Introducción: El cuidado especializado de los pacientes en estadios avanzados de la enfermedad renal crónica (ERC) se asocia a una mejor supervivencia en diálisis, pero se desconoce qué tratamientos favorecen específicamente esta evolución. Objetivos: Analizar las intervenciones terapéuticas habituales en el estadio de ERC avanzada y establecer cuáles de ellas se asocian a una mejor supervivencia en diálisis y su relación con las causas de muerte. Material y métodos: Estudio de cohortes, prospectivo y de observación, que incluyó a 591 pacientes que iniciaron diálisis (491 hemodiálisis y 100 diálisis peritoneal), que habían sido controlados previamente en la consulta de ERC. Las intervenciones terapéuticas analizadas fueron: tratamientos antihipertensivos, estatinas, antiagregantes plaquetarios, inhibidores de la xantina-oxidasa, corrección de la acidosis metabólica, tratamiento con captores de fósforo (cálcicos o no), vitamina D (calcitriol o paricalcitol), eritropoyetina y disponibilidad de fístula arterio-venosa interna (FAVI). La asociación independiente de cada uno de estos tratamiento con la mortalidad en diálisis fue analizada mediante modelos de regresión de Cox con ajuste a edad, sexo, tiempo de seguimiento prediálisis, función renal al inicio de diálisis, comorbilidad, albumina sérica y proteína C reactiva, y con estratificación al tipo de diálisis. Resultados: Con una mediana de seguimiento de 28 meses, la cifra total de fallecidos fue de 191 (32 %). En los modelos multivariantes se observó que, además de la edad, el índice de comorbilidad y la albúmina sérica, el tratamiento prediálisis con inhibidores de la enzima de conversión y/o antagonistas de los receptores de la angiotensina, la corrección de la acidosis con bicarbonato sódico y la FAVI al inicio de la hemodiálisis se asociaron de forma significativa con una mejor supervivencia en diálisis. No se observaron diferencias en las causas de muerte entre los diferentes tratamientos analizados. Conclusión: Estos resultados sugieren un posible beneficio diferido de algunos tratamientos en estadios prediálisis sobre la evolución en diálisis. Además, el inicio de hemodiálisis sin una FAVI, y por tanto la necesidad de utilización de catéteres endovenosos, empeora el pronóstico de estos pacientes.
Introduction: Specialised care of patients in advanced stages of chronic kidney disease (CKD) is associated with better survival in dialysis, but it is not known which treatments specifically favour this outcome. Objectives: To analyse normal treatment in advanced stages of CKD and establish which treatments are associated with better survival in dialysis as well as their relationship with causes of death. Material and method: Cohort, prospective observational study of 591 patients who started dialysis (491 haemodialysis and 100 peritoneal dialysis), who had previously been monitored in the CKD clinic. The treatments analysed were: antihypertensive treatments, statins, antiplatelet drugs, xanthine oxidase inhibitors, correction of metabolic acidosis, treatment with (calcium or non-calcium) phosphate binders, vitamin D (calcitriol or paricalcitol), erythropoietin and the availability of an internal arteriovenous fistula (IAVF). The independent association of each of these treatments with mortality in dialysis was analysed using Cox regression models adjusted for age, sex, pre-dialysis monitoring time, renal function at the start of dialysis, comorbidity, serum albumin and C-reactive protein, and with stratification of the type of dialysis. Results: With a median follow-up period of 28 months, the total number of patients who died was 191 (32%). In the multivariate models, we observed that, in addition to age, the comorbidity index, serum albumin, pre-dialysis treatment with angiotensin-converting-enzyme inhibitors and/or angiotensin receptor blockers, correction of acidosis with sodium bicarbonate and IAVF at the start of haemodialysis were significantly associated with better survival in dialysis. We did not observe differences in causes of death between the different treatments analysed. Conclusion: These results suggest a potential delayed benefit of some treatments in pre-dialysis stages on the outcome of dialysis. Furthermore, beginning dialysis without an IAVF, resulting in the need for intravenous catheters, worsens prognosis in these patients.
INTRODUCTION
Mortality remains very high in dialysis patients. Age and comorbidity are the main determining factors of mortality in this population, but these factors can obviously not or hardly be changed.
An epidemiological feature of dialysis patients is the lack of association between classic cardiovascular risk factors and mortality1. Moreover, the few randomised studies carried out in this population have not demonstrated clear benefits on survival with the use of various drugs proven to be useful in the non-uraemic population or with other therapeutic measures based on sound pathophysiological principles2.
Moreover, some studies have warned us about the potential risk of drugs commonly used in chronic kidney disease (CKD), such as erythropoietin (EPO)3 or calcium salts4, which adds even more difficulty and confusion to the management of these patients.
The specialised care of pre-dialysis patients in advanced stages of CKD is unanimously considered to be a factor that benefits survival in dialysis5,6. In these advanced chronic kidney disease (ACKD) clinics, many treatments are usually carried out, such as controlling blood pressure, correcting over-hydration, metabolic acidosis, mineral and bone disorders and anaemia, creating vascular access and choosing when to start dialysis, etc., but the importance of each of these treatments and the benefits they can bring in terms of dialysis patient survival is unknown.
We carried out this prospective study with the objective of analysing the normal treatments for ACKD and establishing which of them are associated with greater survival in dialysis, as well as their relationship with causes of death.
