The analysis of body composition in chronic kidney disease patients has garnered interest in recent years due to the major impact it has as a risk factor for morbidity and mortality.1,2 Amongst the various methodologies used to evaluate body composition, bioelectrical impedance analysis (BIA) stands out because of its simplicity, low costs, speed, reproducibility, and safety for the patient being examined. The use of BIA in the evaluation of body composition has been expanding in the last few decades, and throughout this period the tools available for this analysis have improved significantly.
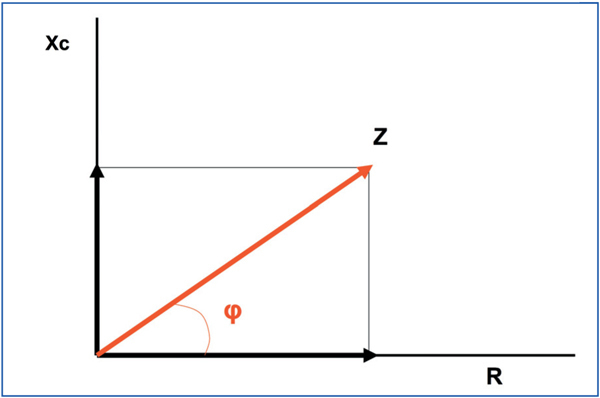
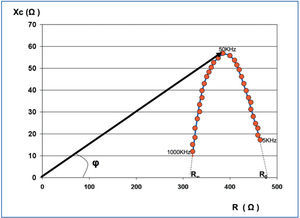
From an electrical point of view, an organism acts as a conductive cylinder or sum of cylinders. BIA is based on the opposition that any organism creates against the flow of an alternating electrical current, which is normally emitted and received from the opposite ends of the cylinders; in the case of a human, from the wrist and ankle. Impedance (Z) is the result of two different components (Figure 1): resistance (R) to the flow of electrical current, which is primarily given by the water content in the body (water being an excellent conductor), such that greater water content yields a lower R, and vice versa. This allows us to analyse the hydration state of a patient, and to distinguish between tissues with large water content, such as muscle, from those with low water content, such as fat, lungs, and bones. The second component is reactance (Xc), which determines the capacity of cells to store energy, since they act as electrical condensers when an electrical current is passed through them. Cell membranes act as conductors and the cellular contents act as dialectic material, storing the charge once the current is passed through the medium. These two components are expressed in Ohms (Ω), and they are graphically represented by vectors, with the resulting vector impedance (Z). The angle formed by R and Xc is called the phase angle (φ), which is normally less than 10º, since R is far greater than Xc. In summary, whereas R primarily determines hydration state, Xc primarily determines nutritional state.
TYPES OF BIOELECTRICAL IMPEDANCE
Based on the frequency of the alternating current applied, BIA can be classified as monofrequency or multifrequency BIA.
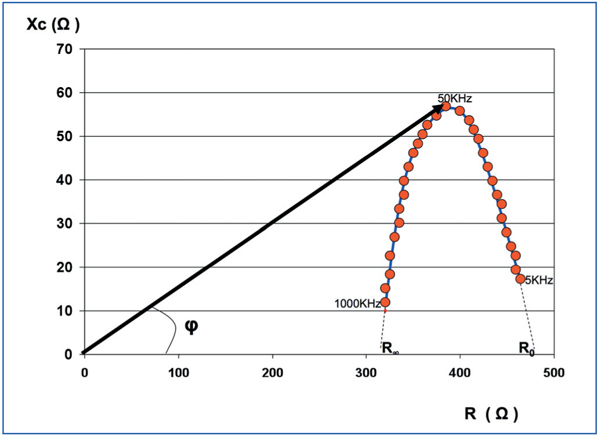
Multifrequency BIA consists of the measurement of resistance, reactance, and phase angle, with frequencies oscillating between 5kHz and 1000kHz. A graphical representation of these measurements results in a parabola, corresponding to the Cole and Cole model (Figure 2).3 With low frequencies, the electrical current is incapable of passing through the cell membranes, and instead moves through the extracellular space, encountering resistance only in the extracellular water and the ions it contains (ECW). The values of Z for this type of frequency lie to the right of the Cole and Cole model, and if the curve is extrapolated until meeting the X-axis, that is to say, with an Xc of 0, we would obtain the resistance corresponding to the ECW (R0).
High frequencies are capable of crossing both cells and extracellular space. As such, the resistance is determined by the opposition given by intracellular water and the ions it contains (ICW), as well as ECW. The values of Z for high frequencies lie to the left of the Cole and Cole curve, and an extrapolation to the X-axis yields an R-value (R∞) estimate, corresponding to total body water, where TBW=ICW+ECW.
