Pica is an individual entity in the patient with chronic kidney disease (CKD), which phenomenon has not been widely studied despite the high reported prevalence. Moreover, pica complications (anaemia, altered electrolytes, poor absorption of micro and macronutrients and malnutrition) could be exacerbated in CKD and limit the quality of renal replacement therapy.
The intake of non-caloric and non-nutritional substances could be harmful and cause effects on satiety and metabolic/electrolyte imbalance and modify the biocompatibility of micronutrients, toxins and pathogens worsening health status.
In daily practice, pica could be under-reported because patient's shame to recognise it, or fear that such behaviour influences their treatment. Additionally, clinicians who not investigate the presence of pica or its complications contribute to the lack of information about the magnitude and relevance of this problem in CKD.
La pica como entidad individual en el paciente con enfermedad renal crónica (ERC) no ha sido ampliamente estudiada, a pesar de que se ha reportado una alta prevalencia en esta población, y de que las complicaciones propias de la pica (anemia, alteración en electrolitos, mala absorción de micro y macronutrientes y desnutrición) podrían verse exacerbadas en la ERC, lo cual limitaría alcanzar una mejor calidad de la terapia de remplazo renal.
La ingesta de sustancias no calóricas y no nutricionales podría ser perjudicial por los efectos en la saciedad y en el descontrol metabólico/electrolítico, y por afectar la biocompatibilidad de los micronutrientes, toxinas y patógenos, lo que finalmente puede empeorar el estado de salud.
En la práctica diaria es posible que la pica resulte subreportada debido a la vergüenza del paciente a reconocerlo, o el miedo a que dicho comportamiento pueda influir en su tratamiento. Adicionalmente, los clínicos, al no investigar la presencia de pica o sus complicaciones contribuyen a la falta de información acerca de la magnitud y la relevancia de este trastorno de la conducta alimentaria en la ERC.
Depending on which discipline is studying pica, it has been interpreted as an eating disorder, a behavioural problem, a symptom of mental illness, an expression of nutrient deficiency, abandonment, neglect, poverty or hunger and, from a cultural point of view, (not a disorder) as a “beneficial” adjustment; at times a cause and other times a consequence, at times a well-defined entity and other times a non-specific symptom of some underlying process. The complications of pica found in the general population can be exacerbated in patients with chronic kidney disease (CKD), as some of these problems already occur as a result of the kidney damage. For example, pica can cause severe anaemia, electrolyte imbalance and problems absorbing micro and macronutrients. It may also lead to exacerbation of malnutrition, although that and the worsening of ingestion remain unproven due to the lack of scientific articles on this subject.1
With this article we present the current evidence on the characteristics, frequency and consequences of pica in patients with CKD. To identify studies assessing the presence of pica and associated factors in patients with CKD, we carried out a search in the databases Medline, Embase, Cochrane Database, EBSCO, Psychology and Behavioral Sciences Collection and PsycINFO, with combinations of the following set of keywords: pica, eating disorder, rumination syndrome, chronic kidney disease, kidney damage, renal failure, nephropathy, dialysis, renal replacement therapy, epidemiology, prevalence, risk factors, consequences, complications. To include as much information as possible, there was no restriction on time frame or place of publication, as long as they were published in English or Spanish, as we did not have the support of translators from other languages. The results of our literature search are described throughout this article.