MATERIAL AND METHOD
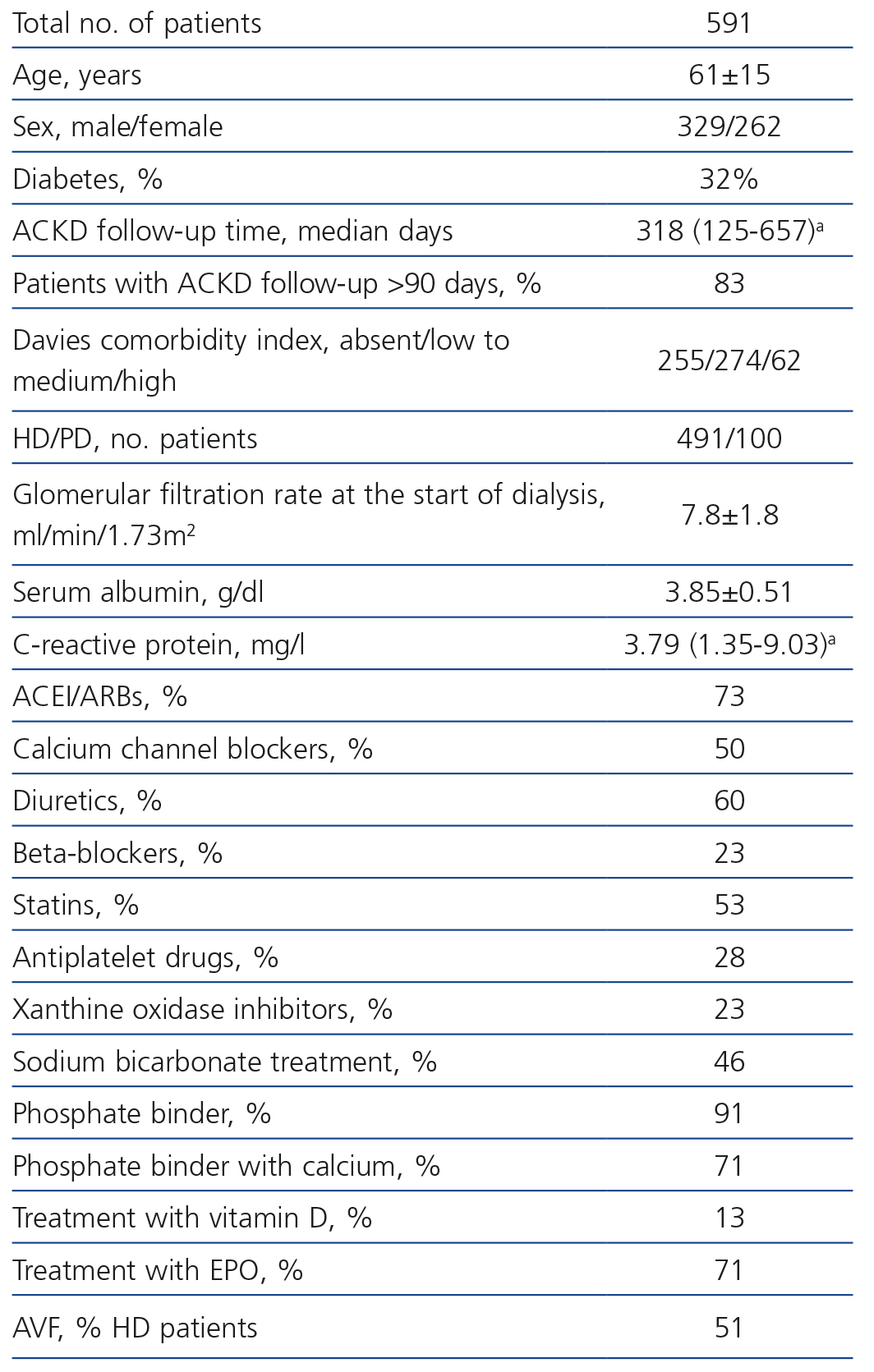
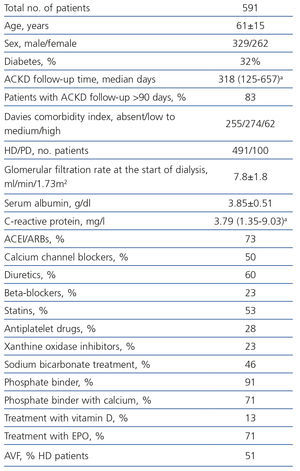
We included 591 patients with the demographic and clinical characteristics that are displayed in Table 1. Inclusion criteria were as follows: having begun dialysis treatment at the Hospital Infanta Cristina de Badajoz during the period between October 1999 and January 2012, and having previously been monitored in the ACKD clinic of the same hospital. We did not exclude any patients.
We started haemodialysis (HD) in 491 patients and peritoneal dialysis (PD) in 100. There were no pre-dialysis kidney transplantations.
The information on the treatment that the patients were receiving was obtained by anamnesis and a review of medical records.
The treatments used during the pre-dialysis stage that were analysed in this study were: treatment with angiotensin-converting enzyme inhibitors (ACEI) and/or angiotensin receptor blockers (ARBs), diuretics, calcium channel blockers, beta-blockers, statins, antiplatelet drugs, xanthine oxidase inhibitors, correction of metabolic acidosis with sodium bicarbonate, treatment with (calcium or non-calcium) phosphate binders, calcium salts, active vitamin D (calcitriol or paricalcitol) and anaemia correction by EPO. Furthermore, we included an internal arteriovenous fistula (IAVF) in our treatment, and this was usable at the time dialysis began.
The covariates included to adjust survival models were: age, sex, Davies comorbidity index (three subgroups: no comorbidity, mild to moderate, and severe comorbidity) , diagnosis of diabetes mellitus, serum albumin concentrations (bromocresol green, Advia Chemistry, Siemens Healthcare Diagnostics) and C-reactive protein (high sensitivity by chemiluminescence immunoassay in the solid phase, Immulite, Siemens). As potential confounding variables, we also included the glomerular filtration rate (MDRD-4) at the start of dialysis and the follow-up time in the ACKD clinic (greater or less than 90 days).
