK) cells.10 The histological analysis found haemophagocytosis in the bone marrow, spleen and lymph nodes. There were no malignant findings and diagnosis was possible with 2% of haemophagocytic cells.1-3 Haemophagocytic syndrome has a poor prognosis despite treatment, with an average survival of 2 weeks after the onset of the clinical symptoms. Survival can reach 60% at 5 years if there is an adequate response to treatment.11,12 Agents that interrupt histiocyte function and macrophage activation are therapeutic alternatives, such as etoposide, steroids, high-dose i.v. Ig, cyclosporine A, anti-thymocyte globulin, anti- TNF antibodies, and in some cases, bone marrow transplant.13,14
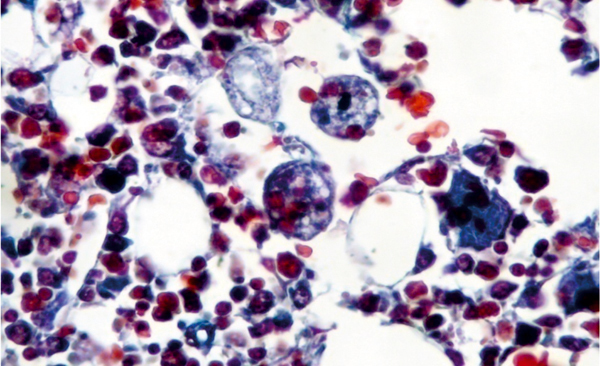
We present the case of a 53-year-old man, subjected to kidney transplant, who came to the emergency department with fever, temperature 38.5ºC over a 24-hour period, with shivers, mild diffuse abdominal pain, asthenia, anorexia, and a decrease in diuresis volume. The physical examination was normal and no important pathology was found from the tests performed at the emergency department: normal X-ray; normal blood and urine tests; negative blood and urine cultures; negative cytomegalovirus (CMV) early-antigen (at that time, CMV polymerase chain reaction (PCR) assays were not available in our hospital). The symptoms worsened, abdominal pain increased, and on the CT scan we observed dilated small bowel loops due possibly to ischaemia or infection. Given the findings and the worsening clinical symptoms, we performed an exploratory laparotomy, without observing anomalies. A coagulase-negative staphylococcus grew in the peritoneal fluid, which was treated with meropenem at 500mg every 12 hours. Following the intervention, the clinical symptoms improved despite having developed a post-operative paralytic ileus, which improved spontaneously. After a few days, the patient presented with fever again, and diarrhoea. There were initially no traces of blood, but he then presented with melaena, associated with neurological deterioration, hepatosplenomegaly and hepatic function alterations, anaemia and thrombocytopaenia. New tests were requested: positive CMV early-antigen; CMV PCR assay above 100 000 copies/ml. Eso-Gastro-Duodenoscopy (EGD): infected oesophagus. Analytical tests showed: GOT/GPT: 135/156IU/l; LDH: 558IU/l; sodium: 130mEq/l, fibrinogen:133mg/dl, haemoglobin: 9.2 g/dl; and haematocrit: 26.8%; platelets: 48 000µl with normal leukocytes (normal formula: 5500µl), significant increase in triglycerides (738mg/dl), progressive deterioration of kidney function (creatinine around 4-5mg/dl). Normal haptoglobin, negative indirect Coombs test. Peripheral blood smear: few schistocytes with no reticulocyte. Bone marrow aspiration: compatible with haemophagocytic syndrome (Figure 1).
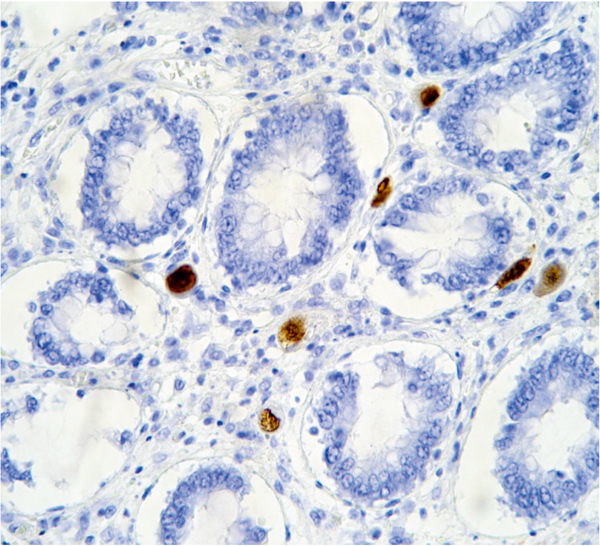
Given these findings, the patient was diagnosed with CMV-associated haemophagocytic syndrome. The patient visited infection diseases unit and the following therapeutic regimen was started: anti-CMV with ganciclovir 50mg/12h and non-specific i.v. gamma globulin 30g/48h, and methylprednisolone bolus were indicated for haemophagocytic syndrome. The patient continued to take cyclosporine at low doses (around 50ng/ml). Despite being treated, the patient’s general and neurological condition worsened and he was finally admitted to the ICU for saturation, where he died 12 hours after admission due to multiple organ failure. The autopsy showed: disseminated CMV infection, mainly affecting the digestive tract and lung (Figure 2) and reactive haemophagocytic syndrome (Figure 1).
The prevalence of haemophagocytic syndrome in kidney transplant patients is 0.4%,11 which makes it a rare complication in this patient group. Furthermore, the most common aetiology for these patients is that secondary to an infection.14 These patients have poor prognosis meaning that early diagnosis is essential to enable starting therapy early. There is no consensus on treatment strategies, and several treatments have been proposed, such as steroids and cyclosporine,14 specific immunoglobulin, treating the aetiological agent, etc.
On the other hand, CMV-associated infections in kidney transplant patients is a common complication, although its incidence and repercussion is decreasing due to the prophylaxis employed.15 In spite of this, it is a diagnosis that we should take into account when a transplant patient’s general condition deteriorates, because the complications for this infectious profile are all serious. Early diagnosis and starting correct therapy greatly improves prognosis.
Haemophagocytic syndrome is a rare complication following kidney transplantation. Furthermore, it is a clinical entity that must be considered during the differential diagnosis of these patients, especially if associated with fever, organomegaly and pancytopenia. Bone marrow aspiration allows for a clearer diagnosis, whereas blood test analyses only enable us to make presumptions (pancytopaenia, hepatic kidney function alteration, increase in LDH, decreased fibrinogen, increased triglycerides, hyponatraemia, etc). Viral infection is the most common triggering agent for immunosuppressed patients. The problem is that there is still no specific treatment, meaning that transplant patient survival is very low, and if patients were to survive, the kidney graft does not often function correctly.
Figure 1. Trichrome staining. Histiocytes with red blood cells indicating haematophagous activity in bone marrow.
Figure 2. Immunoperoxidase staining. Cells containing CMV in the intestinal tissue.