The Spanish Society of Nephrology (S.E.N.) has invited me to participate in a debate on the subject of phosphate binders, defending the position that when prescribing a certain phosphate binder, drug selection is determined by price. Dr Elvira Fernández will take the opposing position. Before beginning, I must say that I feel comfortable with this task, since I am firmly convinced that price is very important when it comes to prescribing a phosphate binder.
First of all, let us consider the current state of the economy in Europe, and in Spain in particular. The sustainability of Spain’s national health system is at risk. These are difficult times and we must decide how to plan for our future; it is clear that many things cannot go back to the way they used to be. Our contributions do not match our expenditure, and both markets and international institutions are reluctant to finance our chronic deficit. Budget cuts are therefore being applied, and the entire health system is feeling the effects.1 It is obvious that nephrologists, the doctors mainly responsible for prescribing these compounds to control hyperphosphataemia, act in a clinical management role: our decisions may lead to an imbalance in the medical services that our system offers to society. This is why the debate is so important.
IS CONTROLLING PHOSPHATE NECESSARY?
Block et al2 studied 40 538 patients on haemodialysis and found an association between phosphate levels above 5mg/dl and increased relative risk of death. These findings were also corroborated by a European database (ARO) which examined 7970 patients on haemodialysis from 172 dialysis units in 11 European countries. As a result, the association between high phosphate levels and mortality is clear. We must highlight however, that there are no studies that show that lowering phosphate levels in patients on dialysis is associated with a decrease in the relative risk of death. At this time, one of the most important recommendations in all clinical guidelines is that we must maintain phosphate levels below 5mg/dl.
CAN WE CONTROL PHOSPHATE AND AVOID ADDITIONAL COSTS?
The possibility of controlling phosphate with diet is quite low for dialysis patients, unless they consume abnormally high amounts of phosphate-rich foods such as dairy products. Prolonging the duration of the dialysis session results in good control over phosphataemia, and well-controlled serum phosphate levels have been observed after long-duration nocturnal dialysis sessions with practically no use of phosphate binders.4 Obviously, this technique is not an option for most of our population, and we must therefore resort to phosphate binders to prevent phosphate absorption.
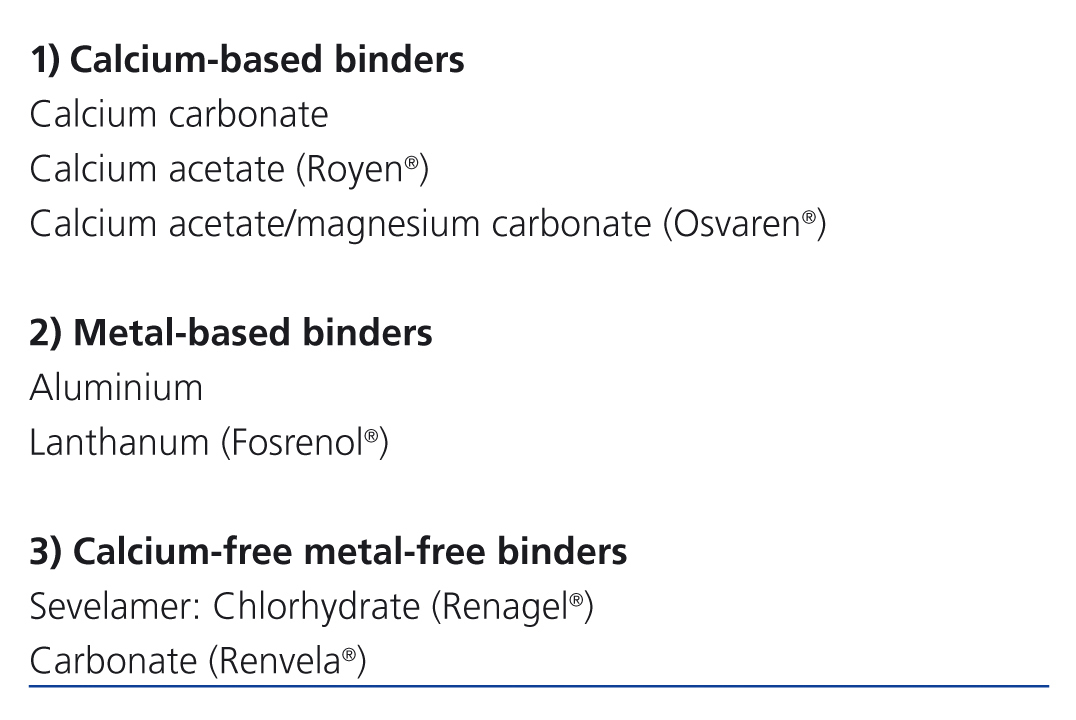
The ideal phosphate binder must meet a series of requirements: it must be effective, minimal absorption, have few side effects, reduced number of tablets taken, and be inexpensive. None of the binders currently used meets all of those conditions. Table 1 lists the different types of phosphate binders that are currently available.
