Leprosy is a chronic disease caused by the intracellular bacillus Mycobacterium leprae, which primarily affects the skin and peripheral nerves.1 The clinical picture is variable; there are paucibacillary forms with few lesions (tuberculoid leprosy), and multibacillary forms with numerous lesions (lepromatous leprosy), which occurs in patients with impaired cellular immunity.2 The presence of extracapillary glomerulonephritis with leprosy is rare, and here we describe the case of a patient with both diseases.
This was a 79-year-old man diagnosed of leprosy at age 32, with both neurological and cutaneous involvement. He was admitted in March 2011 with oedema, haematuria, and worsening of renal function. On examination, he was noted to have leonine facies, loss of eyebrows, and a saddle nose. His skin was rough with xerostomia and thickening, and there were erythematous macules on the limbs. BP was 168/104. Venous pressure was elevated, and there were bibasal crepitations and peripheral oedema. There was reduced sensibility to touching and pain in the limbs.
Blood test revealed a haemoglobin of 11.9g/dL, leukocytes 6660/mm3, platelets 173,000/mm3, creatinine 2.31mg/dL, and urea 93mg/dL. Transaminases, LDH, CK, cholesterol, triglycerides, HDL, and LDL, were normal. Urinary sediment had >100 red blood cells per field (90% dysmorphic), with a 24h proteinuria of 1.3g. Serology was negative for HIV, hepatitis B and C virus. ANA, ANCA, and anti-glomerular basement membrane antibodies were negative, and C3 and C4 were normal. Chest X-ray showed vascular redistribution and a left-sided pleural effusion. Abdominal ultrasound showed kidneys of normal size with increased cortical echogenicity with no other abnormalities.
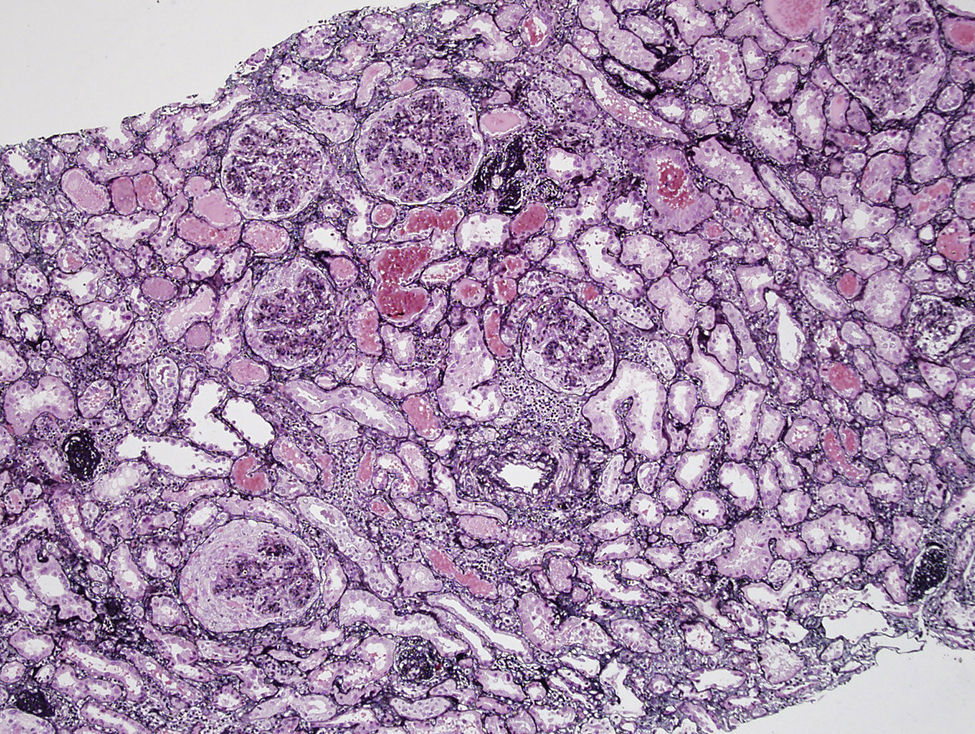
Percutaneous renal biopsy was performed and showed a proliferative endocapillary and extracapillary glomerulonephritis affecting most glomeruli (Fig. 1). Immunofluorescence was negative, there were no amyloid deposits, and no acid-alcohol fast bacilli using Fite technique. Treatment was started with 3 boluses of 6-methyl-prednisolone and thereafter oral prednisone (60mg daily) and cyclophosphamide (100mg daily). Renal function progressively deteriorated, and treatment with haemodialysis was started via a tunnelled right jugular catheter.
In May 2011, pancytopenia was observed, so cyclophosphamide was stopped and treatment with sodium mycophenolate was started (360mg every 12h). In June 2011, he was readmitted with bilobar pneumonia, so sodium mycophenolate treatment was stopped definitively, and prednisone continued, at a reducing dose.