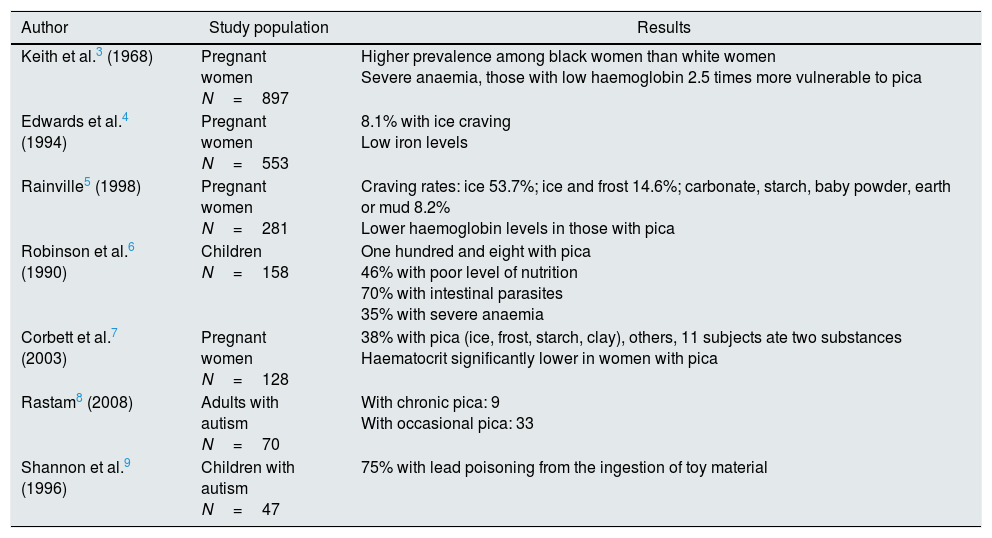
Epidemiology of picaPica is one of the most dangerous self-destructive behaviours of people with mental disorders. Unfortunately, in up to 30% of cases seen for this type of complication, the history of pica is unknown, meaning they had not been diagnosed prior to this episode. More importantly, we know that 37% of patients are repeat offenders, i.e. they are being treated for a new episode even though they were on treatment, and this highlights the great difficulty of completely eliminating this type of behaviour.2Table 1 shows a list of epidemiological studies3–9 in populations vulnerable to pica (pregnant women, children and subjects with autism) and their clinical and pathophysiological findings. Studies on pica and pregnancy show that most pregnant women with pica have low haemoglobin and haematocrit levels and iron and zinc deficiencies. In children with pica, however, more common findings are malnutrition, intestinal parasitic disease and anaemia. As we will discuss below, there are some similarities between these populations and patients with CKD, particularly in terms of having anaemia.
Epidemiology of pica in vulnerable populations.
| Author | Study population | Results |
|---|---|---|
| Keith et al.3 (1968) | Pregnant women N=897 | Higher prevalence among black women than white women Severe anaemia, those with low haemoglobin 2.5 times more vulnerable to pica |
| Edwards et al.4 (1994) | Pregnant women N=553 | 8.1% with ice craving Low iron levels |
| Rainville5 (1998) | Pregnant women N=281 | Craving rates: ice 53.7%; ice and frost 14.6%; carbonate, starch, baby powder, earth or mud 8.2% Lower haemoglobin levels in those with pica |
| Robinson et al.6 (1990) | Children N=158 | One hundred and eight with pica 46% with poor level of nutrition 70% with intestinal parasites 35% with severe anaemia |
| Corbett et al.7 (2003) | Pregnant women N=128 | 38% with pica (ice, frost, starch, clay), others, 11 subjects ate two substances Haematocrit significantly lower in women with pica |
| Rastam8 (2008) | Adults with autism N=70 | With chronic pica: 9 With occasional pica: 33 |
| Shannon et al.9 (1996) | Children with autism N=47 | 75% with lead poisoning from the ingestion of toy material |
The term “pica” comes from the Latin word for the magpie, a bird belonging to the crow family whose scientific name is Pica pica.10
The Diagnostic and Statistical Manual of Mental Disorders [DSM], version five (DSM-V), identifies pica as a term used to define a disturbance of eating or eating-related behaviour, which is characterised by its relationship with emotional or mental disorders,11 for which pica is defined as persistent eating of a substance(s) or object(s) with no calories or nutritional properties for at least one month in the last year, when it is not associated with a cultural and/or community practice and when it is considered inappropriate for the person's stage of development. Furthermore, if the eating behaviour occurs in the context of another mental disorder (e.g. intellectual disability, autism spectrum disorder, schizophrenia) or medical condition (including pregnancy and CKD) it is serious enough to warrant additional clinical attention.11
