IgA nephropathy is a prevalent glomerulopathy in the diagnostic work-up of haematuria and is the most common glomerular condition.1,2
This autoimmune disease is characterised by abnormal synthesis and glycosylation of IgA, resulting in an imbalance and an increase in circulating galactose deficient IgA1 (Gd-IgA1).1
The diagnosis is associated with a reduction in life expectancy of 6–10 years.2
Regarding treatment, patients with proteinuria above 500 mg/24 h should be started on ACE inhibitors/angiotensin II receptor blockers (ARBs). Steroids should be administered in patients with nephrotic proteinuria or in the group of patients at risk of progression to chronic kidney disease.3,4
The course of the disease is glomerular in the usual forms of presentation, but there is very little information regarding the clinical course and its prognostic implications when the manifestation is persistent macroscopic haematuria as the only presenting sign of this glomerulopathy.5,6
We present three clinical cases in which the presentation and common denominator is persistent macroscopic haematuria.
Case 1A 38-year-old man, with no personal history of interest, was referred to the nephrology department for persistent macroscopic haematuria of 20 days’ duration.
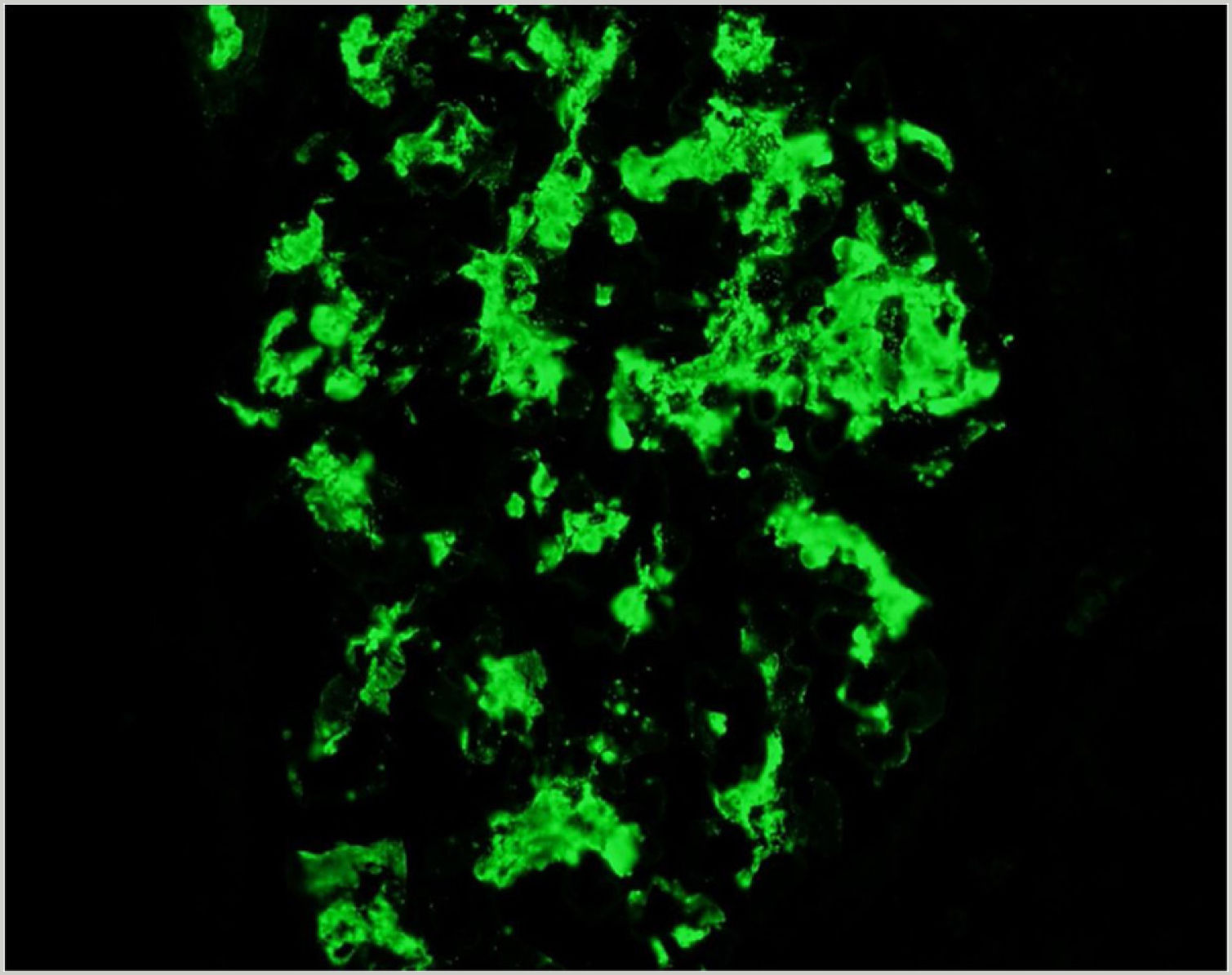
He had normal renal function and dysmorphic urinary red blood cells. Due to persistent macroscopic haematuria, a percutaneous renal biopsy was performed and IgA deposits were found on immunofluorescence (Fig. 1).
Steroid treatment was started at a dose of 1 mg/kg for three months in combination with losartan. The patient had very early complete remission, on the second day after starting treatment. He has normal renal function and no relapses 10 years later.
Case 2A 58-year-old woman, with a personal history of Hashimoto’s thyroiditis and hypothyroidism, was seen in the nephrology department for continuous macroscopic haematuria of 15 days’ duration.
