Introducción: Se define la espiritualidad como la búsqueda personal de propósito y significado en la vida, pudiendo incorporar o no la religión. En este artículo se presenta el desarrollo y la aplicación de una medida de bienestar espiritual a una muestra de pacientes en hemodiálisis. Material y métodos: El instrumento básico empleado se denomina Cuestionario del Sentido de la Vida (Meaning in Life Scale, MiLS), con 21 ítems y cuatro escalas: Propósito, Falta de significado, Paz y Beneficios de la espiritualidad. También se proporciona una puntuación global de espiritualidad. Además, se registraron variables de tipo clínico (tiempo en hemodiálisis, índice de comorbilidad de Charlson) y sociodemográfico (edad, género), así como estimaciones del estado de salud, calidad de vida (general y actual), felicidad personal, el grado de religiosidad y la creencia en la existencia de vida ultraterrena. Se ha utilizado un diseño transversal con 94 pacientes en hemodiálisis. Resultados: Los resultados muestran que la versión española de este instrumento (MiLS-Sp) es una medida de bienestar espiritual con garantías psicométricas de calidad (fiabilidad, validez), adecuada para evaluar las complejas exigencias generadas por la problemática de salud del paciente en hemodiálisis. El bienestar espiritual se relaciona significativamente con diversas variables de calidad de vida, percepción de salud, felicidad personal o religiosidad. No existe una relación significativa entre las puntuaciones de espiritualidad y la edad, el sexo, el tiempo en diálisis o el índice de comorbilidad. El grado de bienestar espiritual de estos pacientes es relativamente bajo. Conclusión: La espiritualidad parece desempeñar un papel importante en el bienestar psicológico, el estado de salud y la calidad de vida percibidos por el paciente en hemodiálisis. El grado de bienestar espiritual de estos pacientes es relativamente bajo. Estos resultados sugieren que considerar y evaluar el grado de bienestar espiritual en los pacientes en hemodiálisis puede ser de utilidad para la práctica clínica.
Introduction: Spirituality can be defined as a personal search for meaning and purpose in life that may or may not encompass religion. In this article we report on the development and testing of an instrument for measuring spiritual well-being within a sample of haemodialysis patients. Material and Method: The main instrument, a 21-item Meaning in Life Scale (MiLS), comprises four scales: Life Perspective, Purpose and Goals, Confusion and Lessened Meaning, Harmony and Peace, and Benefits of Spirituality. A total score for spiritual well-being is also produced. We also used the following variables: clinical (time on haemodialysis, modified Charlson comorbidity index), sociodemographic (age, gender), and self-assessments of health, quality of life (general and recent), personal happiness, religiosity, and belief in the afterlife. A cross-sectional study was carried out on 94 haemodialysis patients. Results: This study demonstrates that the MiLS-Sp is a psychometrically sound measure of spiritual well-being for dialysis patients (reliability, validity) as they manage the complex demands of a chronic illness. Spiritual well-being was significantly associated with various quality of life variables, health status, personal happiness, or religiosity in patients on dialysis. There was no relationship between spirituality scores and comorbidity, HD duration, gender, or age. Spiritual well-being is relatively low in dialysis patients. Conclusion: Spirituality may play an important role on psychological well-being, quality of life, and self-rated health for patients on haemodialysis. Spiritual well-being in these patients is relatively low. Results suggest that assessing and addressing spiritual well-being in dialysis patients may be helpful in clinical practice.
INTRODUCTION
When patients require periodical sessions of haemodialysis, the repercussions manifest not only in terms of the physical, psychological, and social performance of the patient; there are also several spiritual issues that must be addressed.1 Several different studies have demonstrated that spirituality is a fundamental need in these patients.2-4 Spirituality provides the means through which patients can question the meaning, significance, purpose, and direction of his/her life, disease, or suffering. In some cases, spirituality becomes one of the primary resources available to the patient for dealing with suffering, disease progression, and its consequences. Many researchers and doctors believe that, in any case, evaluating and prioritising spirituality are essential components of integrated, holistic therapy for patients with severe health problems or end of life situations. In many cases, patients on haemodialysis and their families turn to spirituality or religion as a fundamental resource for maintaining an optimistic outlook in these situations.5 In this context, it has been shown that spiritual well-being is related in a systematic and significant manner with quality of life, social support, level of satisfaction, decreased symptoms of depression, improved satisfaction with nephrological treatment, and higher survival rates.6-9 These patients enjoy spiritual well-being when they have a sense of purpose, coherence, and personal fulfilment in life, and when they retain the belief that life has value. In this sense, health professionals must recognise the existence of spiritual needs in their patients when applying high-quality, integrated health care, and should evaluate patient spiritual well-being to the extent possible.2,4,5
However, we are frequently presented with the problem that no consensus documents exist regarding the significance of spirituality and its association with, for example, religiosity. Religion is an important means for experiencing personal spirituality, but is not necessarily the only or most important pathway. Recent literature reviews show that the majority of experts indicate that spirituality refers primarily to an attempt to comprehend the sense and purpose of life, which may or may not incorporate religious practices, or the belief or lack thereof in the existence of a higher power.1,10
In Spain, we still lack an instrument for measuring spiritual well-being using high-quality criteria (practical feasibility, reliability, and validity). With this in mind, our group started a research project, using a systematic literature review after the recent studies by Vachon et al.11 and Brandstätter et al.,12 to choose a proper instrument for measuring spiritual well-being that could be adapted to the particularities of our society and culture, and that would evaluate spirituality as the perception that one’s life has meaning, value, significance, and purpose. As a result, we expected patients to experience a feeling of inner peace and personal equilibrium, reporting personal benefit from the experience of their own spirituality.12,13
The objective of our study was to adapt, describe, and validate a multi-dimensional, standardised, and self-administered instrument for measuring spiritual well-being in a given patient or for specific situations. This instrument must include measurable quality guarantees (minimal strain on the interviewee, viability, feasibility, reliability, and validity) and be appropriate and useful for clinical practice in patients on haemodialysis. In addition to adapting and validating this questionnaire for measuring the level of spiritual well-being in patients on haemodialysis, we will explore the behaviour of responses in association with several variables of interest, both clinical (time on haemodialysis, comorbidity), sociodemographic, and psychological (age, sex, health self-assessment, level of religiosity, and indicators of quality of life).