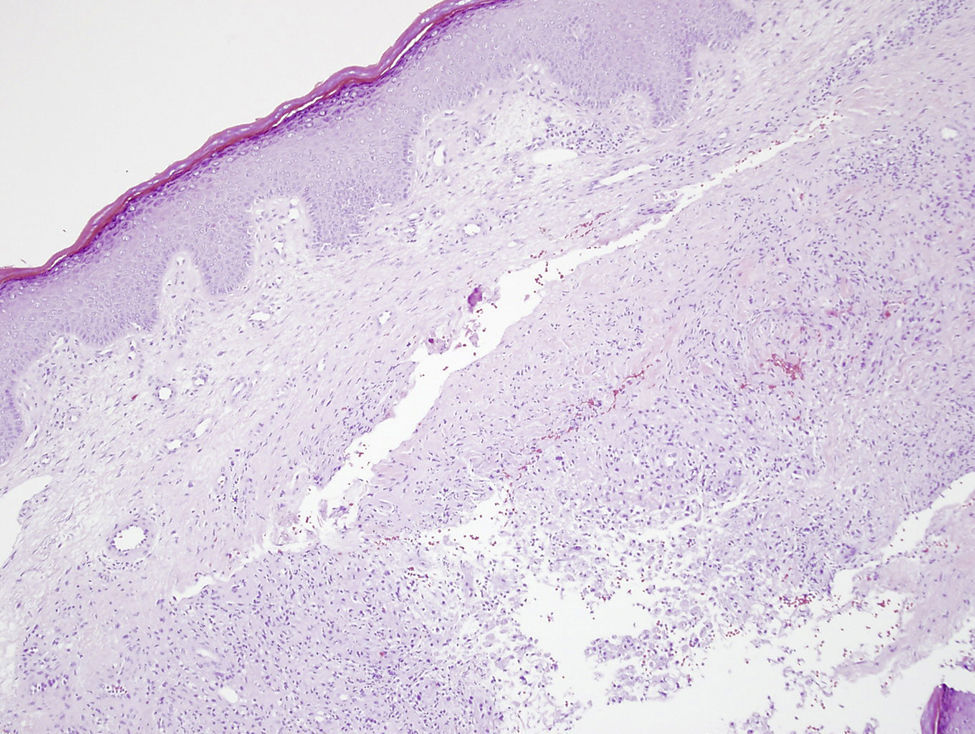
In August 2011, due to the appearance of cutaneous lesions in the lower limbs, biopsy was performed, which showed areas of dermal necrosis associated with macrophages with focal images of leukocytoclastic vasculitis of small vessels, compatible with a diagnosis of type II lepra reaction (borderline lepromatous) (Fig. 2). Treatment was started with dapsone (100mg daily), clofazimine (50mg daily), and rifampicin (300mg per month). He was readmitted in October 2011 for severe anaemia with a haemoglobin of 5.7g/dL, and diagnosed with haemolytic anaemia secondary to dapsone, which was stopped. The patient continued on haemodialysis treatment, and died following a haemopericardium in relation to the change of jugular catheter in July 2012. Post-mortem examination was not possible.
Conclusions: leprosy, particularly in the lepromatous form, can cause secondary renal amyloidosis, especially in patients who have recurrent episodes of associated erythema nodosum or chronic skin ulcers; tubulointerstitial nephropathies, both acute and chronic can also occur.3–5 Finally, several types of immune complex glomerulonephritis have been described, such as proliferative endocapillary, proliferative mesangial, membranoproliferative, and focal glomerulosclerosis.3–5
Extracapillary forms have been described in exceptional cases.6–10 Typically, patients present with acute renal failure. In some cases, the presence of bacilli has been demonstrated in the renal parenchyma at a glomerular level and in the interstitium.7 The mechanisms connecting extracapillary glomerulonephritis with negative immunofluorescence and leprosy are not well-known, but it is possible that the immune abnormalities produced in leprosy could favour the generation of glomerulonephritis.
In these patients, the appropriate treatment must be considered. In our case, treatment was started with cyclophosphamide, and subsequently, mycophenolate sodium with steroids. It is highly possible that this treatment contributed was key in the reactivation of leprosy as was confirmed on cutaneous biopsy, therefore prophylactic treatment with dapsone or clofazimine should be considered in such cases.
Leprosy treatment in patients on dialysis is difficult because there is little experience with the drugs used, and the dose must be adjusted. The risk of side effects increases, and in fact, our patient had severe haemolytic anaemia, possibly secondary to dapsone treatment.
Please cite this article as: de Arriba G, Fiallosa RA, de Lorenzoa A, Rodríguez-Palomaresa JR, Pernab C. Glomerulonefritis extracapilar y lepra: una asociación infrecuente. Nefrologia. 2016;36:313–314.