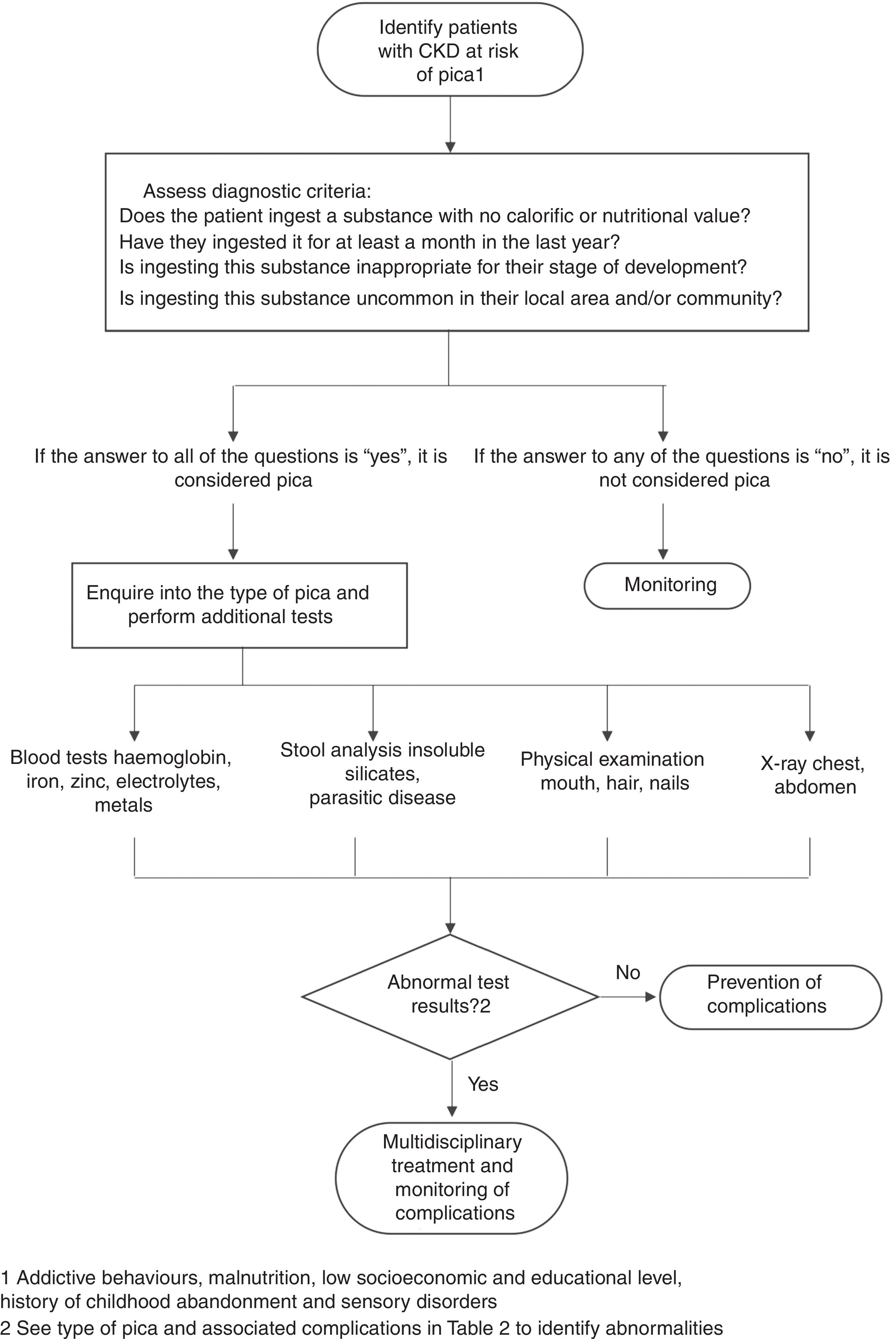
Treating physicians who suspect pica in their patients or who identify associated risk factors should evaluate them with the DSM-V to verify the diagnosis of pica, identify the substance ingested and control the symptoms. Fig. 1 shows an algorithm for the diagnosis of pica. The physical examination is one of the most important investigations for identifying the type of pica and/or related complications and should include exploring for signs and symptoms such as hair and nail loss, broken teeth, gingivitis, mouth ulcers and/or foreign bodies in the mouth. Blood analysis can be useful to identify anaemia, nutrient deficiency, electrolyte imbalance and/or impaired liver function. Testing of stools can identify the presence of parasites and/or of insoluble silicates eliminated 24–48h after the last meal.12 In some cases, chest or abdomen X-rays may be necessary to identify foreign objects or coins, or the presence of earth and/or hair.13
Even with all the above tests, in most cases the clinical findings are non-specific, and diagnosis of pica then requires the patient (or family member) to admit the persistent behaviour. As there may be stigma attached to the diagnosis, the interview should be directed by a healthcare professional, aiming to use a non-judgmental approach to questioning the patient, and so help them to admit their problem more readily.13 Moreover, patients will often not have typical signs and symptoms any different from the underlying disease with which the pica may be associated, so skill and clinical acuity are essential. The most common scenario is that the diagnosis is not made until pica-related complications arise.1
The identification and monitoring of patients with pica is currently inadequate and healthcare personnel are wholly unprepared in terms of knowledge and training to identify this type of disorder at an early stage. This results in the complications and consequences spiralling out of control, even within healthcare institutions.14
Causes and consequences of picaAlthough pica has been studied by anthropologists, geographers, paediatricians, gynaecologists, haematologists, psychiatrists, psychologists, nutritionists, etc., the reality is that nobody knows what causes it.12 Suggested causes include nutritional deficiencies and social and psychological situations. However, at least in some patients, one of the main pathophysiological explanations for pica is addictive behaviour (similar to that of nicotine), as the behaviours/cravings often continue long after the physiological cause is resolved.15 It has been demonstrated that the behaviour persists even after the psychological cause is treated and alleviated. Moreover, if pica was always caused by nutritional deficiencies, it should stop when they are corrected, but that is not usually the case.16
Stillman and Gonzalez17 point to pica as a manifestation of obsessive-compulsive disorder. They state that patients on dialysis who display pica behaviours can consume a large number of substances which are associated with the alteration in their metabolic functions, although this is not always reflected in abnormal laboratory values.