METHODOLOGY
Design
Our study involved a cross-sectional design through the application of a questionnaire.
Materials and questionnaire
After performing an exhaustive review of instruments for quantifying spirituality that appear in scientific publications (for example, Vachon et al.,11 Brandstätter et al.12), our group unanimously selected the Meaning in Life Scale (MiLS).13 The MiLS questionnaire has been developed and validated taking into account the current theoretical models involving meaning of life and existential spiritualism, considering several different, inter-related dimensions, each of which contribute singularly to the construct of ”meaning”. The results provide empirical support for this concept of a meaning to life, as a unifying concept that synthesises the rich theoretical tradition of this field of study, and that allows for using the results of each of the four scales towards a global score for the total questionnaire. In this manner, the MiLS provides a significant improvement over previously existing measurement instruments, which provided very little in terms of psychometric values, evaluated a single aspect of the construct, or evaluated it exclusively within the context of negative experiences. If researchers of the spiritual dimension in these patients base their evaluations on their own methodologies, whether through qualitative interviews designed by other study groups or by developing their own questions, this magnifies the difficulty in coming to an empirical consensus and progressing with theoretical understanding. The adaptation of the MiLS into Spanish allows for profiting from the experience gained from the original study group, as well as establishing comparisons at an international level. The four different categories of the questionnaire are consistent with rigorous theoretical models and incorporate the most essential areas regarding self-transcendence and external transcendence. In this context, a systematic review of the instruments for the empirical measurement of spirituality carried out by Vachon et al.11 resulted in 11 distinct significant components that compose the structure of spirituality: meaning and purpose in life, self-transcendence, transcendence with a higher being, feelings of communion and mutuality, beliefs and faith, hope, attitude toward death, appreciation of life, reflection upon fundamental values, the developmental nature of spirituality, and conscious aspect. Of these, the most commonly used and important components were used in the development and validation of MiLS. These 11 dimensions have also allowed for developing a wider, more integrated, and complete definition of spirituality as a dynamic and conscious process characterised by two areas of transcendence: self-transcendence, and external transcendence.11
We made contact with the authors of the original version and requested the instrument in English as well as authorisation for adapting it into Spanish. This questionnaire evaluates a single and complete concept in the form of spirituality and life meaning, using 21 different questions in 4 different dimensions or spirituality scales derived from an exploratory and confirmatory factor analysis: (1) Life Perspective, Purpose and Goals (composed of 7 questions; Cronbach’s alpha: 0.90): measures the level of personal fulfilment and satisfaction with life felt by the patient in his/her current personal situation and reflects the patient’s level of commitment with activities, self-comprehension, and optimism for the future. (2) Lessened Meaning (composed of 7 questions; Cronbach’s alpha: 0.84): a scale indicating the loss or decrease in the value and worth of life, in terms of a loss of motivation to perform important functions, a sense of confusion regarding sense of self and life in general, and the belief that life is a negative experience. (3) Harmony and Peace (composed of 4 questions; Cronbach’s alpha: 0.87): scale that evaluates the level of inner peace and harmony, personal equilibrium, the experience of an inner feeling that provides happiness and a positive outlook, which establishes a sense of tranquillity, serenity, and comfort. (4) Benefits of Spirituality (composed of 3 items, Cronbach’s alpha: 0.91): evaluates the level of strength, fortitude, and consolation that religious faith or other spiritual beliefs that fall outside of a traditional religious framework may provide.
These questions are posed with the following instructions “The following affirmations refer to the impact that your disease may have caused in your life. Please indicate the level of agreement or disagreement with each item as it relates to you and your life at this moment.” The first two scales (Life Perspective, Purpose and Goals and Lessened Meaning) have six possible responses (from very much in disagreement to very much in agreement). The other two scales (Harmony and Peace and Benefits of Spirituality) have five possible responses (from not at all to very much), based on the level of concordance in each case with the 7 statements that compose items 15-21. These five alternatives were later scaled to 6 alternatives in order to evaluate the responses from these two scales together with those from the other scales in a single, combined analysis with comparable scoring systems.
In addition to the values for each scale, the MiLS provides a total score for Spirituality (21 items; Cronbach’s alpha: 0.93). This total score is obtained from the individual scores of each question with a positive response; to this end, the inverse is taken of values from the Lessened Meaning scale and item 15 (Harmony and Peace scale). At the same time, the questions with 5 possible responses are re-scaled to have 6 responses. A higher total spirituality score indicates a greater level of inner peace and harmony, a greater sense of purpose, fulfilment, and meaning in life, and greater perceived benefit from spiritual beliefs.
We used the same re-scaling procedure used by the original validation article13 as well as other questions of interest. In addition to the sociodemographic variables of sex and age, we analysed two clinical variables: comorbidity and time on haemodialysis. For the analysis of comorbidity, we used the most commonly accepted and internationally recognised scale, the Charlson index,14 as modified by Beddhu et al.15
Another six variables were used as criteria for evaluating the patient’s subjective well-being (health status, general quality of life, current quality of life, and personal happiness), as well as religious well-being (level of religiosity and belief in an afterlife). In order to evaluate health status, we posed the question: “In general, would you say your health is” (possible responses: excellent, very good, good, normal, bad). In order to evaluate general quality of life, we posed the question: “In general, would you say your quality of life is” (possible responses: very good, good, regular, bad, very bad). For the evaluation of current quality of life, we used number 9 from the COOP-WONCA questionnaire “how have things gone in the last few weeks?” (possible responses: Brilliant, couldn’t be better, quite good, sometimes good/sometimes bad, equally bad and good, quite bad, very bad, couldn’t be worse). In order to evaluate personal happiness, we posed the question: “in general terms, would you say you are very happy, quite happy, somewhat happy, or not at all happy?
These variables for evaluating patient well-being have proven their validity and relevance in the scientific literature, and these criteria have been analysed and tested by our group in previous studies.16-20 In addition, we analysed the level of patient religiosity and belief in an afterlife.
