In dialysis patients, there are only 3 mechanisms of phosphate control: (1) elimination of phosphate by dialysis, (2) chelating therapy, and (3) dietary restrictions. Phosphate elimination by dialysis has been shown to be useful but insufficient, while the other two mechanisms require patients to follow the prescribed treatment.1
Failure to follow treatment in chronic patients is very common, multifactorial and involves factors related to the patient, the disease, the health system and the medication itself.2 Non-compliance with medication is even more striking with chelators, and is possibly the leading cause of lack of phosphate control.3,4 Various studies show that phosphate control improves with educational strategies, improving adherence to dietary and medication recommendations.5–7 Despite the high prices of new, more effective chelators, very few studies have addressed the economic aspects deriving from potencial saving associated with improved compliance.
We want to determine whether educational activities improved compliance with medication and phosphate control and evaluate whether this is associated with a lower need for binders and savings in pharmaceutical expenditure.
In a population of haemodialysis and peritoneal dialysis patients, we measured the degree of phosphate control, the level of adherence to medication on 2 different scales (8-item Morisky and SMAQ),8,9 knowledge about diet and treatment through a 6-item survey, the need for binders in each patient measured as the number of binders and dose prescribed of each binder (calcium carbonate/acetate, aluminium hydroxide, sevelamer hydrochloride/carbonate and lanthanum carbonate). The adherence using scales previously validated in chronic and dialysis patients. The scales classify patients as compliant and non-compliant, and also provide values that allows to be used as a continuous variable, assigning a score for each of the items including questions asked in the form of the Likert scale. The Morisky scale assigns a higher score a better adherence, while the SMAQ scale assigns a lower score to a better the compliance.
We conducted an educational activity as workshop in which we addressed the clinical consequences of uncontrolled phosphate, identification of chelating medication, appropriate methods of administration, identification of foods with a high phosphate content and how to reduced their intake.10
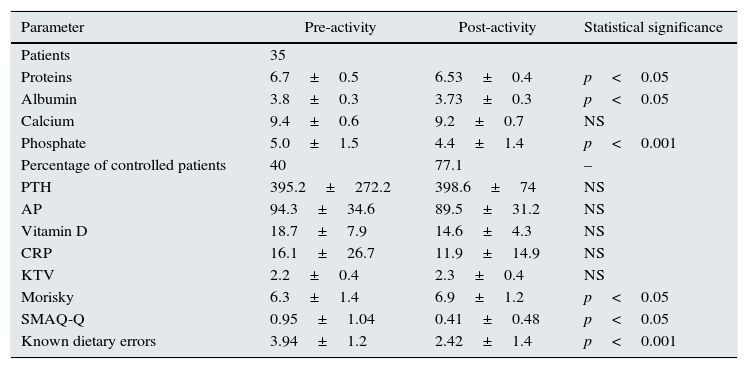
Three months after, we re-measured all of the parameters mentioned. We collected data from 35 patients with a mean age of 59.37±14.9, 18 on haemodialysis (HD) and 17 on peritoneal dialysis (PD), 43% female, 47% diabetic, with a time on dialysis of 54.37±82.9 months. The results of the study are shown in Table 1. Phosphate levels were significantly reduced (5.0±1.5 vs. 4.4±1.4). The percentage of patients with phosphate controlled rose from 40 to 71%. We observed no change in any other biochemical parameters except a negligible reduction in protein and albumin levels. The compliance with pharmacological treatment improved as measured by Morisky, as did the compliance of chelators measured by SMAQ. The number of errors in the knowledge test also improved significantly.
