Introducción: En los últimos años, la enfermedad renal crónica (ERC) se ha llegado a considerar una epidemia, por lo que se ha prestado un gran interés a su diagnóstico precoz, con la finalidad de frenar su progresión a nefropatía terminal (NT) y preparar con tiempo a los pacientes para programas de diálisis y trasplante. Muchos ancianos son etiquetados de enfermos renales crónicos basándose únicamente en un filtrado glomerular estimado < 60 ml/min. Objetivo: realizar un seguimiento clínico de la función renal (FR) y de los pronósticos asociados a la ERC (morbilidad, mortalidad, desarrollo de NT) en ancianos. Pacientes y métodos: 80 pacientes clínicamente estables con mediana de edad de 83 años (rango 69-97); 69% mujeres, 35% diabéticos, 83% hipertensos; fueron reclutados aleatoriamente en las consultas externas de Geriatría y Nefrología entre enero y abril de 2006, y seguidos durante 5 años. En el reclutamiento establecimos dos grupos según la concentración de creatinina plasmática (Crp) basal (mg/dl): grupo 1: 38 pacientes con Crp ≤ 1,1 (rango 0,7-1,1) y grupo 2: 42 pacientes, con Crp > 1,1 (rango 1,2-3). Medimos en sangre Crp, urea, y estimamos filtrado glomerular con MDRD abreviado, basalmente y a los 5 años. Registramos la comorbilidad basal con el índice de Charlson (ICH), los ingresos, los eventos cardiovasculares de novo, los tratamientos, el desarrollo de NT que requiera diálisis y la mortalidad. Resultados: En los 39 pacientes que sobrevivían a los 5 años no hubo diferencias significativas entre los grupos 1 y 2 en número total de ingresos, episodios de insuficiencia cardíaca y cardiopatía isquémica de novo. Globalmente los diuréticos siguen siendo los fármacos más empleados (76,9%), y los betabloqueantes, los menos (10,3%). Fallecieron 41 pacientes (51,3%): 15 por deterioro del estado general, 8 por infecciones, 4 por ictus, 4 por tumores, 3 por causas cardiovasculares, 2 por complicaciones de fracturas y 5 por causas desconocidas. La mortalidad fue superior en el grupo 2 (66,7 vs. 34,2%; p = 0,004). La edad de los fallecidos era mayor (84,73 ± 5,69 vs. 80,12 ± 6,5, p = 0,001). No existieron diferencias significativas en la mortalidad atribuibles a género, diabetes, hipertensión arterial e ICH. Sólo dos pacientes del grupo 2 progresaron a NT realizando ambos tratamiento conservador debido a su comorbilidad (ningún paciente del estudio ha iniciado diálisis). La evolución de FR (basal/5 años) del conjunto de pacientes que sobreviven a los 5 años fue: Crp (mg/dl): 1,15 ± 0,41/1,21 ± 0,49 (no significativa [ns]); urea (mg/dl): 52,21 ± 13,0/61,21 ± 27,0 (p = 0,047); MDRD (ml/min/1,73 m2): 57,47 ± 15/54,86 ± 17 (ns); no existían diferencias en la evolución entre ambos grupos. En el análisis de regresión logística para mortalidad global (variables independientes: edad, género, ICH, antecedentes cardiovasculares, Crp y grupo) sólo la edad (riesgo relativo [RR]: 1,12; 1,03-1,23; p = 0,009) y el grupo (RR: 3,06; 1,10-8,40; p = 0,031) se asociaban independientemente con la mortalidad. Conclusión: El screening de la ERC, basado únicamente en el grado de filtrado glomerular, podría carecer de relevancia clínica en este grupo poblacional: la FR se deteriora lentamente en los ancianos sin proteinuria. La mortalidad global es mayor en los ancianos con peor grado de FR basal, superando el pronóstico de progresión de ERC a NT.