The lack of a functioning IAVF in patients included in this study who started HD may have been due to one of the following reasons: failure (thrombosis), its rejection by the patient or insufficient pre-dialysis follow-up time.
Patients were followed-up with regard to their outcomes in dialysis, with death due to all causes being the only study event. The follow-up period began with the first dialysis session and patients were censored (non-informative censoring) for the end of data collection (September 2012), loss to follow-up and renal transplantation.
We also recorded the cause of death, establishing five etiological groups: sudden death, death from cardiovascular, infectious, tumour and other causes.
To analyse whether there was an association between the different pre-dialysis treatments and survival in dialysis, we used Kaplan-Meier curves (univariate study) and Cox multivariate proportional hazards models, with the calculation of the instantaneous hazard rates (hazard ratio) and their 95% confidence intervals. Covariates in multivariate models were selected automatically, using the backwards progressive conditional elimination process.
Due to the potential confounding by indication in the inclusion of PD and HD patients, who not only had age and comorbidity differences, but also had differences in other characteristics that were not recorded as variables but nonetheless had a potential influence on survival, such as socio-economic and cultural level or the degree of dependency, the analyses were stratified according to the initial form of treatment (HD or PD).
The analysis of survival and stratification between PD and HD was in any case considered by intention-to-treat, independently of the time that the patient would have remained on one or another dialysis technique.
For comparison of continuous variables between patients who survived or died, we used Student’s t-test or the Mann-Whitney test, depending on the characteristics of the variable distribution. The χ2 test was used to compare categorical variables between subgroups.
The data were presented as a mean ± standard deviation or the median and interquartile ranges. A p value less than .05 was considered to be statistically significant. For statistical analyses and creating graphs, we used the SPSS version 15.0 software (SPSS, Chicago, USA) and STATA version 11.1 (Stata Corporation, Texas, USA).
RESULTS
Mortality in dialysis
With a median follow-up of 28 months (interquartile ranges: 13-50 months), the total number of deaths was 191 (32%) and estimated median survival was 82 months (95% confidence interval: 56-108 months).
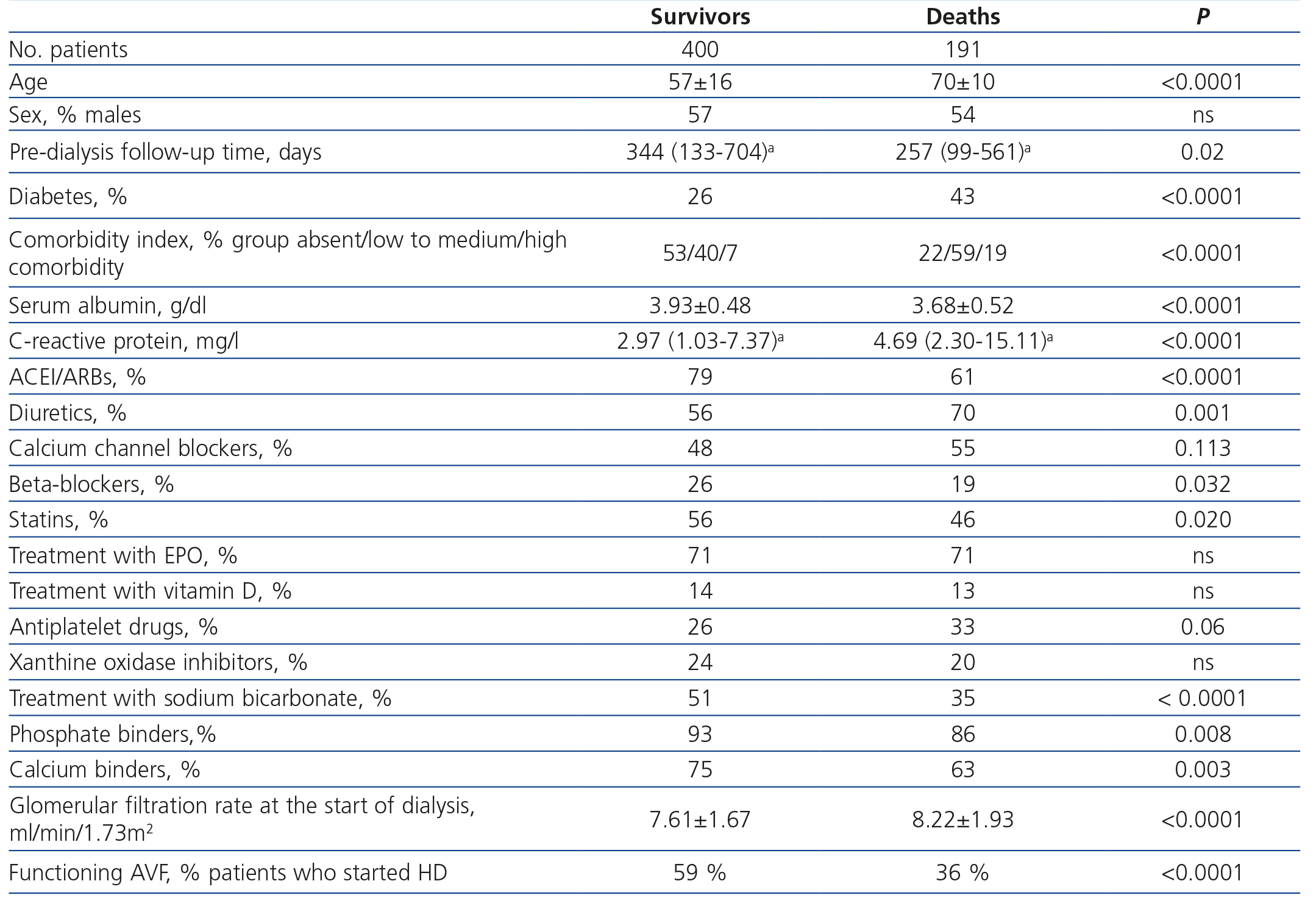
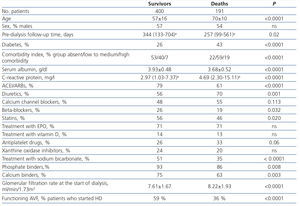
The demographic, clinical and biochemical characteristics of the patients who survived and died are displayed in Table 2. As well as the factors that were very much expected to be associated with mortality such as age, comorbidity and serum albumin and C-reactive protein concentrations, we note the low mean follow-up time in the ACKD clinics of the patients who died (Table 2). We also observed significant differences in pre-dialysis treatments between those who survived and those who died, which highlights the positive association between survival and ACEI/ARBs, beta-blockers, statins, sodium bicarbonate and phosphate binders, and even calcium salts. By contrast, the association was negative for survival with diuretics and at the limit of significance with antiplatelet drugs. We did not observe differences in the percentage of EPO, vitamin D or xanthine oxidase inhibitor prescription between those who survived and those who did not.