ARE THERE DIFFERENCES IN EFFICACY BETWEEN BINDERS?
All studies show that when taken in proper doses, all phosphate binders reduce serum phosphate levels, meaning that their potency is similar. If we refer to comparative studies that include calcium components, lanthanum, sevelamer and calcium acetate/magnesium carbonate, we observe that the mean reduction achieved at 4 weeks is approximately 2mg/dl for all studies. No differences can be found between the studies in which patients followed the treatment plan correctly.5-8
ARE SOME BINDERS MORE BENEFICIAL THAN OTHERS WITH REGARD TO MORBIDITY/MORTALITY?
Only one study (DCOR)9 is large enough to be able to examine mortality and morbidity. The study compares patients receiving sevelamer and those taking phosphate binders. The study includes 2103 patients on dialysis that were assigned to treatment with either sevelamer HCl or calcium (70% calcium acetate and 30% calcium carbonate). Preliminary analysis revealed no significant differences in mortality between the 2 groups, although the secondary analysis found some differences for patients older than 65 years who received sevelamer.
Most of these randomised studies have significant methodological limitations: data is missing, they are not double-blind and the rate of loss to follow-up is more than 50% in the most important ones. Similarly, most do not have a control group. However, we should be aware that the few placebo-controlled trials which have been described found that serum phosphate levels decreased when any type of phosphate binder was administered, as stated before.
A recent Cochrane collaboration study10 that included 60 studies with 7631 participants concluded that sevelamer and lanthanum carbonate are no better than calcium salts for controlling phosphate levels in patients on dialysis, and that their impact on morbidity and mortality was unknown. Nevertheless, it has also been observed that calcium-free products have the advantage of reducing the percentage of hypercalcaemia. With this in mind, we must point out that studies on calcium components have changed in recent years. While early studies11-12 documented intake of 2 to 3.5g/day of calcium, the daily amount of calcium provided by calcium-based phosphate binders has decreased significantly since then. In our prospective randomised study comparing calcium acetate/magnesium carbonate with sevelamer HCl, the maximum amount of ingested calcium did not exceed 750mg calcium/day.8 There was no increase in ionic calcium or differences in hypercalcaemia episodes. Keep in mind that KDOQI13 guidelines state that the intake of calcium from calcium binders should not be greater than 1500mg/day.
ARE CALCIUM-BASED BINDERS RESPONSIBLE FOR VASCULAR CALCIFICATION?