Introduction: In recent years, chronic kidney disease (CKD) has come to be considered an epidemic problem, and there is considerable interest in early diagnosis in order to slow its progression to end-stage renal disease (ESRD) and prepare patients for dialysis and transplantation programmes. Many elderly patients are labelled as having CKD based solely on having a glomerular filtration rate (GFR) of <60 ml/min. Objective: Monitor renal function (RF) and outcomes associated with CKD (morbidity, mortality and progress to ESRD) in an elderly cohort. Patients and method: A total of 80 clinically stable patients, with a median age of 83 years (range 69–97; 69% female, 35% diabetic, 83% hypertensive) were recruited at random in our Geriatric Medicine and Nephrology Departments between January and April 2006, and monitored for 5 years. During the recruitment stage we established two groups based on baseline serum creatinine (SCr) concentration: Group 1, 38 patients with SCr <1.1mg/dl (range 0.7-1.1) and Group 2, 42 patients with SCr >1.1mg/dl (range 1.2–3). We determined baseline blood levels of creatinine and urea, calculated eGFR using an abbreviated Modification of Diet in Renal Disease (MDRD) formula, and repeated these measurements after 5 years. We recorded baseline comorbidity according to the Charlson comorbidity index (CCI); hospital admissions; new cardiovascular events; treatments; progression to ESRD requiring dialysis; and mortality. Results: In the 39 patients surviving after 5 years there were no significant differences between Groups 1 and 2 in total number of hospital admissions, episodes of heart failure and new ischaemic heart disease. Overall, the most commonly used drugs were diuretics (76.9%), while beta-blockers were used the least (10.3%). There were 41 deaths (51.3%): of these patients, 15 died due to overall decline, 8 due to infections, 4 due to stroke, 4 due to neoplasia, 3 due to cardiovascular problems, 2 due to complications from fractures and 5 due to unknown causes. Mortality was higher in Group 2 (66.7% vs 34.2%, P=.004) and patient age was also higher in that group (84.73±5.69 vs 80.12±6.5, P=.001). No significant differences in mortality were attributable to sex, diabetes, hypertension or CCI. Only 2 patients in Group 2 progressed to ESRD, they received conservative treatment due to comorbidity (no patients in the study have started dialysis). The evolution of RF (baseline/5 years) in all patients surviving at 5 years was as follows: SCr (mg/dl): 1.15±0.41/1.21±0.49 (not significant [NS]), urea (mg/dl) 52.21±13.0/61.21±27.0 (P=.047), MDRD (ml/min/1.73m2) 57.47±15/54.86±17 (NS). There were no differences in progression between the 2 groups. In the logistic regression analysis for overall mortality (independent variables: age, sex, CCI, cardiovascular history, SCr and group), only age (relative risk [RR]: 1.12; 1.03-1.23, P=.009) and group (RR: 3.06; 1.10-8.40, P=.031) were independently associated with mortality. Conclusion: Screening for CKD using GFR only may lack clinical relevance in this population since RF slowly deteriorates in elderly patients without proteinuria. Mortality due to all causes was higher in elderly patients with a poorer baseline RF, and mortality rates were higher than rates of CKD progression to ESRD.
INTRODUCTION AND OBJECTIVES
CKD has been considered a public health problem ever since the NKF (National Kidney Foundation) and KDIGO (Kidney Disease: Improving Global Outcomes) introduced a definition and classification method for chronic kidney disease (CKD) judged to be applicable to the entire population.1,2 For this reason, doctors now show considerable interest in early detection of CKD, in order to take actions to slow its progression to end-stage renal disease and have enough time to prepare patients for dialysis and transplant programmes where necessary.3
In general, we are taught that after the age of 30, glomerular filtration rate (GFR) decreases at a mean rate of 1ml/min/year. The Baltimore longitudinal study of aging, which included 254 healthy volunteers, found that the mean decrease in creatinine clearance was 0.75ml/min/year.4 At present, and as stated in KDOQI guidelines, CKD prevalence is high, particularly in the elderly. This has led to widespread debate among nephrology professionals, who disagree about whether or not decreased GFR in this population may show the physiological ageing process rather than intrinsic kidney disease.5,6
Additionally, elderly patients often present certain comorbidities associated with CKD, such as atherosclerosis, heart failure (HF), high blood pressure (HBP), diabetes mellitus (DM) and cognitive deterioration which may all affect the CKD prognosis.7,8
Objectives of this study were as follows: 1) analyse how CKD progresses from baseline renal function (RF) (rapid progression is considered to be a decrease ≥4ml/min/year9); 2) analyse main outcomes associated with CKD: progression to stage 5 CKD requiring renal replacement therapy (RRT) and mortality; and 3) study associated mortality by analysing hospital admissions, the appearance of new cardiovascular events and indicated treatments.