CKD can be a powerful factor for emotional stress, and may therefore stimulate the onset of pica, especially in patients with a cultural predisposition.18 Patients with pica have described their behaviour as ritualistic and compelling, and their consumption as providing relief from anxiety.19 For example, in the Cooksey et al. study20 the patients stated that eating ice helped them when they felt stressed.
In general, factors such as abandonment and lack of supervision of children and people with disabilities by parents, poverty, hunger, gastrointestinal discomfort (for example nausea and vomiting), increased saliva production, and altered taste and smell have all been implicated in the origin and perpetuation of pica.11,21
Unlike the causes of pica, the complications are well documented. Of the complications of pica which occur in pregnant women, children and people with autism, Maravilla and Berk22 identified four types which can be of particular concern from a nephrology point of view: (1) toxicity of the substances (for example, lead or other substance poisoning); (2) gastrointestinal obstruction (for example due to consumption of hair, earth and/or stones); (3) excessive calorie consumption (for example, starch craving); (4) calorie deprivation because the ingested substance contains no calories and also suppresses the appetite (for example, ice consumption).
One of the most remarkable complications is the formation of bezoars (masses of indigestible substances that cannot progress and are isolated or trapped in gastrointestinal cavities); one of the most serious of these is Rapunzel syndrome (mass of hair anchored in the stomach that projects to the small intestine), found in children and people with mental disorders or with trichotillomania and/or trichophagia.23
In view of the impact of pica-related behaviours on the health of patients with CKD, from electrolyte imbalance to poor intake of food and adherence to diet because they feel sated from eating other substances such as ice or earth, and prefer their substance of choice to the diet prescribed by their health practitioner, healthcare personnel have to be able to detect patients with pica and prevent the associated complications and risk of malnutrition.24
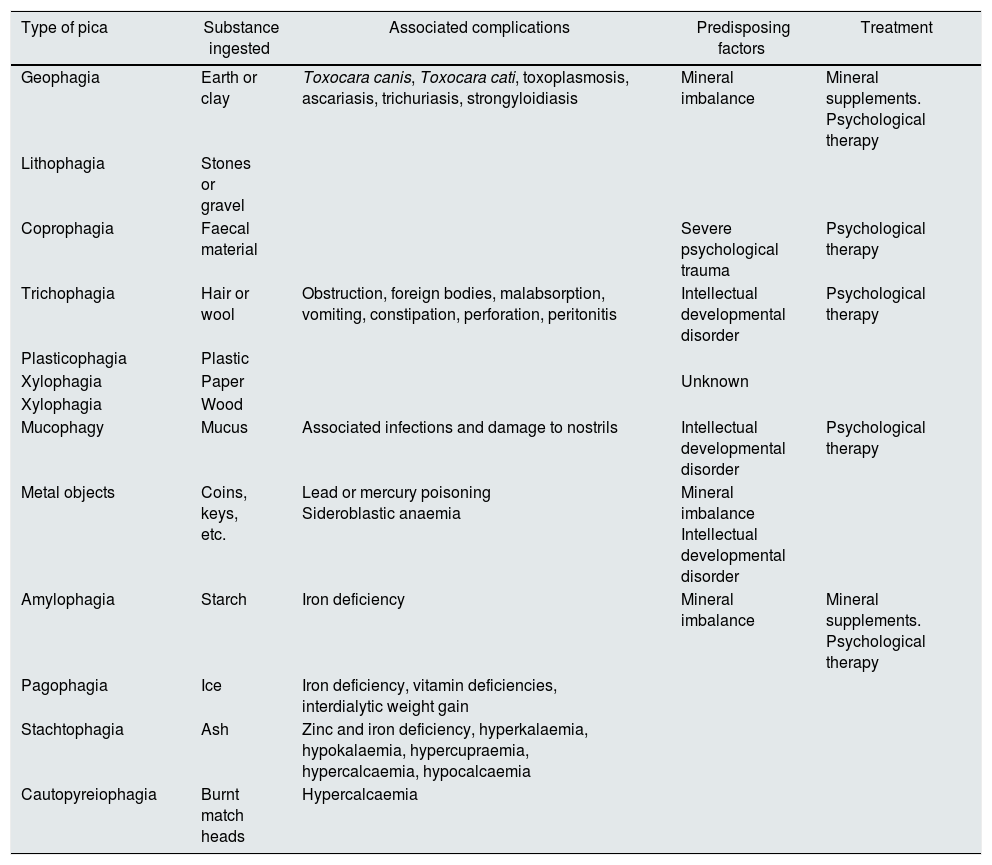
Treating picaTreatment of pica has to address the causes and consequences. Table 2 shows a summary of the treatment25 according to the type of pica, along with complications and predisposing factors. Psychopharmacology experts believe that there is no specific drug for treating pica. Generally, the use of drugs is in accordance with the psychiatric illness, with behavioural disorders predisposed to treatment and/or they are part of a comprehensive approach that includes psychological, social and educational measures.