Kalpakian et al14 analysed studies conducted between 2002 and 2005 in patients on haemodialysis and observed that detectable levels of calcification in coronary arteries were present in most patients (between 53% and 92%). It is obvious that this high percentage of calcification would not necessarily be linked to consumption of calcium-based binders. While it is true that there is a high correlation between vascular calcification and high serum calcium and phosphate levels, other important factors are also at work. These include: 1) loss of calcification inhibitors; 2) bone formation induced by abnormal differentiation of smooth muscle fibres; 3) formation of circulating nucleational complexes derived from bone undergoing continuous remodelling; 4) cell death that releases apoptotic bodies or necrotic waste which can cause apatite nucleation at sites of injury.15
But the factors listed above are not the only ones that may cause vascular calcification. Also involved are time on dialysis, race, presence of diabetes mellitus, and other more modifiable factors such as high vitamin D levels, dyslipidaemia, hypertension, consumption of alcohol and tobacco, etc. Therefore, the association of vascular calcification with the intake of calcium-based phosphate binders, which ultimately introduce a very low amount of calcium, as well as the anti-calcium approach promoted by the calcium-free binder industry, need to be revised in the context of evidence-based medicine. The CARE 2 study provides an example of involvement by factors other than calcium consumption. This study compared sevelamer with calcium acetate plus atorvastatin, reporting that levels of low-density lipoproteins remained below 70mg/dl in both groups. In this randomised study of 203 patients on haemodialysis, no other differences were observed with regard to the prevention of coronary artery calcifications, which highlights the significant effect which hyperlipidaemia has on calcification genesis.6
THE FORGOTTEN PROCESS: VASCULAR CALCIFICATION DURING HAEMODIALYSIS
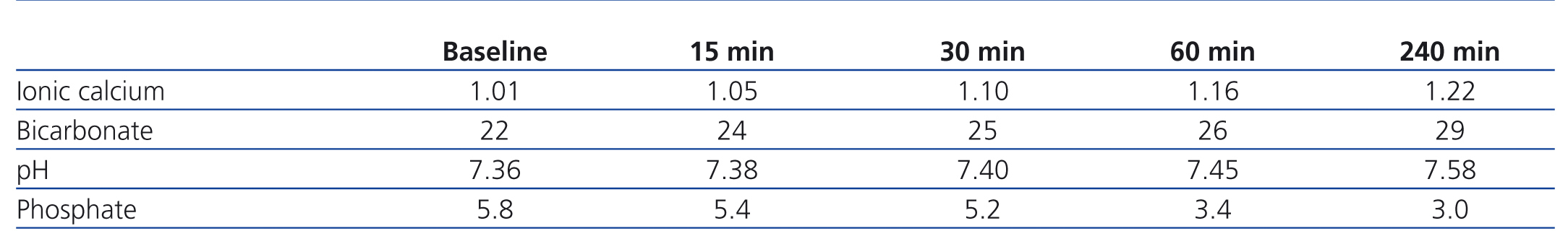
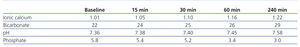
In vitro studies conducted with rat aortas16 have observed that in phosphate-rich media, elevated calcium levels induce vascular calcification, and this effect is intensified in an alkaline medium. Do you remember at what time a dialysis patient would be experiencing increases in ionic calcium, blood alkalinity and serum phosphate levels? See Table 2, which shows results from 12 patients in our Haemodialysis Unit in Santander dialysed against a 1.25mmol/l calcium and 35 mmol/l bicarbonate bath. At baseline, before initiating dialysis, the mean ionic calcium was 1.01mmol/l, with a pH of 7.36 and a phosphate level of 5.8mg/dl. As dialysis progresses, ionic calcium will increase until reaching 1.29mmol/l by the end of the session; pH will go from 7.36 to 7.58 and phosphate, which was initially at 5.8mg/dl, will decrease throughout the session. During the first half of the haemodialysis session, however, until phosphate levels decrease, the patient provides an exact reproduction of what causes vascular calcification according to the in vitro studies mentioned above. In light of this situation, we must be more aware of the mineral changes taking place during dialysis before involving modern calcium-based binders in vascular calcification in our patients.
VASCULAR CALCIFICATION AND MAGNESIUM
Clinical evidence indicates that dialysis patients with higher magnesium levels experience less vascular calcification, reduced intima-media thickness, less mitral calcification and less progression of arterial calcification than those with lower magnesium levels.17 In a study of 390 non-diabetic patients treated with haemodialysis, Ishimura18 showed with limited radiological methods that serum magnesium levels were significantly lower in patients with vascular calcification compared to those without calcification.
Recent studies by Rodríguez et al (currently unpublished), which were carried out in Córdoba and presented at the ERA-EDTA Congress in June 2011,19 used aortic rings to show that magnesium plays a protective role in vascular calcification. The conclusions reached by this research team are that in addition to decreasing vascular calcification, magnesium also promotes reversal of the condition. The future will reveal the importance of this phosphate binder associated with calcium acetate and its effects on vascular calcification, which are truly promising according to these studies and the clinical reports mentioned above.
DO PHOSPHATE BINDERS HAVE DIFFERENT SIDE EFFECTS?
It appears that there are no differences between different compounds, although sevelamer causes more gastrointestinal problems. Hypercalcaemia incidence rates are 13% in patients treated with sevelamer, 6% with lanthanum carbonate, 10% with calcium carbonate and calcium acetate, and 8% with magnesium carbonate/calcium acetate.8,20,21
ARE THERE PRICE DIFFERENCES BETWEEN PHOSPHATE BINDERS?