Method and procedure
With signed informed consent from all patients and the authorisation of the ethics committee at our hospital, two expert psychologists distributed the questionnaire during a haemodialysis session with the patient in a stable clinical condition. All other variables were collected from the patient’s clinical history. We compiled all data for the study between December 2010 and January 2011. Thirty-two patients (34%) required assistance in filling out the survey. In these cases, the assistance was given as per patient request or because connections to the dialysis machine impeded handwriting. The hospital personnel selected a consecutive sample of patients based on the following inclusion and exclusion criteria: patients were included in the study with an age >18 years, fluency in the Spanish language, and the desire to participate in the study, and were excluded if previously diagnosed with neurological, psychological, or mental retardation disorders, if they were unable to respond to the questionnaire due to comprehension problems, or if a deterioration in health required hospitalisation. Using these criteria, none of the patients that were contacted for participation in the study and accepted the informed consent were rejected from participating. The first phase of the survey was the MiLS-Sp, a multi-dimensional questionnaire composed of 21 different questions for evaluating spirituality and meaning of life as experienced by each patient at that point in time, as translated and adapted by our research group following the Brislin methdology21 for translation/back-translation of instruments from one language to another.
The second phase of the survey involved a series of questions regarding sociodemographic, clinical, and other variables related to patient well-being, both subjective and in terms of religiosity, which have been described in another section.
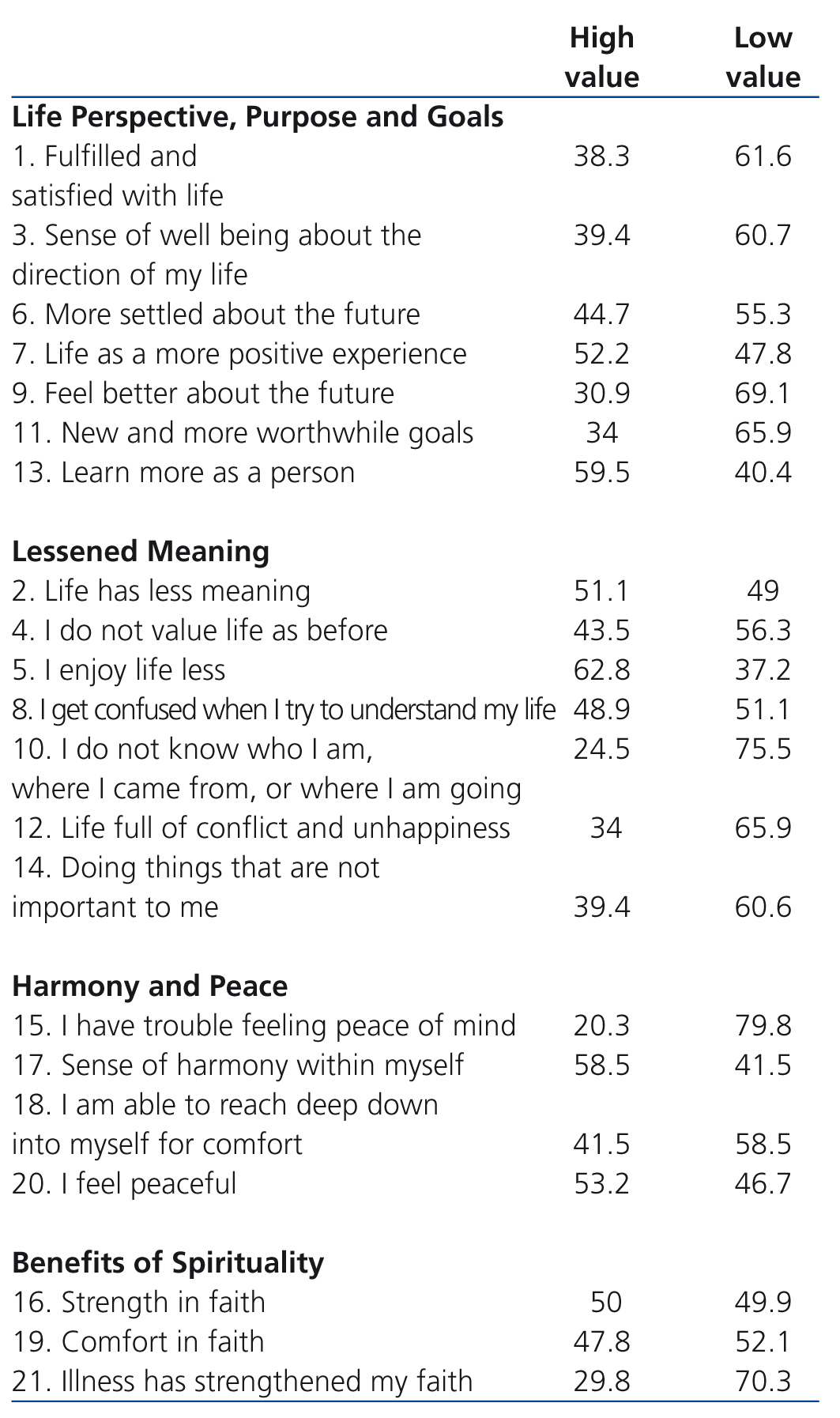
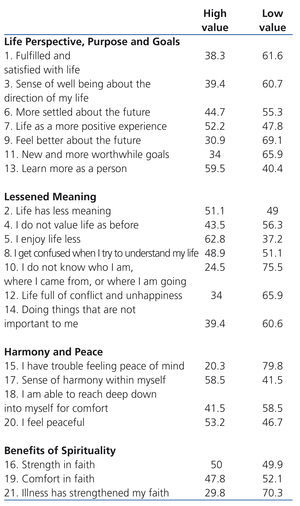
We analysed the study results using PASW statistical software, version 18. We performed a descriptive, correlational, and differential analysis statistics of the study variables. We also performed a grouping analysis that categorised each question as high-value or low-value. This categorisation of question responses produced two different groups: a high-value group (responses including somewhat in agreement, in agreement, and very much in agreement for questions 1-14, along with quite and very much for questions 15-21) and another low-value group (responses including somewhat in disagreement, in disagreement, and very much in disagreement for questions 1-14, along with not at all, very little, and somewhat for questions 15-21). In addition, we used two different types of score transformations for the analysis of questionnaire results. Firstly, we re-scaled all scores based on the recommendations from the creators of the instrument, and secondly, we standardised the direct questionnaire results to a scale of 0-10. For the first transformation, we took the inverse of the values for question 15 and for questions 15-21: 0=1.00, 1=2.25, 2=3.50, 3=4.75, and 4=6.00. In the second transformation, the direct score to be standardised has the lowest possible value on the scale subtracted from it, then is divided by the difference between the highest possible value and the lowest, and then this value is multiplied by 10.
