“Hidden” renal disease (HRD) is defined by an UF <60ml/min associated to normal range SCR. In Primary Care several trials have been performed in order to know HRD prevalence; Labrador et al. performed 13,784 SCR measurements in patients over the age of 18. Findings were the following: UF <60ml/min/1.73m2 in 1042 patients, out of which 418 resulted in normal range SCR, all of them female with an average age of 76.5.1 A newly published Nephrology trial was performed on a total of 183 subjects (64.5% female) with an average age of 59.1±18.2 years. 21.4% or 25% of them would have HRD if MDRD-4 or Cockroft-Gault equations respectively were applied.2
Notwithstanding, only a few trials have focused on knowing what was the outcome of those patients diagnosed of HRD over the course of time. In this study, both the clinical and analytical evolutions of patients with HRD were assessed over a period of five years.
According to “Ancianos con Enfermedad Renal Crónica del Hospital General de Segovia” (Elderly people with Chronic Renal Disease at the Segovia General Hospital), which included 80 elderly people recruited between January and April 2006, normal SCR range (≤1.1mg/dl) was found in 38 patients.3 Of those, baseline characteristics and five-year follow up were analyzed in patients diagnosed with HRD.
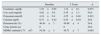
Out of the 80 patients, 18 (22.5%) could be considered as carriers of HRD; all were female and their average age was 81.33±6 years. 33.3% were diabetic and 83.3% were diagnosed of hypertension. For baseline treatments, 66.7% were on diuretics and 38.9% were on ACE inhibitors. During the five-year clinical evolution, 1 of them (5.6%) presented de novo ischaemic cardiopathy and 3 (16.7%) had cardiac failure episodes; 8 (44.4%) patients died during that period. No patient evolved to end-stage nephropathy or needed renal replacement therapy. Baseline and post-five-year analytical data are showed in the table below (Table 1).
Baseline data and five-year evolution data for patients diagnosed with HRD.
| Baseline | 5 Years | A | |
|---|---|---|---|
| Creatinine, mg/dL | 1.03±0.05 | 1.14±0.1 | 0.051 |
| Uric acid (mg/ml) | 4.92±0.9 | 5.45±1.3 | N/A |
| Potassium mmol/L | 4.24±0.4 | 4.55±0.48 | 0.021 |
| Calcium mg/dl | 9.37±0.42 | 9.45±0.44 | N/A |
| Haematocrits (%) | 40.44±3 | 40.88±4 | N/A |
| Urine protein (g) | 0 | 0 | N/A |
| MDRD (ml/min/1.73m2) | 54.50±3 | 48.71±7 | 0.063 |
Our study found that around one-quarter of the analysed population could be considered as HRD carriers, all of were female. Our findings are similar to those of Pérez-Durillo et al. which analysed a younger population, and to those of Labrador et al. where HRD was registered in female patients. Another contribution of our study was the evolution over time of these patients; there was a slow decrease of GFR values, without typical manifestations of renal failure (such as anaemia or hypocalcaemia) or progression of renal failure to end-stage nephropathy. Therefore, the term “hidden” in elderly female patients with HRD might refer to the “physiological” GFR drop associated with age. Our study confirmed a drop of about 1.1ml/min/yr while patients still kept their SCR levels within normal range without typical manifestations of renal failure.
Conclusion: the term HRD should be avoided in elderly people. In those female patients whose SCR range remains normal over time, the drop of UF might correspond to “physiological” renal ageing and not to a “pathological” process.
Please cite this article as: Heras M, Guerrero MT, Sow A, Muñoz A, Ridruejo E, Fernández-Reyes MJ. Enfermedad renal “oculta” en ancianos: ¿continúa “oculta” a los cinco años de seguimiento? Nefrologia. 2015. . 2015;35:343–344.