Frailty has been defined as a syndrome or state of deterioration and increased vulnerability to situations of stress which occurs with ageing. It is characterised by weakness and diminishing of functional biological reserves, which leads to an increased risk of further deterioration towards disability, hospitalisation and death.1,2 Frailty is not the same as disability and comorbidity; although the three concepts are closely related and affect each other, they do not always coexist.3
Although frailty has been defined as generally associated with advanced age and ageing, there are conditions and diseases that cause changes similar to ageing which can lead to a state of frailty at younger ages, and one of these situations is chronic kidney disease.4–6 The prevalence of frailty in patients on haemodialysis has been estimated by different studies at 26–73%.7,8 The huge variability can be explained by differences in the populations studied and the different tools used to assess frailty.9,10 In Spain, no studies have been published to date on the prevalence of frailty in patients on haemodialysis.
Our aim was to estimate the prevalence of frailty in patients on haemodialysis in the southern health area of Gran Canaria and to study some of the associated demographic, clinical and analytical factors. We designed a cross-sectional study of 277 patients on haemodialysis, estimating frailty using the Fried Frailty Phenotype Index (FFPI) and the Edmonton Frail Scale (EFS). The FFPI is a standardised five-item scale that measures weakness, slow gait speed, exhaustion, low physical activity and weight loss. The EFS contains 11 items that also measure other spheres of frailty, such as cognitive, psychological and social factors. We collected demographic and clinical data, the Charlson comorbidity index and analytical parameters. Patients were then followed up for a year to assess mortality rates according to frailty.
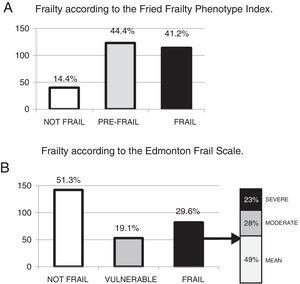
The prevalence of frail patients with the FFPI was 41.2% and, with the EFS, 29.6%. Fig. 1 shows graphs of the prevalences found with both tests. We found a lack of consistency between the scales; of patients frail with EFS, 83% were frail with FFPI and 17% pre-frail, and of patients frail with FFPI, 60% were frail with EFS and 40% vulnerable or non-frail. The EFS classified a larger number of patients as non-frail, while the FFPI classified a larger number as pre-frail. It is difficult in a cross-sectional study to determine the reason and the prognostic implications of this lack of consistency, but it could be a result of the different spheres of frailty measured by each of the tests.
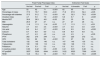
Table 1 shows the main demographic, clinical and analytical characteristics according to the results of the two tests. We can see that there is an association between frailty and other clinical data suggesting poor prognosis, such as advanced age, diabetes mellitus, a higher Charlson comorbidity index and being female. Among the analytical parameters, a slight but statistically significant decrease in haemoglobin, albumin and uric acid was found in the pre-frail and frail groups with respect to the non-frail. We found no differences between groups in the parameters of bone-mineral metabolism or lipid profile. There was a significant decrease in CPK with frailty, which may reflect a decrease in muscle mass due to frailty-associated sarcopenia. We also found an increase in certain analytical parameters described as markers of poor prognosis for their relationship with inflammation or overhydration, such as C-reactive protein, NT-proBNP and red cell distribution width.
Demographic, clinical and analytical characteristics.
| Fried Frailty Phenotype Index | Edmonton Frail Scale | |||||||
|---|---|---|---|---|---|---|---|---|
| Not frail | Pre-frail | Frail | p | Not frail | Vulnerable | Frail | p | |
| Age | 52 | 62 | 71 | <0.001 | 62 | 65 | 71 | <0.001 |
| Percentage of males | 77.5 | 70.7 | 55.3 | <0.01 | 71.8 | 67.9 | 52.4 | <0.05 |
| Percentage with diabetes | 37.5 | 51.2 | 71.1 | <0.001 | 43 | 32.3 | 79.3 | <0.001 |
| Charlson Index | 4.7 | 5.9 | 7.9 | <0.001 | 5.6 | 6.7 | 8 | <0.001 |
| Months RRT | 30.6 | 28.3 | 49.1 | <0.05 | 29 | 33 | 50 | n.s. |
| BMI | 26.5 | 27 | 27 | n.s. | 27 | 27 | 26 | n.s. |
| Haemoglobin | 11.8 | 11.3 | 11.4 | <0.05 | 11.7 | 11.3 | 11.1 | <0.01 |
| Albumin | 3.7 | 3.6 | 3.5 | <0.001 | 3.7 | 3.5 | 3.5 | <0.01 |
| Uric acid | 6.6 | 6.4 | 5.7 | <0.001 | 6.4 | 6.5 | 5.6 | <0.001 |
| Calcium | 8.7 | 8.8 | 8.9 | n.s. | 8.8 | 8.9 | 8.8 | n.s. |
| Phosphorus | 4.7 | 4.3 | 4.2 | n.s. | 4.4 | 4.5 | 4 | <0.05 |
| iPTH | 262 | 275 | 249 | n.s. | 277 | 225 | 272 | n.s. |
| CPK | 104 | 82 | 56 | <0.001 | 91 | 67 | 50 | <0.001 |
| Total cholesterol | 132 | 145 | 140 | n.s. | 147 | 140 | 135 | n.s. |
| Triglycerides | 130 | 139 | 112 | n.s. | 130 | 126 | 113 | n.s. |
| Potassium | 5.4 | 5.3 | 5.3 | n.s. | 5.3 | 5.5 | 5.3 | n.s. |
| C-reactive protein | 0.32 | 0.42 | 0.6 | <0.05 | 0.41 | 0.61 | 0.48 | n.s. |
| NT-proBNP | 2637 | 3230 | 6944 | <0.001 | 3122 | 6523 | 7599 | <0.001 |
| RDW | 14.6 | 15.4 | 16 | <0.001 | 15.1 | 15.6 | 16.3 | <0.005 |
At one-year follow-up, the mortality rate was 21.1% in frail patients versus 11% in pre-frail and non-frail patients with the FFPI (p<0.05). With the EFS, the mortality rate was 26.8% in frail patients compared to 10.3% in vulnerable and non-frail patients (p<0.001).
In conclusion, we found a high prevalence of frailty in patients on haemodialysis. Frailty is associated with poor short-term outcomes. However, we found a lack of consistency between the tests used to measure frailty, and further studies are therefore necessary to validate the frailty tests in patients on haemodialysis, determine their prognostic value and establish the impact of possible therapeutic measures to reverse frailty in this group of patients.
FundingThis study was funded in part by a grant from the Colegio Oficial de Médicos de Las Palmas [Official College of Physicians of Las Palmas] 21st invitation for grant application proposals for research projects and work placements.
Please cite this article as: García-Cantón C, Ródenas Gálvez A, Lopez Aperador C, Rivero Y, Diaz N, Antón G, et al. Prevalencia de fragilidad y factores asociados en pacientes en programa de hemodiálisis. Nefrologia. 2019;39:204–206.