Patients
A total of 94 patients on haemodialysis in the nephrology department of the Hospital Perpetuo Socorro (Alicante) participated in the study, with a mean age of 67 years (standard deviation [SD]: 13.4, range: 33-86; mode: 78; median: 69.5). Of these, 65% were male. The mean modified Charlson comorbidity index value was 7.37, with a median of 7 and a range of 2-14. The mean time on haemodialysis was 4.6 years (median: 3 years), with a minimum of 2 months and a maximum of 409 months.
RESULTS
Table 1 displays the different scales of the MiLS-Sp questionnaire along with an abbreviated list of the questions they are composed of. Also shown are the relative results of the sum of responses indicating some level of agreement (in percentages) for each of the items in the Life Perspective, Purpose and Goals and Lessened meaning scales, along with the sum (in percentages) of the responses quite and very much for the other two scales: Harmony and Peace and Benefits of Spirituality. This categorisation of the possible responses allowed for dividing responses into two large groups, referred to as high value (the three different measures of agreement along with quite and very much) and low value (the three different measures of disagreement, along with not at all, very little, and somewhat) in terms of spiritual well-being.
In this manner, the mean percentages of the items composing each scale demonstrate high value in 42.7% for Life Perspective, Purpose and Goals, 43% for Lessened Meaning, 58.8% for Harmony and Peace, and 42.5% for Benefits of Spirituality.
A punctual inspection of specific questions provides certain information of interest. For example, the situation of a nephrological condition that requires sessions of haemodialysis does not strengthen spiritual beliefs in 43% of patients, whereas only 29.8% declared that their disease had provided quite a lot (18.1%) or very much (11.7%) reinforcement to their faith or spiritual beliefs.
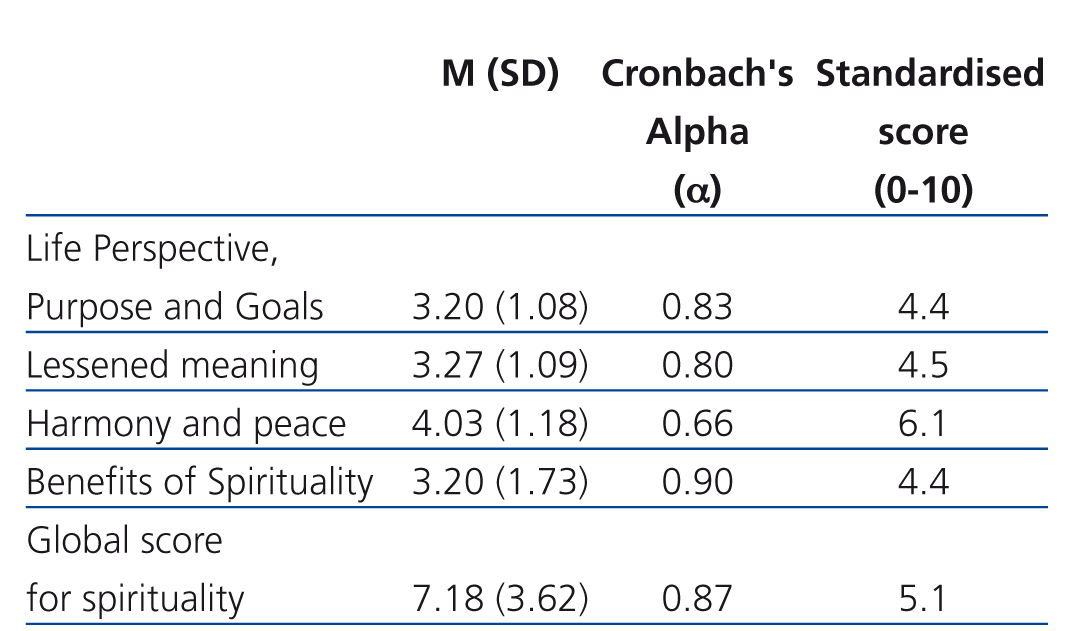
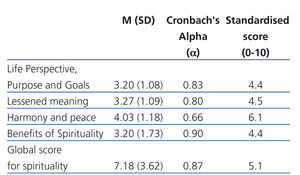
Table 2 summarises the re-scaled and transformed data, as per the original validation study, in the form of averages and standard deviations for each of the scales and the total questionnaire, the Cronbach’s alpha coefficients for this sample of patients on haemodialysis, and the standardisation of the direct scores from each scale and the overall questionnaire into a scale of 0-10.
The internal consistency of the spirituality questionnaire was quite good, as was the case for three of the four scales. Only one of the scales produced a lower, though still quite satisfactory, coefficient value, this being the Harmony and Peace scale. If question 15 were eliminated (the only item in the entire instrument that was inverted for inclusion in the final score), the Cronbach’s alpha for the Harmony and Peace scale would increase from 0.66 to 0.79.
The standardised scores allow for an easy and simple interpretation of the resulting mean values. In this sense, on a scale of 0 (the worst possible score for spiritual well-being) to 10 (the best possible score for spiritual well-being), the sample of patients on haemodialysis obtained low scores (below 5) for three different components: Life Perspective, Purpose and Goals, Lessened Meaning, and Benefits of Spirituality, and higher scores for Harmony and Peace. The normalised mean score for the spirituality questionnaire was 5.1.