Change in parameters after educational activity.
| Parameter | Pre-activity | Post-activity | Statistical significance |
|---|---|---|---|
| Patients | 35 | ||
| Proteins | 6.7±0.5 | 6.53±0.4 | p<0.05 |
| Albumin | 3.8±0.3 | 3.73±0.3 | p<0.05 |
| Calcium | 9.4±0.6 | 9.2±0.7 | NS |
| Phosphate | 5.0±1.5 | 4.4±1.4 | p<0.001 |
| Percentage of controlled patients | 40 | 77.1 | – |
| PTH | 395.2±272.2 | 398.6±74 | NS |
| AP | 94.3±34.6 | 89.5±31.2 | NS |
| Vitamin D | 18.7±7.9 | 14.6±4.3 | NS |
| CRP | 16.1±26.7 | 11.9±14.9 | NS |
| KTV | 2.2±0.4 | 2.3±0.4 | NS |
| Morisky | 6.3±1.4 | 6.9±1.2 | p<0.05 |
| SMAQ-Q | 0.95±1.04 | 0.41±0.48 | p<0.05 |
| Known dietary errors | 3.94±1.2 | 2.42±1.4 | p<0.001 |
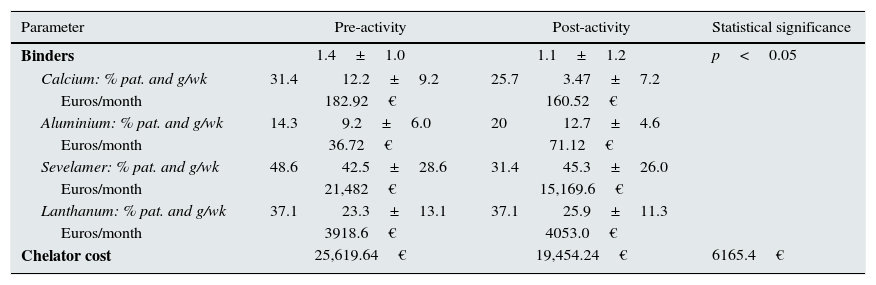
This improved control of phosphate led to a reduction in the number of binders and in the dose prescribed. The change in chelator dose and monthly expenditure is shown in Table 2. The number of binders an the dose prescribed per patient was reduced especially in calcium and sevelamer binders. The monthly savings in the treatment of 35 patients was over 6000 euros, and with a better control of serum phosphate.
Changes in binders treatment after educational activity.
| Parameter | Pre-activity | Post-activity | Statistical significance | ||
|---|---|---|---|---|---|
| Binders | 1.4±1.0 | 1.1±1.2 | p<0.05 | ||
| Calcium: % pat. and g/wk | 31.4 | 12.2±9.2 | 25.7 | 3.47±7.2 | |
| Euros/month | 182.92€ | 160.52€ | |||
| Aluminium: % pat. and g/wk | 14.3 | 9.2±6.0 | 20 | 12.7±4.6 | |
| Euros/month | 36.72€ | 71.12€ | |||
| Sevelamer: % pat. and g/wk | 48.6 | 42.5±28.6 | 31.4 | 45.3±26.0 | |
| Euros/month | 21,482€ | 15,169.6€ | |||
| Lanthanum: % pat. and g/wk | 37.1 | 23.3±13.1 | 37.1 | 25.9±11.3 | |
| Euros/month | 3918.6€ | 4053.0€ | |||
| Chelator cost | 25,619.64€ | 19,454.24€ | 6165.4€ | ||
Patient education and therapeutic alliance in the prescription process are not only effective, but also cost-effective. To be effective educational strategies need to be uninterrupted. It is evident that educational activities directed to patients are needed; these activities should have a multidisciplinary approach including doctors, dietitians and nutritionists capable of planning and carrying out these training activities on an ongoing basis, is daily more evident. If educating just 35 patients produces a monthly saving of 6000 euros, how much could be saved by improving the education of all patients on chelation, diet, potassium, interdialytic weight gain, etc.?
Please cite this article as: Rodriguez-Palomares JR, Japaz Cancino MC, Blazquez Collado L, Fiallos Criollo R, Villabon Ochoa PM, Sanchez Heras M, et al. Las estrategias de educación a pacientes son coste efectivas: reduzca el fósforo ahorrando 200€ al mes por paciente. Nefrología. 2017;37:103–105.