Dear Editor,
Diabetic retinopathy is a microvascular complication of diabetes mellitus and its prevalence is closely related to long term diabetes, chronic hyperglycaemia, nephropathy and hypertension.1 It has been shown that a decrease of blood pressure decreases retinopathy progression.2 The benefits of hypotensive treatment for microvascular and macrovascular complications can be seen from blood pressure values <130/80 mmHg. To achieve this it is necessary to use combined therapies.1
Given the close relationship between diabetic retinopathy, diabetic nephropathy and hypertension, we have studied 63 patients with diabetic nephropathy due to diabetes mellitus type 2 (DM2) who came in to our outpatient offices consecutively. The patients had a mean age of 65.24 + 7.47 years, 26 were women and 37 were men. Statistical analysis was carried out with the statistical software package SPSS 15.0 for Windows.
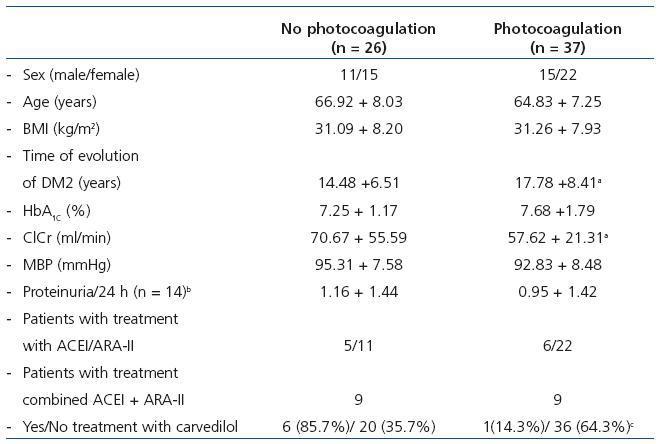
The patients were divided into 2 subgroups: one group that had not received photocoagulation (n = 26) and another group that had received it (n = 37). The clinical characteristics and the number of patients treated with carvedilol in both subgroups can be seen in Table 1.
In the subgroup of patients that had not received photocoagulation, 35.7% were being treated with carvedilol in comparison with 14.3% in the group who had received photocoagulation (p = 0.017). Since there were no differences in their mean blood pressure, it can be inferred that the effect of carvedilol is independent of its hypotensive effect.
Carvedilol has a blocking effect on beta-adrenergic receptors combined with vasodilator action based on the blockage of alfa-1-adrenergic3 receptors. In experimental studies carvedilol has been shown to have protective and antioxidant4 effects on perivascular inflammation.5 These effects could, in part, be explained by the results of our study. Although it is probably limited by the number of patients studied, the finding that the percentage of patients who received carvedilol in the subgroup that did not receive photocoagulation is significantly higher than in the group that did receive photocoagulation should be taken into account when treating patients suffering from diabetic nephropathy. Subsequent studies should evaluate if carvedilol prevents the development of diabetic retinopathy.
Acknowledgements
The authors wish to acknowledge Professor Limiñana for his help with the statistics.
Table 1. Subgroups of patients with diabetic nephropathy caused by DM2 based on whether they had or not received photocoagulation