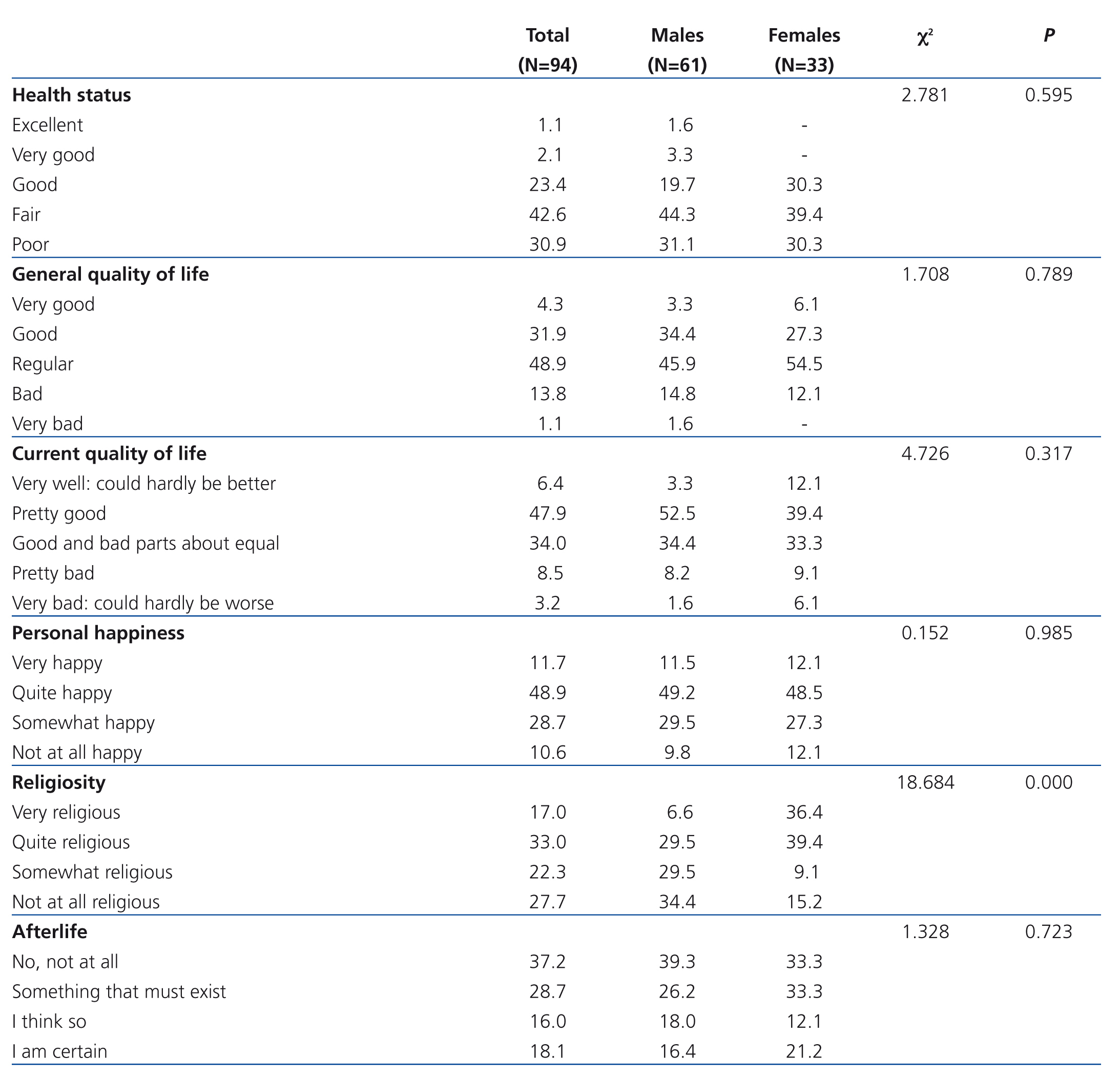
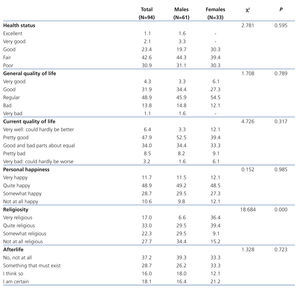
Table 3 shows the distribution both global and by sex of the variables related to subjective well-being (health status, quality of life, and personal happiness) and religious well-being (level of religiosity and belief in an afterlife).
There were no statistically significant differences attributed to gender in terms of perception of health status, general quality of life, current quality of life, level of personal happiness, or belief in an afterlife. On the other hand, there was a significant and substantial difference in terms of level of religiosity: women tended to be more religious than men (P=.000).