The glomerular filtration rate at which dialysis began was significantly higher in patients who died and the percentage of patients with an IAVF was significantly lower in this same subgroup (Table 2).
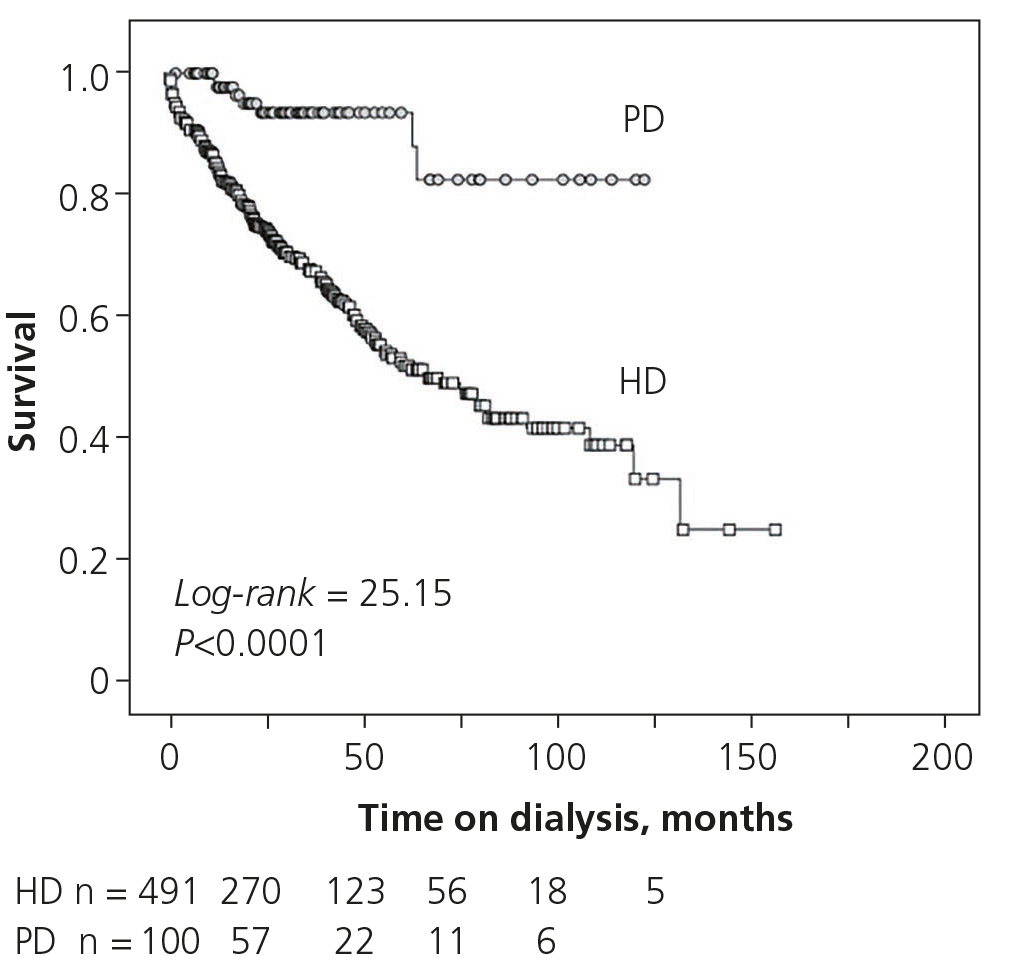
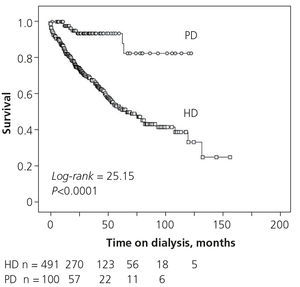
Patients whose initial treatment was with PD had better survival than those treated with HD (Figure 1), although it is important to highlight again that there were major differences between both subgroups with regard to age, comorbidity and other factors that potentially influenced survival that were not recorded in this study, such as socio-economic, cultural and dependency levels.