PATIENTS AND METHODS
Patients
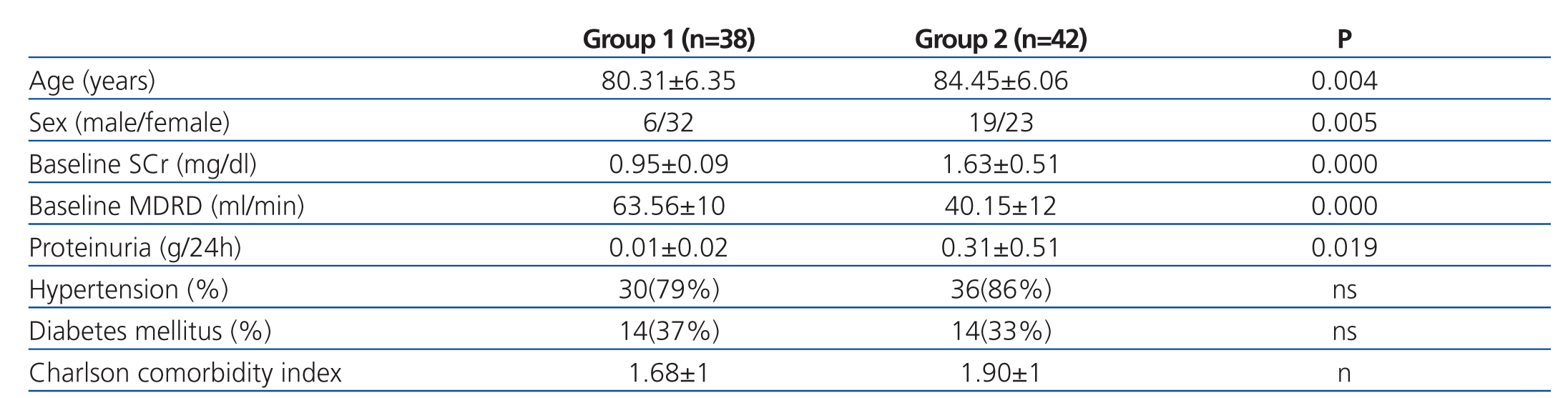
We studied 80 clinically stable patients with a median age of 83 years (range: 69-97 years), who were randomly recruited during scheduled outpatient check-ups with the Geriatric Medicine and Nephrology departments between January and April 2006. According to baseline serum creatinine (SCr) levels, we established two groups: Group 1, n=38, SCr ≤1.1mg/dl (range 0.7-1.1) and Group 2, n=42, SCr >1.1 mg/dl (range 1.2-3). Of the total, 55 patients (69%) were female; 28 (35%) had DM and 66 (83%) had HBP. Socio-demographic characteristics, RF and baseline comorbidity for both groups are shown in Table 1.
Patient distribution by CKD stage (using the abbreviated MDRD formula) for the baseline period was as follows: stage 1: 0%; stage 2: 30%; stage 3: 60%; stage 4: 10%; stage 5: 0%.
Method
Observational analytical cohort study. The first evaluation was completed at the time of the patient’s scheduled visit during the period between January and April 2006. All of the elderly patients underwent laboratory and clinical monitoring during 5 years, and were re-evaluated during the January - April 2011 period.
Laboratory analyses were completed as a baseline measurement one week before patients came in for scheduled visits with Geriatric Medicine or Nephrology departments, and they were repeated once again after 5 years. Creatinine and urea levels were measured in venous blood according to the routine method used at Hospital General de Segovia. Systematic urine analysis was completed for all patients to screen for proteinuria; additionally, for Group 1, the protein/creatinine ratio (mg/dl) was measured in a single morning void. In Group 2, the urine protein count was measured in a 24 hour sample. In the baseline period, the systematic analysis detected no proteinuria in Group 1 and the urine protein/creatinine ratio was <0.05g. In Group 2, baseline proteinuria was 0.31±0.51g/24 hours (range 0-3.0g/24 hours): 87% of Group 2 patients had proteinuria <0.5g/24 hours; 5.2% had values between 0.5g and 1g/24 hours; and 7.8%, between 2g and 3g/24 hours. GFR was estimated using the abbreviated MDRD formula.10
Baseline comorbidity was calculated using the Charlson comorbidity index (CCI) without including age.11 We also recorded hospital admissions, appearance of new cardiovascular events (HF, ischaemic heart disease; stroke) and drugs taken during the 5 year period. With regard to the CKD prognosis, we evaluated 1) changes in RF over the 5 year period in patients who remained in the study; 2) patients who progressed to ESRD and began RRT; and 3) mortality and its causes.