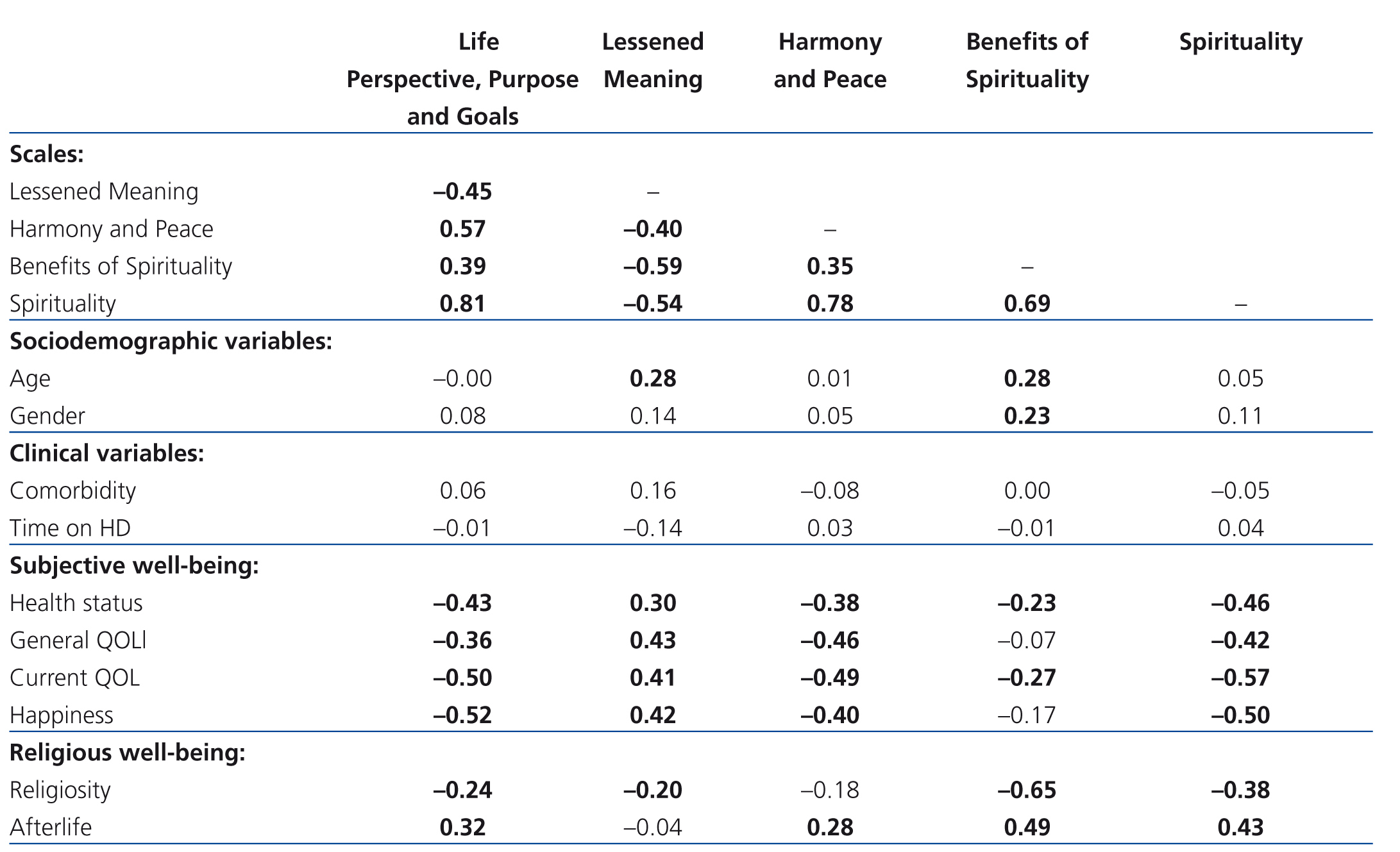
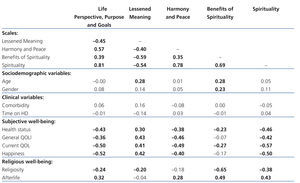
The relational behaviour of scales with each other as well as with sociodemographic, clinical, health status, subjective well-being, and religious well-being variables, are presented in Table 4.
The mean correlation value between scales is 0.45 (P<.001). The scale that explains the highest percentage of variation in level of spirituality is Life Perspective, Purpose and Goals (r=0.81; P<.001).
As regards the two sociodemographic variables, the relational analysis demonstrated that age was significantly correlated with the Lessened Meaning scale (r=0.28; P<.01) and the Benefits of Spirituality scale (r=0.28; P<.01): in older patients, there was a higher probability of issues arising in terms of life meaning and a higher benefit was reported for spirituality. There was only one significant association observed with sex: women reported a significantly higher value in the Benefits of Spirituality score (r=0.23; P<.05).
The level of spirituality, along with each of its scales, was not significantly related to time on haemodialysis (r=0.04) or comorbidity index (r=-0.05).
The total score for spirituality was significantly correlated with each of the self-evaluated variables of self-referred subjective well-being: at a greater level of spirituality, the perceived health status was higher, a greater quality of life was reported, both in general and currently, and the patient reported a greater level of happiness. The same pattern was observed for each of the four scales, with the exception of general quality of life and personal happiness, which did not correlate with overall responses to the Benefits of Spirituality scale.
Finally, spirituality was positively and significantly associated with religious well-being: at greater levels of spirituality, the patient was more religious and gave more credence to an afterlife. This type of association was primarily derived from the Benefits of Spirituality scale. All other relationships between religious well-being and the scores for the other scales barely surpassed a correlation of 0.30.
DISCUSSION
For the first time, the results from our study provide a quantitative measure of the level of spiritual well-being in Spanish patients on haemodialysis. Preliminary results from our study were recently presented by our group.22-27 Along this line, we now have access to a clinical tool for evaluating the level of spiritual well-being in patients on haemodialysis. The viability of the instrument was good. The application of the questionnaire does not imply an inappropriate level of physical or emotional effort on the part of the patient, nor do the needs for administering the questionnaire (time, reading and comprehension abilities, or special needs) imply a burden or excessive effort by either the interviewer or interviewee. Although not rigorously measured, the acceptability of the questions on the part of the patient was quite good. This along with the fact that more than 75% of the patients were able to complete the questionnaire without any help at all is indicative of the high practical applicability and viability of the instrument. Only question 15 of the questionnaire, the only one that is formulated in a negative context requiring inversion of the responses, appears to have generated difficulties in comprehension. The global internal consistency of the questionnaire is quite good, both for the total score (Cronbach’s alpha: 0.87) and for each of the constituent scales, which coincides with the results from the original validation.13
The relational behaviour of each of the different scales and the overall sum of the variables of interest confirm the convergent and discriminatory validity of the questionnaire: spirituality is positively and significantly associated with variables of perceived health, personal happiness, quality of life, and religiosity, independent of gender, negative objective health value (comorbidity), age, and time on haemodialysis. These results coincide with those from other studies involving samples of patients on haemodialysis and other chronic clinical situations.5,28 For example, Finkelstein et al. (2007)1 summarised the evidence from several studies carried out by their research group, concluding that spirituality (evaluated with the Spiritual Well Being Questionnaire) was independent of clinical variables such as comorbidity (Charlson comorbidity index) and patient compliance (evaluated by several health professionals), whereas significant and substantial relationships were found with several indicators of global quality of life, depressive psychological issues (Beck Depression Inventory), and the SF-36 mental component. In addition, the impacts of the disease in patients on haemodialysis are more evident in the physical component of quality of life on the SF-36 scale than on the mental component.29 Other authors observed similar results, in the form of significant and substantial scores, between spirituality and quality of life, satisfaction with life, and symptoms of depression.1,8 High scores for spirituality are correlated with reduced psychological suffering and improved personal well-being.30
The subjective perception of patient health (scored on a scale of Excellent to Bad), or self-evaluated health, is another widely used indicator in the medical literature for monitoring one’s own health, and is correlated with various dependent variables, such as morbidity and mortality.31 Despite the fact that several authors propose self-evaluated mental health as a similar indicator (for example, using the question “in general, would you say that your mental health is excellent, very good, good, normal, or bad”), the available scientific evidence indicates that the first indicator of self-reported health covers both physical and mental health already.31 Little more than 25% of the patients interviewed in this study reported a good health status, which appears to have had a notable impact on spiritual well-being.