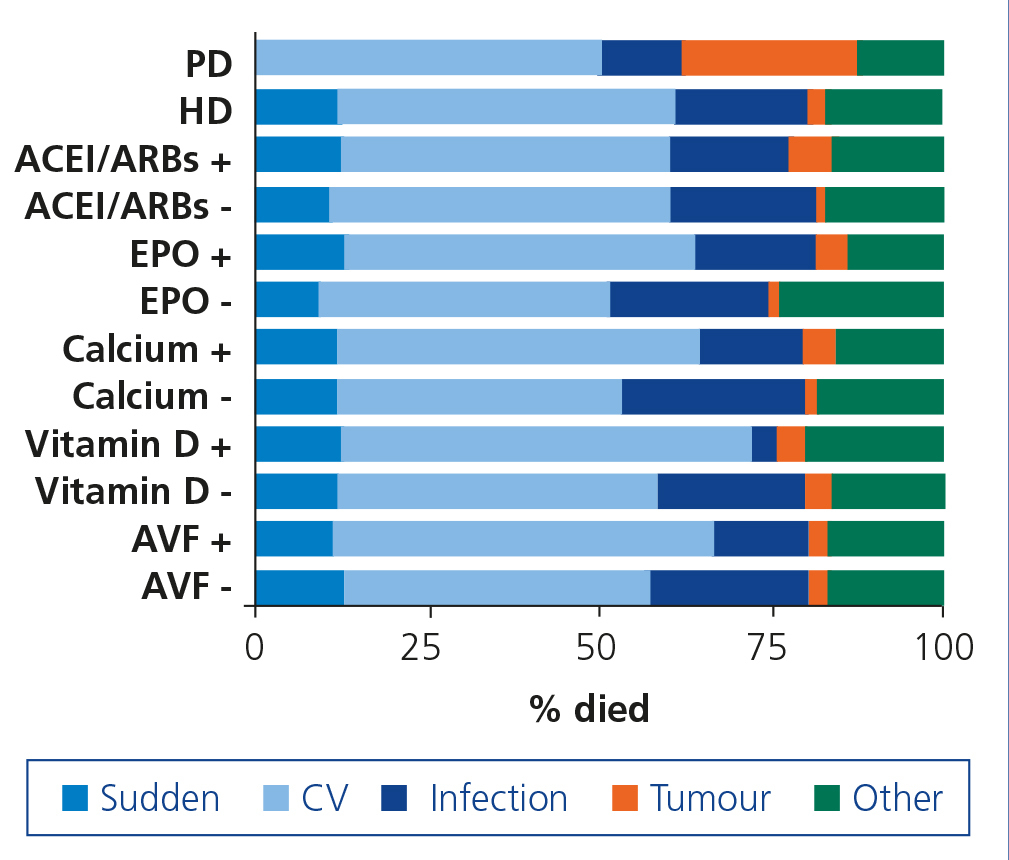
Causes of death according to pre-dialysis treatments
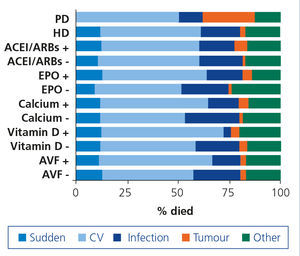
Figure 2 displays the causes of death grouped into five aetiological sections (sudden death, cardiovascular, infection, tumour and other causes), according to the type of initial dialysis and some treatments carried out in the pre-dialysis stage. Those of cardiovascular and infectious origin were the most common causes of mortality.
The only significant difference observed was between PD and HD (p=.02), with there being an absence of sudden death in PD patients and on the other hand, a greater proportion of death from tumours, due to a lack of oncological control of myeloma and leukaemia that were already related to the origin of renal failure.
We did not observe significant differences in the cause of death between those treated and those not treated with EPO, vitamin D or calcium salts. The