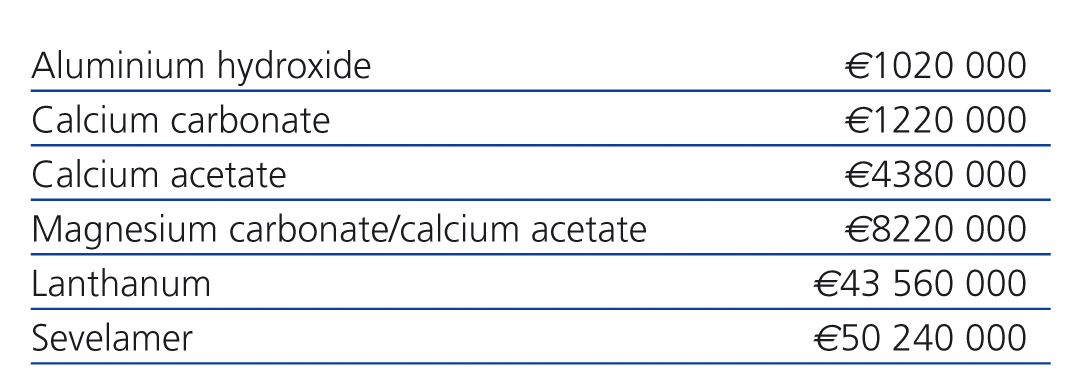
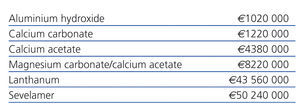
If we calculate the maximum number of tablets a patient may consume per day, the cost of treatment with aluminium hydroxide (prescribed exclusively for rescue treatment in a patient with uncontrolled hyperphosphataemia during limited time periods) amounts to €51 per year. Other treatment costs would be as follows: calcium carbonate, €61/year; calcium acetate, €219/year; magnesium carbonate/calcium acetate, €411/year; lanthanum carbonate, €2178/year; and sevelamer, €2512/year.
Let us imagine that out of 25 000 patients on haemodialysis in Spain, 20 000 needed phosphate binders, and all of these patients were treated with only one of these drugs. Of course, this situation is completely hypothetical, but for the sake of argument, see Table 3 for the exact annual cost in Euros of treating these patients. I repeat that this is merely a virtual construct, but it does adequately reflect the importance of the economic component in a nephrologist's decision-making process.
SHOULD SEVELAMER AND LANTHANUM BE RECOMMENDED AS INITIAL TREATMENTS?
The recent Cochrane review10 and the article by Tonelli in the New England Journal of Medicine20 state that calcium-based agents should be chosen as the first line of treatment, due to being less expensive, better-tolerated and equal in performance to sevelamer and lanthanum carbonate. As a result, in the absence of proven clinical benefits, sevelamer and lanthanum carbonate cannot be recommended as initial treatments.
RECOMMENDATIONS
In light of the above, when faced with a patient with hyperphosphataemia and reviewing diet and dialysis efficacy, my recommendations are as follows:
1) First choice: calcium acetate/magnesium carbonate (provided that magnesium levels are below 3.5mg/dl) or calcium acetate.
2) Sevelamer or lanthanum carbonate only under the following circumstances:
- Parathyroid hormone level below 120pg/ml
- Calcium level above 10.2mg/dl
- Associated with calcium products due to lack of phosphate control
CONCLUSIONS
1. We must reflect on cost-effectiveness when prescribing medicines in order to protect our National Health System.
2. There are no differences in potency, side effects, morbidity or mortality among phosphate binders, but cost differences are indeed present.
3. Calcium content has been reduced considerably (below the upper limits recommended by guidelines) in the most modern calcium-based binders.
4. In the absence of larger and more precise studies, known data currently suggests that magnesium prevents and reduces vascular calcification.
5. The problem of vascular calcification induced during the early hours of a dialysis session has not yet been sufficiently studied.
In conclusion, selection of phosphate binders is indeed determined by price.
Conflicts of interest
The author affirms that he has no conflicts of interest related to the content of this article.
Table 1. Phosphate binders currently in use
Table 2. Mean values in 12 patients in our Haemodialysis Unit dialysed against a 1.25mmol/l calcium and 35 mmol/l bicarbonate bath
Table 3. Annual cost of treating 20 000 patient on haemodialysis, in the hypothetical case that all of them receive the same treatment