Blood tests showed normal renal function; urine showed abundant dysmorphic red blood cells and red blood cell casts.
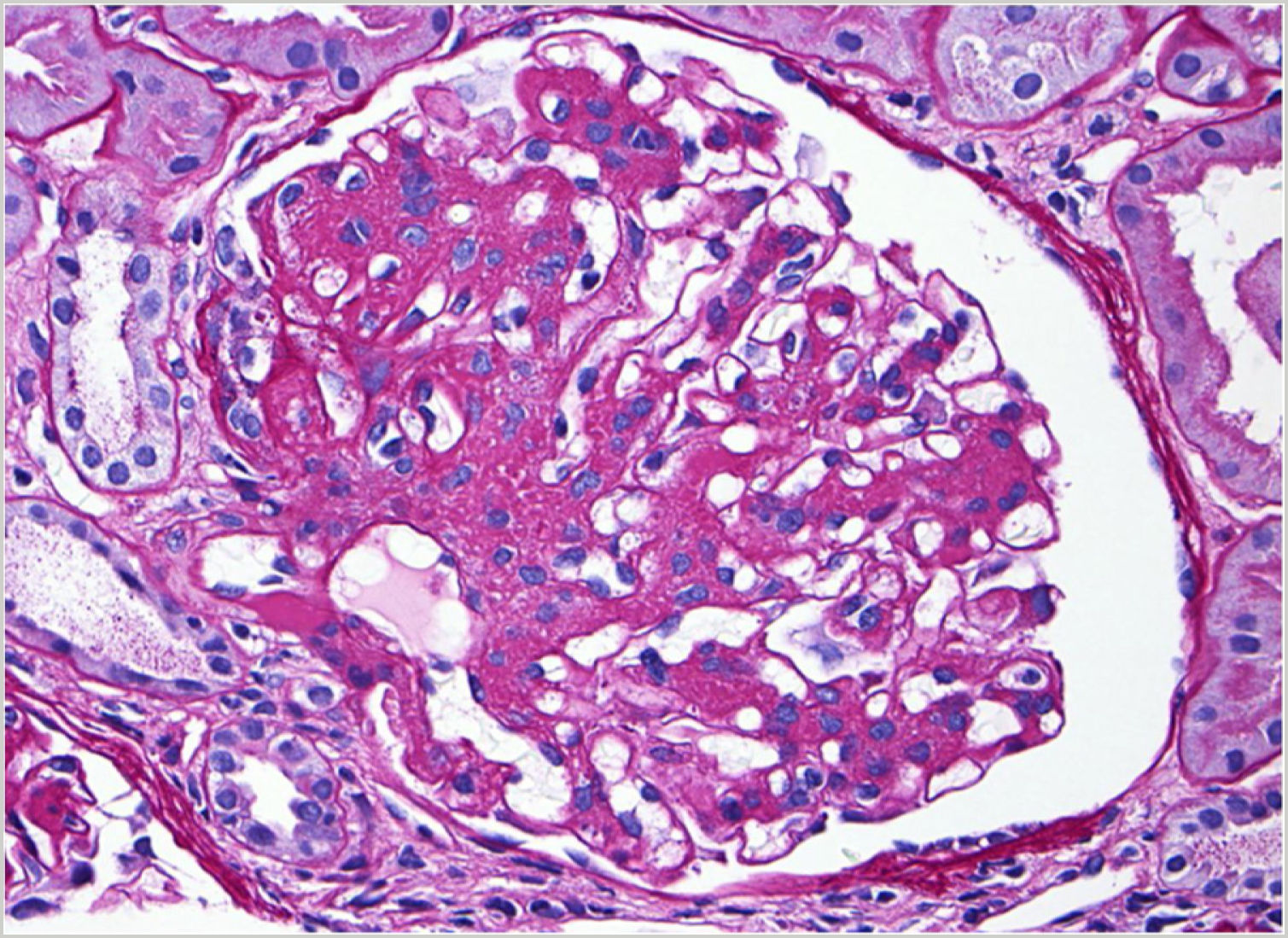
Given the persistence of macroscopic haematuria, a renal biopsy was performed: IgA mesangial nephropathy, with findings on light microscopy (Fig. 2).
Steroid treatment was started at a dose of 1 mg/kg for three months in combination with telmisartan. The patient had early complete remission on the third day after the start of treatment. She has normal renal function, with no relapses, three years and eight months later.
Case 3A 53-year-old woman was admitted to the nephrology department for continuous macroscopic haematuria of 22 days’ duration.
Nephrological studies showed normal renal function; the urinary sediment showed abundant dysmorphic red blood cells and red blood cell casts.
Oral steroid treatment was prescribed at a dose of 1 mg/kg for three months in combination with irbesartan. The patient had early complete remission on the second day of treatment, with no relapses and good renal function 16 months later.
IgA mesangial disease is a very common glomerular disease.5 The most characteristic clinical sign is haematuria, although presentation as a bout of macroscopic haematuria persisting over several days in the absence of crescents is uncommon.6 Few prognostic data are available for this form of manifestation.
In terms of treatment, steroids are known to be the first choice when the disease shows signs of poor prognosis, such as nephrotic proteinuria, renal failure or arterial hypertension.
In our cases, all three patients had rapid complete remission when treatment was instituted and are relapse-free to date.
Conflicts of interestThe author has no conflicts of interest to declare.
I would like to thank Dr Enrique Morales Ruiz (Nephrology, Hospital 12 de Octubre, Madrid, Spain), for his collaboration on the paper.