To the Editor:
There is a general consensus about the importance of a personalised follow-up in consultations of patients with advanced renal failure and it has been recognised for years as a good prognosis factor in the progression of these patients.1,2 We summarise our experience, evaluating some of the normal parameters in our study group. Currently, the preparation of a patient who is close to beginning renal replacement therapy is a fundamental tool. Our objective is to share our experience in this regard and to compare the results of the most common clinical and biological parameters, according to age groups and the modified Charlson index.3
The group reviewed corresponds to 98 patients assessed for this type of consultation in 2012. We assessed the overall distribution by age, sex, type of nephropathy, previous preparation for renal replacement therapy (vaccination, their response, vascular access, etc.) and standard biological markers. We then compared the aforementioned parameters according to age group and the Charlson index. The mean age of the group was 67.35 and the median was 69, with a majority of males (2/3). The median of the modified Charlson index was 6 and the mean, 6.5. The types of nephropathy were grouped by order of frequency into nephroangiosclerosis, diabetic nephropathy, unknown origin, glomerulonephritis, polycystic kidney disease, obstructive uropathy and others, as expected. The hepatitis B vaccination was administered in 86% of the patients and the rest was distributed amongst those who had prior natural immunity and those in whom there was no time to initiate the process for one reason or another. We found 5% of non-respondents and 56% of respondents, with a high percentage of patients in the titration phase or who did not finish the required dose. Vascular mapping was required for arteriovenous fistulas and, if not possible, we scheduled the insertion of permanent catheters, which was carried out by nephrologists in our unit.
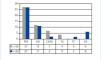
The observation of biological parameters (Table 1) was performed by reviewing the group's overall data divided into groups by age and the Charlson index. It was notable that very similar results were observed by comparing the results of both medians with the total population, which displayed better nutritional parameters and lower erythropoietin requirements in the theoretically better groups. Regarding the progression of patients, 54 remained in consultation, and the 44 remaining patients began some kind of renal replacement therapy (Figure 1). As expected, there was a higher rate of renal transplantation in younger patients and in those on continuous ambulatory peritoneal dialysis (CAPD). Four transplantations were performed, all in patients under 69 years of age; a total of 13 were included in the waiting list during the year, and all had a Charlson index below 6: 1 anticipated live donor transplantation, 2 in patients who started CAPD during the year and 1 from haemodialysis. There was a wide age range in patients selected for inclusion on the waiting list for renal transplantation in relation to a very high mean Charlson index of 7.92 in elderly patients. The mean age of the 6 patients who died and the 2 on conservative treatment was 79 and 86 years with Charlson indices of 9 and 11, respectively, for their multiple concomitant pathologies. Four of the 6 deaths occurred before the start of the clearance programme, whose indication was more than dubious. In patients younger than 69 years, no exitus was recorded, with a good renal transplant choice (13 already included on the waiting list and 15 under study) and CAPD.
These observations maintain our interest for the future of this consultation, and we can assess whether we are on the right track. Similarly, in this work we wish to be somehow examined by colleagues who are more experienced in this subject. The opportunity for direct and frequent contact with patients and their families may also open new avenues for renal patient care, with the possibility of choosing something as forgotten as haemodialysis at home.4
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. Overall biological parameters and by median of age and Charlson index
Figure 1. Final destination of period