Types of pica and their characteristics.
| Type of pica | Substance ingested | Associated complications | Predisposing factors | Treatment |
|---|---|---|---|---|
| Geophagia | Earth or clay | Toxocara canis, Toxocara cati, toxoplasmosis, ascariasis, trichuriasis, strongyloidiasis | Mineral imbalance | Mineral supplements. Psychological therapy |
| Lithophagia | Stones or gravel | |||
| Coprophagia | Faecal material | Severe psychological trauma | Psychological therapy | |
| Trichophagia | Hair or wool | Obstruction, foreign bodies, malabsorption, vomiting, constipation, perforation, peritonitis | Intellectual developmental disorder | Psychological therapy |
| Plasticophagia | Plastic | |||
| Xylophagia | Paper | Unknown | ||
| Xylophagia | Wood | |||
| Mucophagy | Mucus | Associated infections and damage to nostrils | Intellectual developmental disorder | Psychological therapy |
| Metal objects | Coins, keys, etc. | Lead or mercury poisoning Sideroblastic anaemia | Mineral imbalance Intellectual developmental disorder | |
| Amylophagia | Starch | Iron deficiency | Mineral imbalance | Mineral supplements. Psychological therapy |
| Pagophagia | Ice | Iron deficiency, vitamin deficiencies, interdialytic weight gain | ||
| Stachtophagia | Ash | Zinc and iron deficiency, hyperkalaemia, hypokalaemia, hypercupraemia, hypercalcaemia, hypocalcaemia | ||
| Cautopyreiophagia | Burnt match heads | Hypercalcaemia |
Adapted from Viguria et al.25
One common psychological treatment is the application of aversive stimuli (for example the aversion to taste technique, where a bitter substance is mixed with the material consumed by the patient and they then develop an aversion to it). However, this has to be complemented by other psychoeducational strategies which aim to involve the patient in the process and help them understand more about pica and the associated risks.25 Some cognitive/behavioural treatment strategies applied in other disorders can be adapted for the treatment of pica26; by identifying what is going through the patient's mind when they start eating the non-food substances, it can be possible to modify this behaviour. It is also important to identify emotions and behaviours patients have as consequences of their dysfunctional thoughts, in order to help them restructure the underlying cognitive schemas.25 The inclusion of nutritionists, family support groups, motivational interviewing, anxiety management techniques, training in social skills and assertiveness training, individual therapy when necessary and prevention of relapse are basic elements in the treatment of pica. A multidisciplinary intervention of this type tends to be more effective than psychopharmacotherapy as a sole treatment.11 In any event, there is no one single method of treatment. What is essential is the work of a professional team prepared to investigate and take into account biological, psychological and social factors, who also understand the magnitude of the problem, how to approach it and the short- and medium-term consequences. Also important is educating the family and carers to give them basic ideas about how to control pica stimuli.26
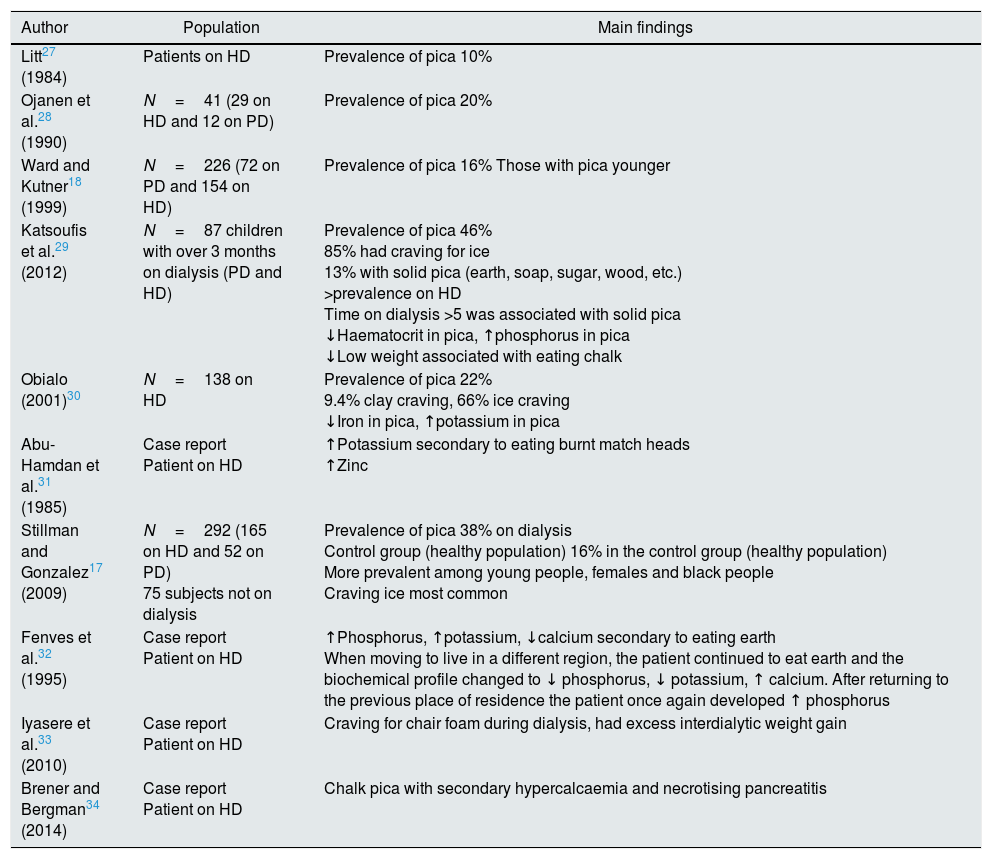