Once R0 and R∞ are known, the calculation of resistance corresponding to ICW (RI) is given by the difference in resistance, following the equation below:
1 1 1 R0R∞
--- = --- - --- where RI = ----------
RI R∞ R0 R0 - R∞
Monofrequency BIA is based on the measurements of R, Xc, and phase angle only at 50kHz, since at this wavelength, phase angle and reactance are considered to be at a maximum, that is to say, they would be at the highest part of the parabola (Figure 2). However, when all of the measurements are obtained, using multifrequency analysers, it is observed that this axiom is not constant, and as such, monofrequency BIA assumes a certain level of error, especially with extreme values of body composition.
Phase angle gives us an indirect idea of cellular mass, and as such, it has been considered as a good parameter for nutrition that has been widely used as a marker for survival.4-7
Currently, we have at our disposal three different systems for analysing BIA: based on formulas, vector impedance, and impedance spectroscopy (BIS). The first two are based on monofrequency models, whereas BIS is based on a multifrequency model.
Systems based on formulas have worked for many years, and several different equations have been described,8-10 in which the subject’s height tends to be included along with mean resistance at 50kHz. The equations were validated with reference methods for certain subgroups of the population, and so it is recommended that each researcher put together reference tables specifically for each study using healthy subjects.11 Normally, the software included in BIA analysers allows for calculating TBW, ICW, and ECW, as well as lean mass or fat-free mass, and fat mass calculated using the difference between body weight and lean mass. It is important to point out that the different equations described in the literature are only valid for those impedance analysers for which they were developed. In hyper-hydrated patients, the excess water is incorporated into the lean mass instead of displaying this as a third body component.
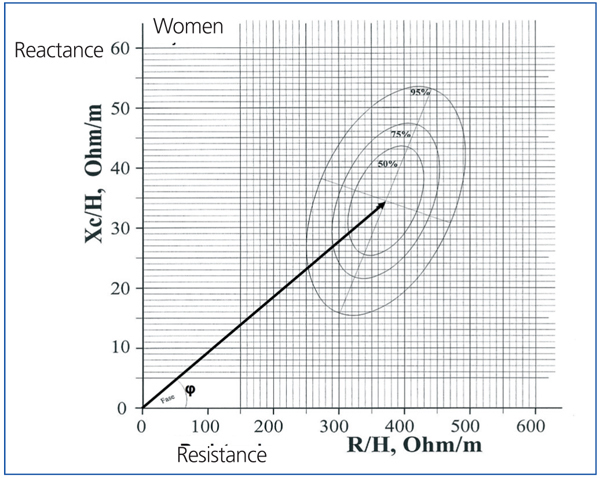
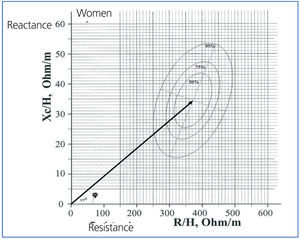
The bioelectrical impedance vector analysis (BIVA) system was introduced by Piccoli in 1994.12 This is based on the length of the impedance vector and its phase angle measured at 50kHz. The length of the vector establishes the level of hydration, such that the longer the vector, the lower the water quantity and greater the resistance, whereas the greater the phase angle is, the better the nutritional state. The reference values are provided by ellipses that represent 50%, 75%, and 95% percentiles in the form of a nomogram (Figure 3), but as in formula-based models, the reference ellipses were calculated in a population of healthy Italian subjects. This model offers an idea of the evolution of hydration state in a patient as he/she gets closer or farther from the ellipse centre,12,13 but it also impedes making quantitative comparisons between patients or groups of patients. The ellipses are different for men and women due to differences in body composition (fat content), but in order to achieve a greater level of accuracy, they should also be divided according to age, nutritional rate, and even race.11,14 Additionally, reference ellipses should be developed that incorporate several of these variables, which would excessively complicate the elaboration of reference patterns.
Recently, Fresenius Medical Care developed a BIS analyser (BCM®; Body Composition Monitor) based on simultaneous measurements of R, Xc, and phase angle at 50 different frequencies, which oscillate between 5kHz and 1000kHz, using the Cole and Cole model for determining ECW, ICW, and TBW. The system is different to other multifrequency BIA models as it is based on tissue normohydration, assuming a certain value for the physiological content of water contained in lean mass and adipose tissue, the latter being much lower. The excess water is described by the difference between TBW and the water contained in normohydrated adipose and lean tissues.