differences in the cause of death between patients who began HD with or without an IAVF were not significant either, although there was a higher rate of death from infectious aetiologies in those who did not possess an IAVF.
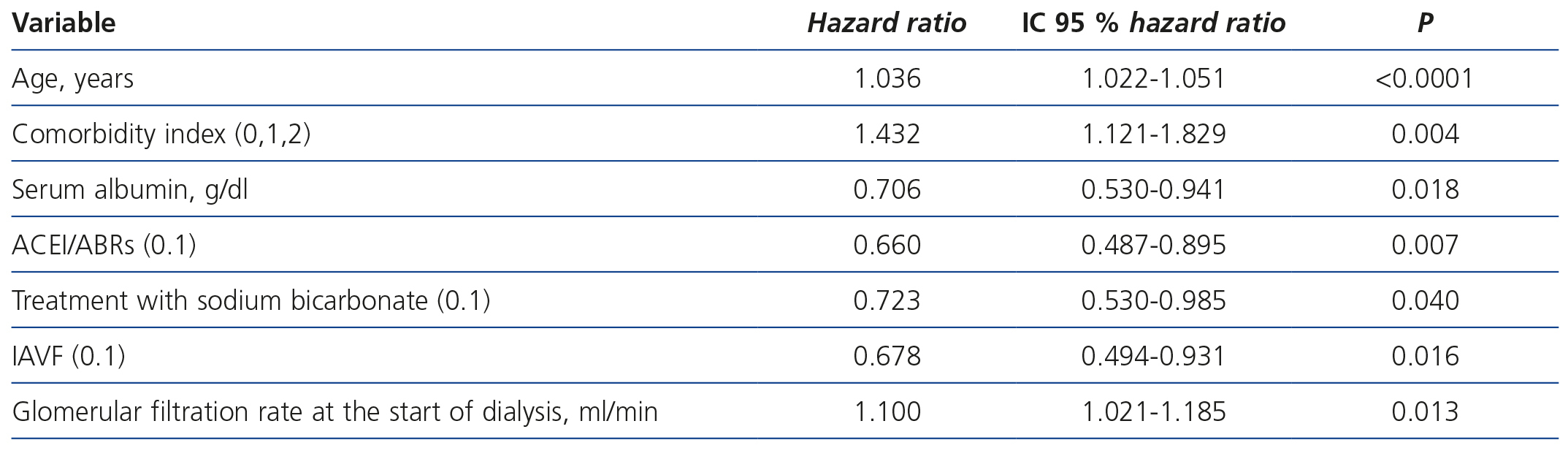
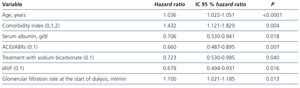
Analysis of survival and its association with the study variables
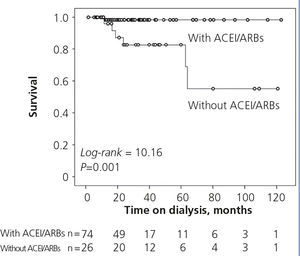
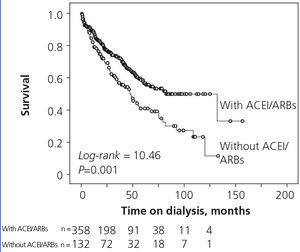
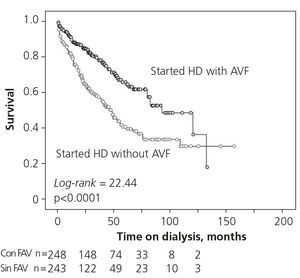
In the Cox stratified regression analysis according to the initial type of dialysis (Table 3) we observed that, as well as age, the comorbidity index and serum albumin, pre-dialysis treatment with ACEI/ARBs and the correction of acidosis with sodium bicarbonate were positively associated with survival in dialysis. We also note the positive and significant association between the availability of an IAVF at the start of HD and survival. By contrast, higher renal function at the start of dialysis was associated with worse survival.
