Dear Editor,
Primary distal renal tubular acidosis (dRTA) is a tubule disease characterised by metabolic acidosis with inappropriately alkaline urine, hypopotassaemia and hypercalciuria. It may be sporadic or hereditary, with a dominant or recessive autosomal pattern. The severity of the clinical spectrum may vary greatly, from slight, asymptomatic compensated acidosis with an occasional calculus to severe acidosis with delayed growth and early onset nephrocalcinosis caused by kidney failure. In general, patients with dominant-pattern dRTA have a milder phenotype than those with a recessive pattern.1
A subgroup of recessive dRTA patients suffers from progressive neurosensory deafness, caused by mutations in the gene that codifies sub-unit B1 in H+-ATPase (ATP6V1B1).2 The clinical profile for this tubular alteration, besides the deafness, is similar to that described for other types of dRTA.
We present the clinical evolution of a patient with dRTA with neurosensory deafness and chronic kidney disease secondary to nephrocalcinosis over a 30-year follow-up period.
Male patient aged 36. A few days after birth his clinical profile included frequent vomiting, polyuria, polydypsia, psychomotor delay, hyperchloraemic metabolic acidosis, hyperchloraemia, hypopotassaemia, alkaline urine and nephrocalcinosis, and he was diagnosed with dRTA. His family history included parents related by blood, one sibling with dRTA who died in a workplace accident and another healthy sibling.
The patient has been examined in our centre since he was six years old and receiving treatment with sodium citrate and oral potassium supplements.
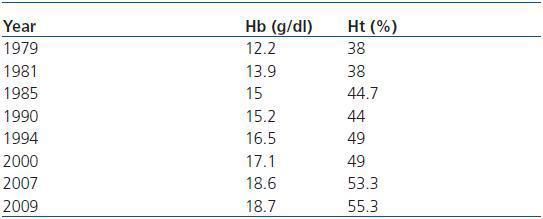
Laboratory analysis data of interest: pH 7.07-7.33, bicarbonate 10-26mmol/L, Cl 113-124mEq/L, K 1.8-3.5mEq/L. Magnesium, calcium, phosphorus, ALP, PTH and Vitamin D levels are normal. Hb 12.2-18.7g/dl, Ht 38-55.3%. Urine: pH 7-8, anion gap 43mEq/l, Calcium 2.5-4.5mg/kg/day, Phosphorus 6-12mg/kg/day. Urineplasma PCO2 difference: 2mmHg (urine pH: 7.25 and plasma pH: 7.33), CaO/CrO index: 0.16-0.24.
The patient¿s treatment was irregular; he stopped taking his medication frequently, and often did not attend check-ups. This resulted in numerous admissions to hospital due to hypopotassaemic muscle paralysis and severe metabolic acidosis that would resolve quickly once bicarbonate and potassium treatment was administered.
When the patient was 16, a slow but progressive decrease in renal function began and the nephrocalcinosis became worse (figure 1). At 19, hearing loss was detected; the patient was diagnosed with bilateral neurosensory deafness, and needed a hearing aid.
At 25, he developed bilateral renal lithiasis and complications and hospital admissions have been common over the last 10 years. Most worthy of note are his bilateral renal colic episodes and the development of spontaneous steinstrasse, which on some occasions resolved with spontaneous expulsion of the stones, and on others required urethral catheterisation with a double J Stent and lithotripsy. Several episodes caused obstruction of the urinary tract with hydronephrosis and acute renal failure added to his chronic kidney disease; this resolved upon expulsion of the stones.
The latest check-ups show a progressive increase of nephrocalcinosis. There is also a parallel progressive increase of Hb and Ht levels currently with polycythaemia (table 1) and a normal EPO level (11.6mU/ml).
The patient currently maintains a stable creatinine clearance rate of about 45ml/min.
This case is important to us because our patient shows the main complications that can arise from this disease: 1) hypopotassaemic muscular paralysis as a result of discontinuing treatment frequently. 2) bilateral renal lithiasis, which in turn has caused obstructive acute renal failure requiring multiple urinary tract procedures, and has even provoked spontaneous steinstrasse, which is seldom described in this type of patient.3 3) polyglobulia, probably secondary to nephrocalcinosis, since the tissue hypoxia would induce an increase in EPO production which, although still in the normal range in our case, could be inappropriately high for such a high haemoglobin level. In the literature, this complication has very rarely been reported in association with dRTA;4,5 4) chronic kidney disease, which in our case is progressing very slowly, despite numerous complications (20 years have passed since the creatinine clearing rate began to decrease) and which has been stable over the last few years.
We conclude that with dRTA, supervising compliance with the treatment is very important for avoiding complications, some of which are potentially severe and completely avoidable. Paying attention to polycythaemia secondary to nephrocalcinosis is also crucial, as the condition could foster the development of thrombotic events in these patients. Despite everything, the renal failure has been progressing very slowly over 30 years of observation.
Table 1.
Figure 1.