The model considers fat content, which maintains an inverse relationship with TBW, ICW, and ECW, according to a study by Chamney et al,15 such that, for example, in a subject with a fat content of 10%, as measured by DEXA , the TBW adjusted for normohydrated tissues is approximately 65% of the total body weight (40% ICW and 25% ECW), whereas in another subject with a 30% fat content, TBW would be 50% (30% ICW and 20% ECW). As such, after adjusting for the fat content in each subject analysed, no other reference pattern is needed in addition to the person’s own body composition.15
APPLICATIONS IN PATIENTS WITH CHRONIC KIDNEY DISEASE
Hydration
It is essential to quantify the hydration state in the clinical evaluation of patients with chronic kidney disease both before and after starting renal replacement therapy.16-21 The incorporation of dry weight as measured by BIS in patients on haemodialysis allows for showing that the clinical evaluation of the patient is skewed from the true situation in some cases, whereas in other cases facilitates the improvement of haemodynamic tolerance.22,23 This will influence both blood pressure and the severity of left ventricular hypertrophy.24,25 Maintaining a hydration state close to ideal levels can aid in controlling residual renal function in dialysis patients, the loss of which is another risk factor for mortality.26 More recently, ECW has also been associated with inflammatory states.27,28
Nutrition
Nutritional state is a factor that has a major impact on mortality in chronic kidney disease patients.29-31 Measuring body composition and its changes in time by BIA provides morbidity/mortality markers that can aid in the early detection of reversible changes in these patients.32,33 Additionally, this tool allows for distinguishing between lean mass and fat mass, which have different impacts on patient evolution and provide added value to the classic method for determining body mass index.34,35
Volume of distribution of urea (UDV)
The introduction of haemodialysis monitors that determine the dialysis dosage using online ionic dialysance is becoming more and more frequent. This type of device aids in analysing the dialysis doses being administered.36-38 The measurement of UDV is usually performed by the monitor itself, using anthropometric formulae, among which the Watson equation39 is the most commonly employed. In patients with extreme fat content, the differences between UDV provided by BIS and using equations can be significant. As such, using the UDV measured by BIS can provide a dialysis dose better adjusted to the patient’s true situation.
In summary, BIA is a non-invasive, simple tool that requires little time, with reproducible and low-cost results that, given the information that they provide to the nephrologist and all of its clinical applications, should form a part of the health care equipment at the disposal of all departments, especially in dialysis units.
The two studies included in this issue of Nefrología and the previous one show some of the many applications of BIA.6,7 Caravaca et al described their results with BIS in patients with predialysis advanced chronic kidney disease, demonstrating slight over-hydration, with a mean of approximately 0.2 litres. However, there was a wide range of variation. Hydration is more important in men and diabetic patients, and is inversely correlated with body mass index and plasma albumin and haemoglobin levels. The quantitative assessment of excess hydration or dehydration, regardless of body composition, is a parameter of great clinical importance, and can only be provided in a precise manner using the most advanced BIS systems available.
The study by Abad et al examined phase angle as a nutritional marker in dialysis patients. For this, they used a multi-frequency BIA analyser, although in the analysis of the results the authors only took into account the results obtained using only a frequency at 50kHz, which is the commonly used value in monofrequency. The authors concluded that phase angle was associated with nutritional parameters and the content of ICW, similar to the results from Caravaca et al. However, the most novel result was the association between phase angle and dialysis patient survival. This association was strongly supported by a multivariate analysis that was adjusted for other nutrition and inflammation variables, in which only age and a phase angle <8º continued to be independent risk factors for mortality. Although the phase angle has previously been described as a short-term protective factor,4-7 this study supported its prognostic value after 6 years of follow-up.
Both studies concur that the best prognostic value of phase angle is reached at 50kHz, but the cut-off point is different in the two studies, probably as a result of the different analysers used in the two studies. It is important to point out that generally, when we talk about BIA, the equations and raw data obtained with one analyser are not valid for another type of analyser.
KEY CONCEPTS
1. Bioelectrical impedance analysis is an extremely useful tool in the treatment of chronic kidney disease patients. It should be incorporated into all units because of the information provided, ease of use, quick results, safety, and low cost.
2. The primary applications of this technology are the evaluation of hydration state, the analysis of nutritional state, and the calculation of the volume of distribution of urea for a better application of this kinetic model.
3. It is preferable to use raw data that are provided by the bioelectrical impedance analysers themselves in order to avoid errors induced by different values for body composition, which would eliminate the need to search for adequate reference values for the population that we wish to study.
4. Bioelectrical impedance systems have notably improved in recent decades, and are always providing more precise information. Bioelectrical impedance spectroscopy is the most advanced method currently available, since the results from this technique are adapted to tissue normohydration and are adjusted for the fat content in the patient’s body composition, without the need for a reference population adjusted for age, sex, race, or body composition.
5. The hydration and nutrition parameters provided by the bioelectrical impedance analysers are extremely useful as early markers of survival/mortality in patients with chronic kidney disease with/without dialysis.
Figure 1. Vector components of electrical impedance (Z). Xc = reactance; R: resistance; g: phase angleVector components of electrical impedance (Z). Xc = reactance; R: resistance; g: phase angle
Figure 2. Representation of the vector bioelectrical impedance model
Figure 3. Graphical representation of multifrequency impedance, where each point corresponds to a different frequency (Cole and Cole method)