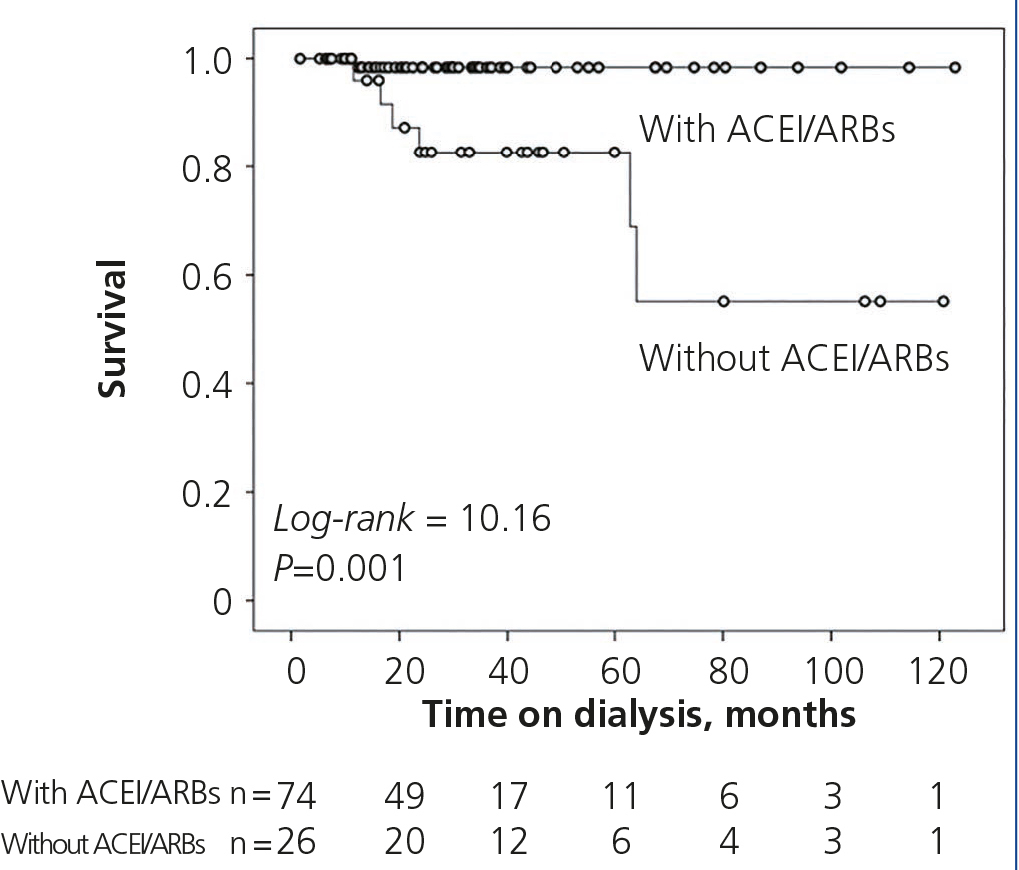
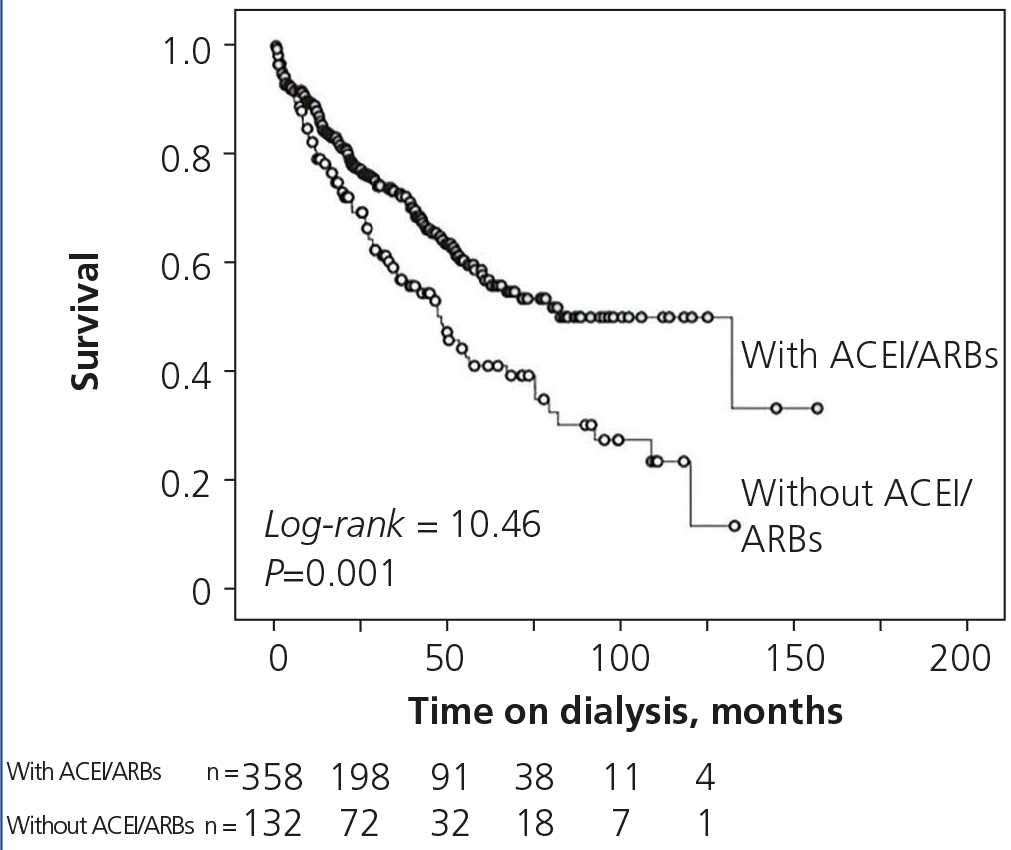
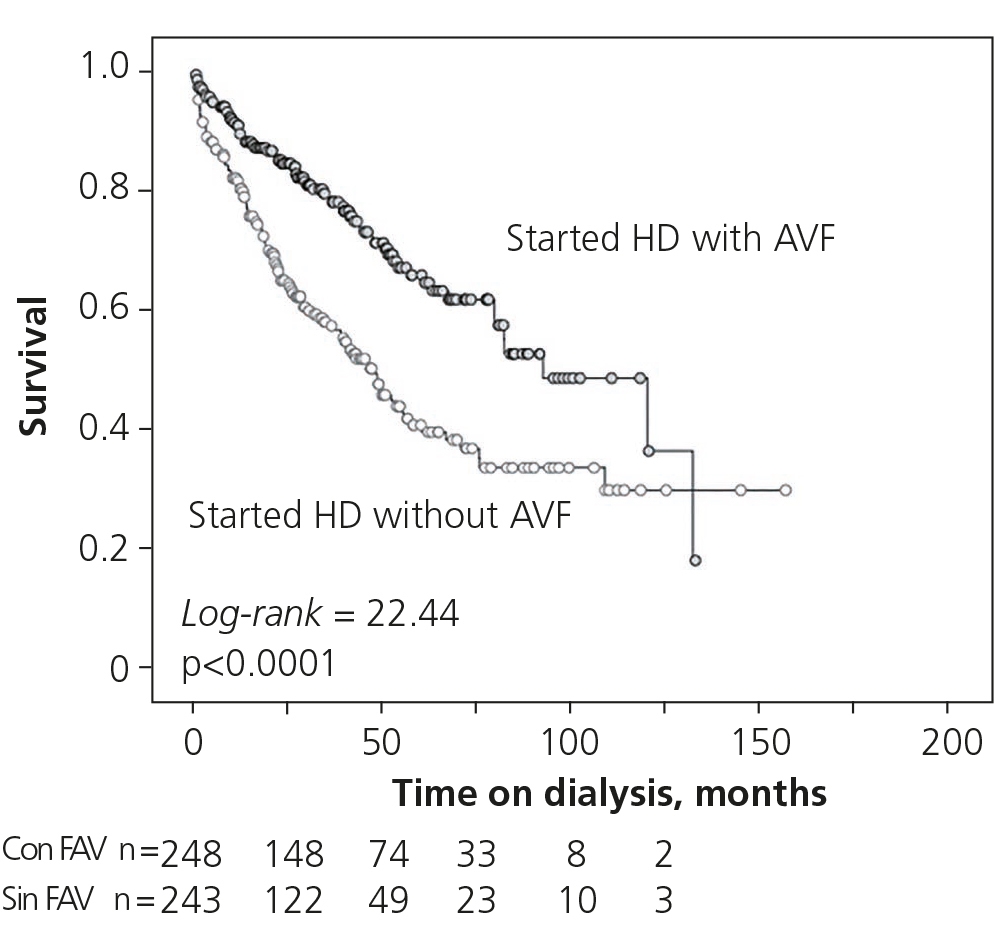
Figures 3 and 4 display the dialysis survival curves of the patients who had been treated and those who had not been treated with ACEI/ARBs during the pre-dialysis period. Figure 5 displays the survival curves of patients who started HD with or without an IAVF.
DISCUSSION
Mortality in dialysis patients continues to be very high. Some characteristics of CKD such as the growing severity of its complications as renal failure progresses, as well as accumulative adverse effects, some of them irreversible, could help us to understand this disconcerting fact. As such, the monitoring and treatment of the disease in less advanced stages may have a major influence on the survival of patients who reach more advanced stages.