Statistical analysis
Statistical analysis was performed using SPSS software version 15.0. Data are expressed as percentages, means and standard deviations. Changes in RF over time were evaluated using a linear model for repeated measures. Proportions were compared using chi-square (Fisher’s test). Variables predicting mortality were analysed using logistic regression analysis. The statistical significance level was 95% (P<.05).
RESULTS
After 5 years of follow-up, 39 patients (including 10 males) with a mean age of 84.94±6 years (74-101) remained in the study. Only 2 patients (5.1%), both in Group 2, (SCr>1.1mg/dl), were taking erythropoiesis-stimulating agents (ESA); 5 (12.8%) were treated with iron salts; 10 (25.6%) with calcium salts and 12 (30.8%) with statins. Diuretics were the most commonly-used anti-hypertensive agents (76.9%) and most were loop diuretics (48.7%). Angiotensin-converting enzyme (ACE) inhibitors were prescribed for 35.9% of the patients; and angiotensin II receptor blockers (ARB) and calcium blockers for 20.5%, respectively. Beta-blockers were the least commonly-used antihypertensive agents, prescribed for 10.3% of these patients. There were no significant differences between the 2 groups with regard to prescriptions for ESA, iron salts, calcium salts, statins, diuretics, ACE inhibitors, ARB, calcium blockers or beta blockers. Systolic blood pressure (BP) recorded after 5 years was 128.83±13mm Hg (100-160); and diastolic BP 70.56± 10mm Hg (50-95).
During the study period, 60% of the patients were admitted to hospital at least once. Regarding new cardiovascular events, 20.3% of the patients had an episode of HF, 7.5% suffered a stroke and 6.3% suffered IHD. If we compare new cardiovascular events between the 2 groups, we find the following: in Group 1, 13.5% of patients suffered from an HF episode and in Group 2, 26.8% suffered 1 or more episodes; ischaemic heart disease was present in 5.3% of Group 1 patients and in 7.3% of Group 2 patients; and a stroke episode occurred in 11.5% of Group 1 patients and in no patients in Group 2. These differences were not statistically significant.
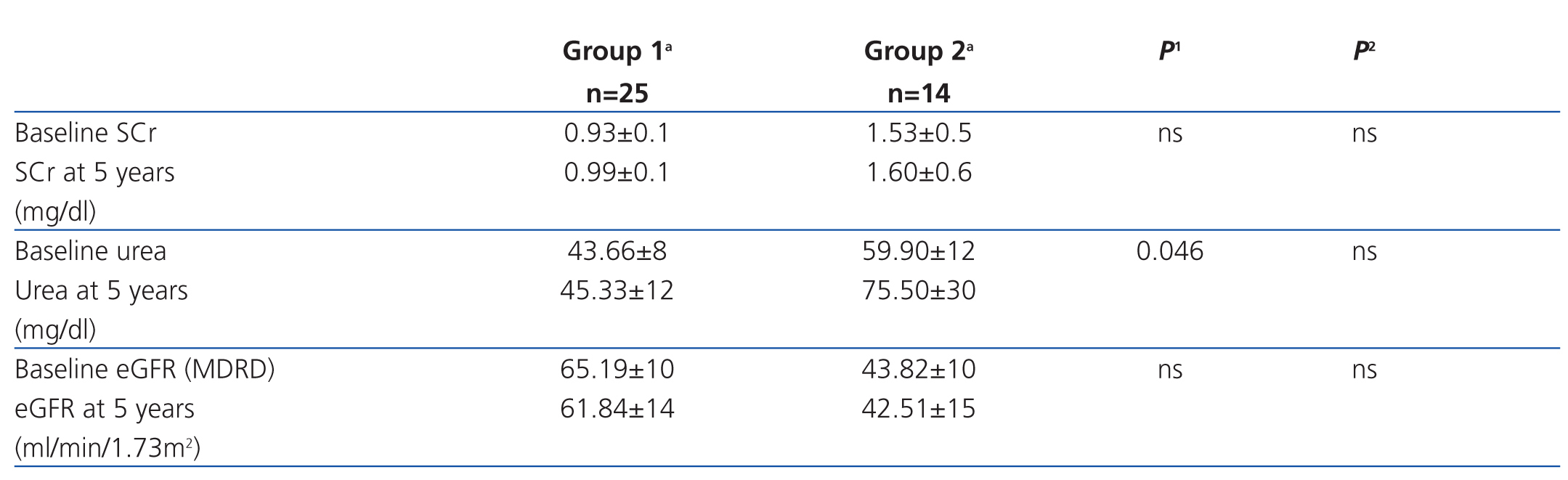
Overall data regarding changes in RF (baseline/5 years) in surviving patients were as follows: SCr (mg/dl): 1.15±0.41 vs 1.21±0.49 (not significant [ns]); urea (mg/dl) 52.21±13.0 vs 61.21±27.0 (P=.047); MDRD (ml/min/1.73 m2): 57.47±15.0 vs 54.86±17.0 (ns). Changes in RF by group are shown in Table 2. Among all surviving patients, GFR decreased at a mean rate of 0.52ml/min/year. When this parameter was broken down by group, we found that in Group 1 (baseline creatinine ≤1.1) the mean decrease was 0.67ml/min/year, compared to 0.26ml/min/year in Group 2.