Evidence on pica in chronic kidney diseaseFew studies have analysed the epidemiology of pica in a population with CKD. The available evidence is only in patients on long-term dialysis, haemodialysis (HD) and peritoneal dialysis (PD), and most of the information in this area comes from case reports. Table 3 shows the main results of studies performed in patients on dialysis, in whom the prevalence of pica varies from 10% to 46%17,18,27–34: Stillman and Gonzalez17 reported 38% in their sample of 292 subjects with dialysis; Obialo30 reported 22% in a sample of 138 African-Americans on haemodialysis; Katsoufis29 found a prevalence of 46% in a paediatric population of 87 children; Ward and Kutner18 a prevalence of 16% in 226 incident patients on replacement therapy; Ojanen28 found that among 41 patients assessed, 20% had some type of pica; and, lastly, Litt et al.,27 in the oldest study found published in 1984, reported a rate of 10%. However, Litt et al.27 did not specify how the individuals were questioned, which calls into question the validity of the results. Most studies include population on HD, and the main form of pica is the consumption of ice. In the majority of cases, low haemoglobin and haematocrit levels were found, as well as electrolyte concentration abnormalities, although with no well-defined pattern.
Studies on pica in population with chronic kidney disease.
| Author | Population | Main findings |
|---|---|---|
| Litt27 (1984) | Patients on HD | Prevalence of pica 10% |
| Ojanen et al.28 (1990) | N=41 (29 on HD and 12 on PD) | Prevalence of pica 20% |
| Ward and Kutner18 (1999) | N=226 (72 on PD and 154 on HD) | Prevalence of pica 16% Those with pica younger |
| Katsoufis et al.29 (2012) | N=87 children with over 3 months on dialysis (PD and HD) | Prevalence of pica 46% 85% had craving for ice 13% with solid pica (earth, soap, sugar, wood, etc.) >prevalence on HD Time on dialysis >5 was associated with solid pica ↓Haematocrit in pica, ↑phosphorus in pica ↓Low weight associated with eating chalk |
| Obialo (2001)30 | N=138 on HD | Prevalence of pica 22% 9.4% clay craving, 66% ice craving ↓Iron in pica, ↑potassium in pica |
| Abu-Hamdan et al.31 (1985) | Case report Patient on HD | ↑Potassium secondary to eating burnt match heads ↑Zinc |
| Stillman and Gonzalez17 (2009) | N=292 (165 on HD and 52 on PD) 75 subjects not on dialysis | Prevalence of pica 38% on dialysis Control group (healthy population) 16% in the control group (healthy population) More prevalent among young people, females and black people Craving ice most common |
| Fenves et al.32 (1995) | Case report Patient on HD | ↑Phosphorus, ↑potassium, ↓calcium secondary to eating earth When moving to live in a different region, the patient continued to eat earth and the biochemical profile changed to ↓ phosphorus, ↓ potassium, ↑ calcium. After returning to the previous place of residence the patient once again developed ↑ phosphorus |
| Iyasere et al.33 (2010) | Case report Patient on HD | Craving for chair foam during dialysis, had excess interdialytic weight gain |
| Brener and Bergman34 (2014) | Case report Patient on HD | Chalk pica with secondary hypercalcaemia and necrotising pancreatitis |
All minerals and electrolytes mentioned are serum.