Several different studies have demonstrated that spirituality is a fundamental need for medical patients,2,3 with notable repercussions on health care and impacts on clinical decisions to make32 as well as the results from health care upon patient quality of life, family well-being,33 and even on the health care personnel themselves.34-36 Many severely ill patients declare that their interest in existential questions rose substantially with the progression of their disease,35 and even that it is the very adverse or difficult situations that provide the opportunity to grow spiritualy.37 However, our results do not support this last statement. Patients on haemodialysis do not perceive a notable personal growth derived from their health problems. Finding a meaning in life and maintaining faith or hope does attenuate the adverse effects of stress on the mental health of those caring for the patient33 and provides strength for those fighting against a loss of hope. In spite of the possibility that certain members of the clinical team might be more experienced in the field of spiritual care, all health professionals have the opportunity for exploring spiritual or religious values that shape the response of current patients. However, as Surbone and Baider state,38 each patient has a different threshold of intimacy, and sharing one’s spirituality is a very personal subject for both patients and the health care professionals that attend to them. As such, spirituality and religiosity should not necessarily be imposed into the clinical framework, and so should not be directly addressed in routine medical pracitice.38 Finding a meaning of life and hope during a disease is a spiritual task. The search for a meaning of life may not be such a basic need as survival, but it continues to be a very powerful driver of human consciousness,37,39 and the dedication to a constant and unceasing spiritual development can become the very soul of our existence. Providing a meaning of life implies a sense of order, of purpose, and of coherence for our existence; the feeling that we have a reason for being, and that we must fight in order to reach the end goal. If we have purpose, the comprehension of its significance aids in achieving that purpose. If we have no purpose or are unable to achieve it, this significance becomes less important. Thus, each individual must discover their own purpose in life. A strong sense of purpose and meaning of life provides a better subjective sense of well-being.
Religious well-being shares a good deal of the variance observed in spirituality. Spirituality, however, is a much broader concept than religiosity. In a recent consensus conference on spiritual care, the following proposal was presented for a standardised definition of spirituality: “spirituality is the aspect of the human condition that refers to the manner in which individuals search for and express meaning and purpose, as well as the manner in which they express a sense of connection with the moment, one’s self, with others, with nature, and with the holy or divine” (Puchalski et al.4: page 23). Religion, of any type or belief, is one of the possible pathways through which spirituality can manifest itself, but is not the only or most important type.
Almost 30% of our patients declared that they were not at all religious, and little more than 37% believed in an afterlife, but our results also indicate that the total score for spiritual well-being is positively and significantly related to religiosity: patients who declared themselves to be more religious perceive a greater sense of global spiritual well-being, along with greater benefits associated with spirituality in terms of overcoming health issues, a greater purpose in life, and decreased lessened meaning. In addition, a better spiritual well-being is correlated with stronger beliefs in and hope for an afterlife, which creates a greater sense of inner peace, purpose, and benefits of spirituality. The study by Spinale et al.9 found that a greater sense of spirituality (evaluated as the importance of faith) was associated with improved survival in patients on haemodialysis at a medical centre. This relationship between spirituality and survival in patients on haemodialysis could be partially explained by an increased perception of social support in patients that are involved in religious activities.9 In addition, this study showed yet again that females were more apt to declare a greater level of religiosity than males. At least in the healthy population, several researchers have found that females obtain higher scores in measures of spirituality than males.40,41 Purnell and Andersen41 found, as we did, that spirituality and religion are two constructs that are related, but fundamentally distinct.
In comparison with the original validation sample (mainly females with breast cancer and a lower age range than in our study), the level of spiritual well-being in patients on haemodialysis was significantly lower (7.18±3.62 vs 10.80±3.66).13 This difference can be explained, at least in part, by the different type of patient from that study (in regards to diagnosis, demographic variables, and place of origin). Perhaps the environment in the United States is also more receptive and open than ours in terms of the religious and spiritual aspects of disease.42 The mean standardised value of spirituality in our sample was only 5. This was due to the low values in Benefits of Spirituality (4.4) and Life Perspective, Purpose and Goal (4.4), although also in Lessened meaning (4.5). A somewhat higher score was obtained by the scale for Harmony and Peace (6.1). Although it does not appear that these patients responded to the questionnaire with bias in terms of social desirability, some authors have observed a modest but significant correlation between these two variables.41,43
The differences we have observed may also be due to other factors. In fact, the progression or course of a disease in patients with chronic kidney disease is not necessarily similar to cancer patients. There are particular situations experienced by renal patients with advanced disease (for example, removal from the dialysis machine) that are singular in these patients. In the context of end of life situations, which includes suffering from a renal disease that advances progressively and requires renal replacement therapy in order for the patient to survive, it can be clinically useful to identify these differences in order to optimise the clinical care given to these patients.44 Chronic kidney disease patients appear to have a particularly low level of awareness of the options for palliative care and of the progression of their disease. Less than 10% of these patients report having had a conversation regarding end of life issues with their nephrologist in the last year.44 The majority of nephrologists do not feel properly prepared or trained to make end of life care decisions for their patients, professing that these measures effectively obliterate any hope the patient still had. Attention to spiritual issues appears as an essential area for providing quality care to renal patients, and studies demonstrate a strong desire on the part of the patient to incorporate spirituality into their care.44,45
These last studies involved analyses of two different types of spirituality (religious and existential) in North American patients, finding through self-evaluations that religious spirituality was weakly correlated with existential spirituality, which coincides with our results. These studies also found that, whereas the religious dimension of spirituality does not particularly capture the existential dimension, it is the existential component that is clinically more relevant in nephrological patients and that has a greater impact on quality of life,45 results that coincide with our own. However, in a sample of 205 patients on dialysis in Brazil, Lucchetti et al.46 found that religiosity was associated with a lower frequency and severity of depression and with a higher perceived quality of life.