Only 2 patients, both in Group 2, progressed to ESRD, but neither case started RRT. Conservative treatment was administered in the first case according to the patient's own decision, and the second patient was not included in a RRT programme due to advanced age (89 years) and high comorbidity (patient had undergone surgery for meningioma, was in a wheelchair and had a bladder neoplasm). Both patients died during the study period.
Regarding overall mortality, 41 patients (51.3%) died during the 5 year follow-up period: there were 15 deaths due to general decline, 8 due to infections, 4 due to stroke, 4 due to neoplasia, 3 due to cardiovascular problems, 2 due to complications from fractures and 5 due to unknown causes. Causes of mortality broken down by group are listed below. Group 1: 4 due to general decline, 4 due to infections, 2 due to stroke, 1 due to cardiovascular problems, 1 due to neoplasia and 1, unknown. Group 2: 11 due to general decline, 4 due to infections, 2 due to stroke, 3 due to neoplasia, 2 due to cardiovascular problems, 2 due to complications from fractures and 4, unknown. A comparison of baseline comorbidities of patients who died found no significant differences between the 2 groups. Mortality was higher in Group 2 (66.7 vs 34.2%; P=.004). Patients who died were also older (84.73±5.69 vs 80.12±6.5; P=.001). There were no statistically significant differences in mortality related to sex, presence/absence of DM or HBP or baseline CCI. Logistic regression analysis for overall mortality (independent variables: age, sex, CCI, history of cardiovascular disease, baseline SCr and group) showed that only age (relative risk [RR]: 1.12; 1.03-1.23; P=.009) and group (RR: 3.06; 1.10-8.40; P=.031) were independently associated with mortality.
DISCUSSION
The main findings of this study are as follows: 1) the GFR in elderly patients in this study remained stable or decreased slowly over the 5 year follow-up period, regardless of baseline GFR; 2) we did not find statistically significant differences that could be attributed to baseline GFR regarding new cardiovascular events or treatment received during the 5 year follow-up; 3) almost no patients progressed to stage 5 CKD; 4) mortality was significantly higher among Group 2 patients (SCr >1.1mg/dl). It was associated with older patients, and seemed to be independent from all other comorbidities.
In our follow-up reports for these patients at 24 months and 36 months,12,13 we stated that RF remained stable or decreased slowly over time. Our follow-up report at 5 years confirms prior conclusions: RF decreases slowly in elderly patients, and most die before progressing to RRT-dependent ESKD.