This is a hypothesis that would explain better survival in dialysis of patients who were monitored and treated in ACKD clinics.
The results of this study show that there are various pre-dialysis treatments that are significantly associated with a better outcome in dialysis patients, but the only ones to remain in the models adjusted for age, sex, comorbidity, dialysis type and other prognosis markers were treatment with ACEI/ARBs, metabolic acidosis correction with sodium bicarbonate and the introduction of an IAVF in those who began HD. By contrast, we did not observe that any of the treatments analysed in adjusted models were associated with a worse outcome or any specific cause of death.
Due to strong confounding by indication in this study, we cannot claim that there is causality between the direct therapeutic effects of these drugs and improved survival in dialysis patients, even after adjustment with the confounding variables, but we believe that the data provide information that could prove useful in the prediction of outcomes in dialysis patients.
The effect of treatment with ACEI or ARBs on ACKD or dialysis patient survival is controversial. These drugs may have positive effects on residual renal function, vascular access and the uraemic myocardium7, which in turn may be reflected in better survival8, although other studies have not been able to demonstrate this benefit9.
The association between ACEI/ARBs use in pre-dialysis and survival in PD and HD patients is an original result of this study. A hypothesis to explain these findings may be based on a potential survival bias, that is, patients who required, tolerated and survived treatment with ACEI/ARBSs in the pre-dialysis period form a select group with a greater probability of survival in dialysis. However, this hypothesis seems unlikely, since we also observed better pre-dialysis survival in those treated with ACEI/ARBs (observations not published).
Another hypothesis to explain this delayed association may be related to a “legacy effect”. This term was originally coined to describe the positive effect of good metabolic control during the initial stages of diabetes on the subsequent outcome and its complications. There has also been speculation about the possibility that this same legacy effect could be achieved with the control of high blood pressure or with the use of ACEI/ARBs11, which is a benefit of survival that could be maintained beyond drug interruption, and it is therefore more difficult to appreciate it clinically.
Metabolic acidosis in CKD has negative effects on the state of nutrition, mineral and bone disease and inflammation, and is associated with worse survival12. The correction of acidosis with sodium bicarbonate has demonstrated not only that it improves the state of nutrition, but that it also has very positive effects on maintaining renal function.
In this study, the correction of acidosis with sodium bicarbonate was independently associated with better survival in dialysis. However, the potential confounding by indication also prevented the causality of this association from being confirmed. Some confounding factors that may influence this association are the decreased tendency for acidosis of diabetic patients with CKD13, or the association between acidosis and treatment with ACEI/ARBs due to type IV renal tubular acidosis or the impossibility of prescribing antacids in those who were treated for a brief period of time in the ACKD clinic. All of these confounding variables were taken into account in the multivariate regression analyses (diagnosis of diabetes, ACEI/ARB treatment and pre-dialysis follow-up time), and treatment with bicarbonate maintained statistical significance.
Starting HD with an IAVF improved vital prognosis14. According to these studies, we also observed better survival in patients with a functioning IAVF at the start of HD, and this association was independent of other confounding factors (age, sex, comorbidity, drugs, etc.)
Although the causes of death in those who initiated HD with or without IAVF were not significantly different, a greater percentage of deaths due to infection was observed, perhaps in relation to the more frequent use of endovascular catheters.
The renal function with which these patients started dialysis was another determining factor of survival, but to the contrary of what was expected, the association was negative. In accordance with observations of other authors15, it is likely that a higher glomerular filtration rate at the start of dialysis reflects a poor general patient condition, higher intolerance to uraemia, especially that related to states of over-hydration and the development of heart failure. It is also important to point out that when a patient from our study required the (urgent) non-scheduled initiation of dialysis due to any of these complications, the renal function figure that was taken was that of the last scheduled test, and therefore, this higher glomerular filtration rate would not reflect real renal function at the time of the first dialysis session.
This study has limitations mainly derived from the aforementioned confounding biases (indication and survival). Although the effect of these biases aims to correct itself by stratification and adjustment of the models with the main confounding variables, we cannot rule out the possibility of other variables that we have not considered having a significant influence on the end results.
Another limitation is that all patients studied were from the same hospital, with certain treatment criteria, which prevents us from guaranteeing the reproduction of the results with different treatment criteria.
In conclusion, there are differences in pre-dialysis treatments of patients who survive or die on dialysis. The most significant differences in models that are stratified to the type of dialysis and to the main confounding factors are: treatment with ACEI/ARBs, treatment with sodium bicarbonate and having a usable IAVF at the time of the first HD session.
These results suggest a potential delayed benefit (legacy effect) of some treatment in pre-dialysis stages on the subsequent evolution of dialysis patients. In addition, starting HD without an IAVF, with the resulting need for intravenous catheters, could be related to worse prognosis.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. Clinical characteristics and treatments received by patients included in the study
Table 2. Clinical characteristics and treatments received by patients who survived or died during the study period
Table 3. Cox multivariate regression models on mortality in dialysis
Figure 1. Kaplan-Meier survival curves in patients who started haemodialysis or peritoneal dialysis.
Figure 2. Causes of death according to the dialysis type, or some pre-dialysis treatments, or the availability of an arteriovenous fistula in those who started haemodialysis.
Figure 3. Kaplan-Meier survival curves in patients who started peritoneal dialysis and were treated or not with angiotensin-converting enzyme inhibitors and/or angiotensin receptor blockers.
Figure 4. Kaplan-Meier survival curves in patients who started haemodialysis and were treated or not with angiotensin-converting enzyme inhibitors and/or angiotensin receptor blockers.
Figure 5. Kaplan-Meier survival curves in patients who started haemodialysis and had or did not have a functioning arteriovenous fistula.