The subjective experience of disease often prompts the incorporation of health issues into the context of his/her personal life, thus favouring a perception of coherence and competence for taking action against possible changes. In other cases, the patient experiences a multi-dimensional suffering, the “total pain” coined by Cicely Saunders at the inception of the Hospice movement, expressing unsatisfied spiritual needs in the form of indeterminate emotional distress, leading to spiritual distress. Recently, Chaves et al.47 identified and clinically validated a series of definitive characteristics proposed for diagnosing spiritual distress, referred to as “impaired spirituality.” According to this study, 27.5% of chronic kidney patients receiving haemodialysis that were interviewed were diagnosed with impaired spirituality, in which suffering was questioned, alienation was reported, patients were incapable of expressing creativity, and anger was shown as a behavioural alteration. According to the authors, this percentage implies an important conflict in the spiritual dimension of these patients, which could hinder a positive outlook when dealing with kidney disease.
Despite the fact that patients desire that their attending physicians take the initiative in approaching and dealing with end of life decisions and spiritual needs,38,44 these issues appear to be poorly addressed, and the level of training and awareness in health professionals is insufficient and unsatisfactory. A substantial portion of health professionals are incapable not only of detecting a patient’s spiritual needs, but also of considering their own spiritual needs as health care providers.48 Despite the fact that spiritual well-being is a crucial aspect in the adaptation of many patients with terminal chronic disease,48 studies have demonstrated a high level of difficulty expressed by health care professionals, specifically those who work in palliative care, in identifying the expressions of spiritual needs from their patients and defining what exactly is spirituality. This lack of a capacity for recognising the importance of spirituality translates into a barrier against being able to respond to such a need. Between 40% and 48% of palliative care professionals do not identify the spiritual needs of their patients or speak with them about death or the subject of spirituality in clinical sessions. At least in our country, spirituality still has sparked very little interest or attention in the majority of health care professionals, including those who work in palliative medicine.48
A human is a biological, psychological, social, and transcendent being. Disease, which is both a biomedical reality and a socio-cultural construct, affects and can create discord in any or all of these dimensions, and only a biopsychosocial and spiritual model provides the appropriate basis for complete and holistic health care for the patient.49 Spiritual well-being is not something that simply creates itself: it is a human condition that we must prepare for, cultivate, manage, and defend. We are all immersed in spiritual dimensions of existence: recognising these spheres of thought and feeling aids in creating the appropriate atmosphere for personal development.38,49,50 In fact, many patients with severe chronic diseases seek guidance from health care professionals for their spiritual concerns: what is the meaning of this suffering? have I done something bad to deserve this? is there an afterlife? who will take care of my loved ones? has my life really been worth it?, etc. Health care professionals are not necessarily capable of composing a valid response to the spiritual questions of each patient, but they can accompany them in this line of questioning by providing physical company and support, facilitating dialogue, offering a comfortable atmosphere in which to explore these questions, showing compassion, sharing uncertainties and hopes, sharing with the patient the journey for spiritual awareness and understanding, and even seeking assistance from other fields when necessary (psychological, social, religious, etc.).38,48 In any case, spirituality can be shared, but never imposed. Doctors must never use their power and authority to proselytise, but this does not mean that we should ignore the concerns or questions of the patient. Even more so, health care professionals should place special attention on their own spiritual lives, since their state of spirituality will undoubtedly affect the manner in which they attend to their patients. In certain cases, patients may not want to discuss or even consider spiritual questions, and these wishes, too, should be respected. Therefore, spirituality and religiosity should not be imposed in clinical practice.38
One important limitation of this study was the restrictions involved in using a questionnaire. In this sense, the responses to our instrument are difficult to interpret, since patient comprehension of the questions and the reasons for responding in one way or another were not directly assessed. The lack of a definitive pattern impacts our ability to evaluate spirituality in clinical and research contexts. The definition of spirituality used in this study is based on an empirical review of the relevant medical literature, but does not reflect an internationally standardised definition of spirituality. In addition, we would need to consider both philosophical and theological sources of literature as well in order to conceive of a more complete concept of spirituality. Another limitation of our study was the application of the instrument in a sample of convenience, which does not guarantee the ability of extrapolating our results to the general population. Future studies with other samples of chronically ill or palliative patients could greatly aid in developing a better perception of spiritual well-being in patients on haemodialysis as compared to other groups of interest.
CONCLUSIONS
The role of health care professionals in the spiritual care of their patients is becoming an ever more relevant aspect of medicine that requires an increased scientific rigour in the research into spirituality in clinical practice.
The adaptation of the MiLS into Spanish (MiLS-Sp) has shown to be a viable, reliable, and valid instrument for evaluating spiritual well-being of patients on haemodialysis. The scores for spiritual well-being in our sample of patients were relatively lower than the values we expected or hoped to see. This questionnaire may be useful for learning the level of spiritual well-being and spiritual needs of these patients in a clinical context, and for comparing them with other patient groups (palliative care, primary care, etc.).
Finally, as a recommendation for the future, it would be very interesting and relevant to analyse the relationship between spiritual well-being and survival in patients with chronic kidney disease.
Conflicts of interest
The authors have no conflicts of interest to declare.
Table 1. Abbreviated results for spiritual well-being questions in each scale
Table 2. Descriptive analysis of the spiritual well-being questionnaire results
Table 3. Bivariate analysis (by sex) of subjective well-being and religious well-being variables
Table 4. Relative analysis of the study variables