Overall, the mean decrease in GFR was 2.61ml/min over the 5 years of follow-up covered by our study. In the analysis broken down by group, we find a slight, non-significant decrease in GFR over time, but there is an interesting paradox: Group 1 patients (those with SCr levels within the normal range) showed a greater decrease in GFR (ml/min/year) than Group 2 patients, who had a poorer baseline GFR. A possible explanation is that the decline in Group 1 simply represents the physiological phenomenon of GFR decreasing with age, while rates in Group 2 remained almost constant since patients whose GFR declined sharply died and patients whose GFR was more stable survived.
In recent years, increased demand for RRT (dialysis or transplant) has sparked interest in the early detection of CKD.14 In fact, one of the goals of early detection is to initiate preliminary treatments to slow the rate of CKD progression to stage 5, and prepare patients for RRT where appropriate. Nevertheless, these objectives seem less clear for the elderly population, as the vast majority are not going to receive specific preparation for RRT. This may be due to the patient’s own decisions, doctors’ decisions based on the comorbidities associated with RRT that may contraindicate such treatment (neoplasia, cognitive deterioration, etc.), or death. Some preliminary studies have shown that risk of death is higher than the risk of reaching ESRD: for example, the study by Eriksen and Ingebretsen15 reported a 31% mortality rate, while only 2% of their patients started RRT. In our elderly population, we also recorded high mortality rates (more than 50% at 5 years) and noted that patients died before reaching ESRD and/or requiring RRT (only 2 patients reached ESRD and neither one was included in the RRT programme).
Patients with a poorer baseline RF (Group 2) had significantly higher mortality rates in our study. A possible explanation is that these patients, in addition to having poor baseline RF, were significantly older. In fact, logistic regression analysis found an association between age and mortality that was independent from the group; progressive decline was the leading cause of death in this cohort, and not cardiovascular disease (which is the primary cause of death in CKD patients in general).16,17 For this reason, the high mortality rates recorded among elderly patients with poor GFR support the need to provide overall treatment, even if kidney function is not the key factor on which their survival depends.
Regarding morbidity, 60% of the total patients were hospitalised at least once. HF was the main cardiovascular event (followed by ischaemic cardiopathy and stroke). Although differences were not statistically significant (either due to the low number of patients evaluated or the period of time in question), Group 2 patients experienced more HF episodes during follow-up.
Diuretics are drugs that aid in BP control and have the added benefit of preventing HF episodes. In our study population, diuretics were the main anti-hypertensive agents prescribed (76.9%); however, 20% of patients presented 1 or more HF episodes. In addition to preventing HF, use of diuretics may increase SCr values due to the volume depletion associated with use of such drugs, as we reported in a previous study.18 Treatment with diuretics is therefore a factor that must be considered when evaluating CKD in elderly patients: the same patient may be categorised in different stages of CKD depending on whether he or she was taking diuretics when SCr and GFR (MDRD) were measured.
Proteinuria is the main sign of kidney injury.19 In our study, Group 1 patients had no proteinuria at the time of the baseline measurement, and more than 80% of Group 2 patients had proteinuria levels below 0.5g/24h. Only 14 patients in Group 2 were still in the study 5 years later, and this number is too low to allow us to reach any conclusions regarding the prognostic value of proteinuria. In fact, we believe that our assessment at 36 months was more reliable.13 At that time, we showed that patients with proteinuria were the ones whose renal function deteriorated the most over time, and that proteinuria and age were the main variables associated with mortality.
In conclusion, CKD screening based solely on GFR may have no clinical relevance in these patients since GFR decreases slowly over time in elderly patients without proteinuria. Patients with poorer baseline GFR do not present an increased risk of new cardiovascular morbidity and mortality, although their overall mortality rate is higher, particularly in the very old ones. The risk of mortality is higher than the risk of progressing from CKD to ESRD. Based on these findings, we recommend caution when applying current guidelines to elderly patients.
Conflicts of interest
The authors affirm that they have no conflicts of interest related to the content of this article.
Table 1. Socio-demographic characteristics, renal function and baseline comorbidities by group
Table 2. Changes in renal function by group among patients surviving at 5 years of follow-up