HD: haemodialysis; PD: peritoneal dialysis; ↑: elevation; ↓: decrease.
Anaemia is a common complication of CKD and is associated with an increased risk of cardiovascular disease, morbidity and mortality, particularly in the dialysis population. Although erythropoietin deficiency is the main cause, persistence of anaemia is multifactorial, with disorder of iron metabolism one of the most important and common factors.35 Pica may be related to the exacerbation of anaemia in patients with advanced CKD; for example, iron deficiency is three times more common among subjects who eat earth than in those who do not. Additionally, consumption of starch (another common form of pica) can prevent intestinal absorption of iron.36 Talkington et al.37 conducted an experimental study with 32 people and analysed the effect of eating earth and laundry starch on iron absorption; the results showed that after consuming these elements, the incidence of iron deficiency anaemia increased. The anaemia then improved after a modest dose of oral iron, even when the pica continued, with the patients consuming an average of 70g of starch a day.
In addition, the association between pagophagia (ice consumption) and anaemia, and its apparent improvement after iron therapy has been documented (subjects lose interest in eating ice after iron replacement).20 Some consider pagophagia to be a symptom of lack of iron.38 That would suggest that pica is a behaviour motivated by the lack of certain essential nutrients in the subject, implying the existence of a possible unknown compensatory mechanism, but that continues to remain a matter of discussion.
The association between pica and iron deficiency has been described in pregnant women, children and people with gastrointestinal blood loss, in whom iron administration resolves the pica in many cases, generally before the anaemia is corrected (which implies an independent mechanism). If, as described in this population, pica is resolved by correcting the iron deficiency, the mechanism of action needs to be investigated and explained.39
Electrolyte and nutrient imbalancesPica is characterised by an imbalance in eating habits, including inadequate intake of a number of different nutrients. Pica can cause micronutrient deficiency disease in three ways: (1) by replacing nutrient-rich foods with objects with no nutritional value; (2) by causing geo-helminth infection and secondarily due to poor absorption of nutrients or blood loss through the gastrointestinal tract; and (3) by preventing micronutrients from being usable by the body.36 Despite these possible mechanisms, there is no clear explanation for the association between pica and micronutrient deficiencies.
Zinc is one of the micronutrients to have been linked to pica. In samples of children and in case reports, administration of zinc has decreased episodes of pica.40 One study showed that 53% of patients with mental disabilities and pica had a zinc deficiency. These patients were compared to a group matched by age, intellectual level and years of institutionalisation, ensuring that both groups had a similar diet which complied with Food and Drug Administration recommendations. The findings suggested that consumption of earth may prevent adequate assimilation of zinc, as all the geophages suffered from zinc deficiency.41 Regardless of intellectual disability, iron deficiency and other factors, people with a zinc deficiency are 6.25-times more likely to suffer from pica.42 After documenting the resolution of a pica case following prescription of zinc sulphate, Lofts et al.43 suggested that abnormal zinc levels should be considered as part of the aetiopathogenesis of pica. Zinc has been linked to many functions and disorders, including anorexia.44 In experiments with rats, zinc deficiency leads to reduced intake and elevation of neuropeptide Y in hypothalamic nuclei.45 However, if zinc is in fact an aetiopathogenic factor in the development of pica, as in the case of iron, its mechanism of action is unknown.
Eating earth or clay, one of the most common types of pica, could contribute to the intake of some micronutrients such as potassium, calcium and/or phosphorus, depending on the composition of the earth. The subsequent effect on serum electrolytes could upset a delicate balance in patients with CKD.32
It has been demonstrated that the daily consumption of clay in an African-American community – an everyday practice – contributes an additional amount to the daily intake of potassium contained in food.24 Unfortunately, there have been no other studies on the effect of pica on plasma potassium concentrations46 in a healthy population or people with specific disorders such as CKD and/or on long-term dialysis, even though hyperkalaemia is one of the preventable causes of sudden death in these last two populations.
Pica-related poisoningAlthough pica may be described in some cases as a compensatory mechanism for nutrient deficiency, there is also an increase in the risk of poisoning, including the following: lead poisoning, resulting in hyperammonaemia with cerebral oedema and encephalopathy; zinc poisoning due to consumption of copper coins; sideroblastic anaemia associated with iron-based coins; and hypernatraemia from consuming too much sodium chloride. Other forms include both acute and chronic organophosphate poisoning; mercury poisoning associated with pica involving printed paper; and arsenic or aluminium poisoning in patients with geophagy. Other complications can be haemolytic anaemia caused by paradichlorobenzene.25 In the case of patients with CKD, the dialysis process cannot be guaranteed to remove these substances and prevent poisoning and this makes it particularly important to monitor the consumption of non-nutritive substances that place the patient at risk of poisoning.
Altered nutritional statusNutritional problems are common among patients on long-term dialysis. Some studies report that the rate of mild-to-moderate malnutrition in PD patients ranges from 30% to 35% and severe from 8% to 10%,47 while HD has an associated malnutrition rate of 24% to 37%.48 The prevalence of malnutrition in patients with CKD and pica has not been measured. None of the studies on pica have carried out a nutritional assessment as part of their procedures; only Katsoufis et al.29 associated their patients’ low weight with consumption of chalk.
Ice craving is the type of pica most reported in previously published studies.17,18,27–33 Eating ice may seem harmless, and sometimes it is encouraged by the treating physician to mitigate thirst control.49 However, compulsive ice consumption is recognised as pica19,30,32 and could contribute to inadequate fluid intake and loss of appetite18 and, subsequently, to negative effects on nutritional status. Excessive ice intake can generate up to an extra 750ml of water/day for the patient50 which can also lead to interdialytic weight gain,27 with the consequent increase in blood pressure, volume overload and increased cardiovascular morbidity and mortality rates.33
Perhaps the most important question that remains after this review is what role does pica play (including ice pica) in worsening of nutritional status and dietary intake? In particular, whether that is the cause or consequence of the chronic consumption of any of the above-mentioned substances. Because of the nature of the studies we found, is has not been possible to establish causality. It is therefore important for future observational follow-up studies to determine whether malnutrition is the cause or consequence of pica. It is also important to establish what relationship there is between pica and dietary intake, as it is possible that increased water consumption (ice craving) and lower nutrient consumption lead to deterioration in patients’ nutritional status over a long period of exposure. In addition to this, it is important to recognise that patients with solid pica and those who have cravings for more than two types of substance may be at risk of worse deterioration in nutritional status and dietary intake. However, that has not been assessed to date.
Gaps in our knowledge about pica in chronic kidney diseaseCKD can be a powerful factor for emotional stress, and that may act as a trigger for pica, especially in patients with a cultural predisposition.30 Due to the high prevalence of malnutrition and biochemical abnormalities in the population with CKD and dialysis, we need to identify the magnitude of pica and analyse its association with sociodemographic, clinical, biochemical and dietary factors, and so create the opportunity to establish the following strategies: (1) determine whether or not it is necessary to screen for pica; (2) identify factors that may be associated with the prevalence of pica and thus establish the necessary strategies to correct them; (3) determine whether or not pica is associated with the nutritional status of the patient on dialysis.
Key conceptsEstablishing the diagnosis of pica (persistent and compulsive consumption of objects that have no calorific value) in a patient can be particularly complex. The most common scenario is that the diagnosis is not made until pica-related complications arise.
The causes of pica have not been completely clarified; psychological and nutritional causes have been proposed.
The complications of pica are associated with the toxicity of the substances consumed, gastrointestinal obstructions and alterations in calorie intake, especially relevant in patients with CKD.
The presence of pica in the patient with CKD may have a greater impact on the complications of kidney damage, such as anaemia, electrolyte and nutrient imbalances and malnutrition.
Conflicts of interestThe authors declare that they have no potential conflicts of interest related to the contents of this article.
Please cite this article as: Orozco-González CN, Cortés-Sanabria L, Márquez-Herrera RM, Núñez-Murillo GK. Pica en enfermedad renal crónica avanzada: revisión de la literatura. Nefrologia. 2019;39:115–123.