Lupus podocytopathy (LP) is not included as a subtype in the classification of lupus nephropathy (LN) of the ISN/RPS 2003.1 Presently the frequency, prognosis and treatment of LP are not well established.2,3
We describe the case of a 34-year-old woman, with no prior medical history of interest, who presented severe thrombocytopenia and nephrotic syndrome, with no other associated symptoms. In the lab work, the following stood out: platelets 36,000/μl, hemoglobin 12.1g/dl, creatinine 0.61mg/dl, cholesterol 258mg/dl, serum albumin 2.7g/dl; haptoglobin and LDH were normal; proteinogram without significant alterations. In the urine, the sediment was normal with proteinuria of 7g/day, Bence Jones proteinuria was negative. Positive ANA at 1/320, anti-DNA IgG: 98IU/ml (normal value <15); anti-La was + and anti-Ro +++. Coombs, C3, C4, antiphospholipid antibodies, ANCA, anti-GBM, cryoglobulins, immunoglobulins, serologies for hepatitis B and C, HIV were normal or negative. The renal biopsy contained 42 glomeruli, 2 of them sclerotic, and in the majority there were no abnormalities at optical microscopy, only and very focal, in some glomeruli, there was minor mesangial proliferation. There were no tubulointerstitial or vascular abnormalities. In the immunofluorescence there were mesangial granular deposits of moderate intensity of IgG and negative for IgA, IgM, C3, C1q, kappa and lambda and fibrinogen. No electronic microscopy was available.
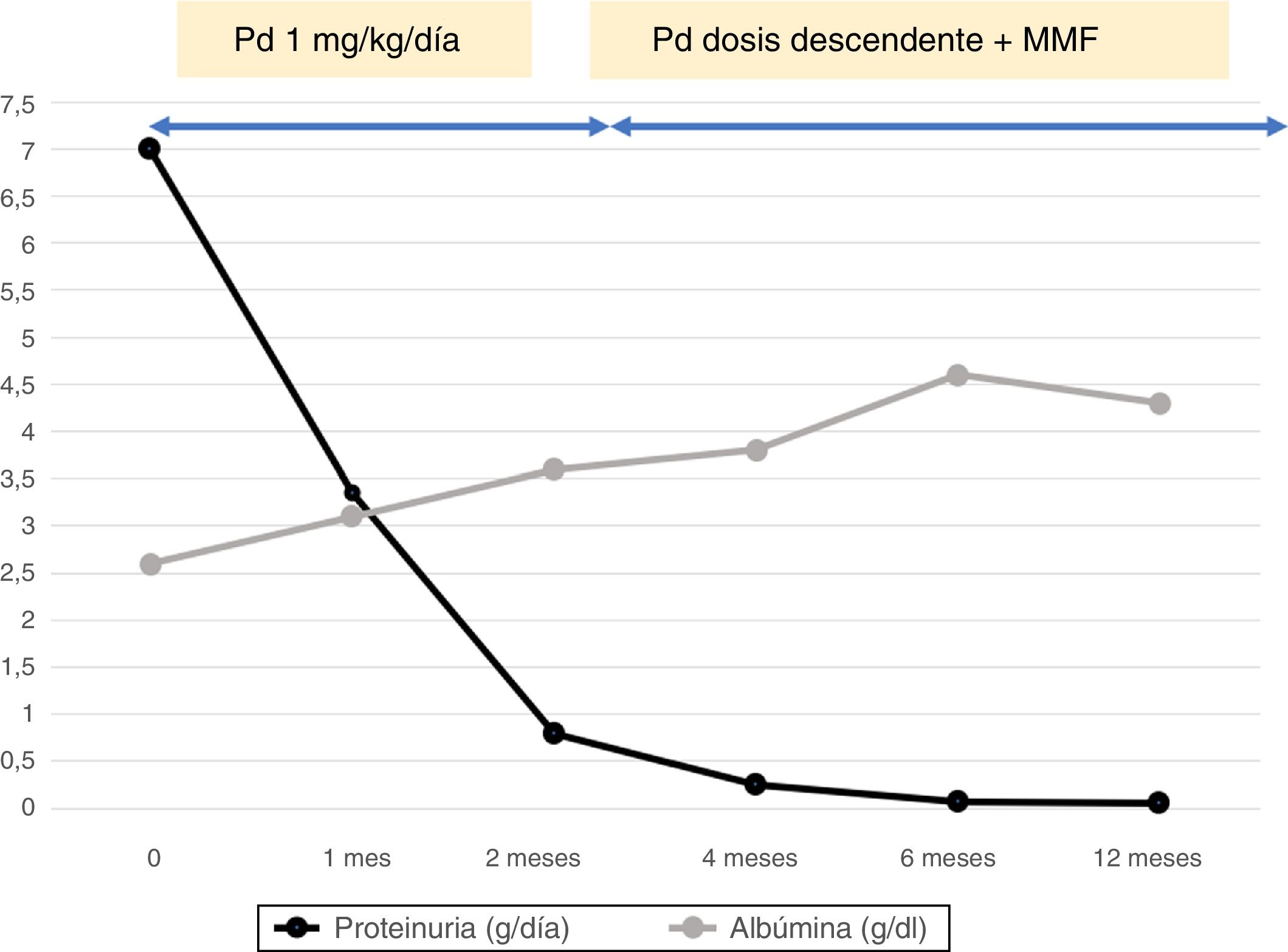
It was suspected the presence of LP and treatment with hydroxychloroquine and prednisone was started at a dose of 1mg/kg per day, which was maintained until 2 weeks after the remission of the nephrotic syndrome (achieved after 2 months of treatment) (Fig. 1). Then, the dose of prednisone was reduced slowly and progressively and mycophenolate mofetil was associated to the treatment. At month 18, the patient was still in complete remission, prednisone was discontinued and mycophenolate mofetil was maintained. Throughout the follow-up, the patient was normotensive, the glomerular filtration rate and complement were normal and the ANA and anti-DNA persisted positive, but at a lower level. Platelets recovered partially, after administration of romiplostim before the renal biopsy and, later, with the treatment, platelets remained in normal range throughout the follow-up. Besides these hematologic abnormalities there were no other extrarenal clinical manifestations.
The LP is characterized by nephrotic syndrome with normal glomeruli or with slight mesangial proliferation, or rarely, a segmental and focal glomerulosclerosis, in the context of a systemic lupus erythematosus (SLE). The essential criteria for the diagnosis are: (1) absence of endocapillary proliferation; (2) absence of deposits in the capillary wall (although they may exist in the mesangium) and (3) diffuse fusion of podocyte pedicels. In the presence of mesangial deposits, alone or accompanied by mesangial proliferation, some authors4 prefer to make the diagnose of LN type I or II, respectively, associated with podocytopathy. The LP usually presents at the beginning of SLE, and, generally, ANAs are positive, but anti-DNA may be negative and with a normal complement.5,6 Most frequently associated extrarenal manifestations are cutaneous and hematological.5,6
Our patient presented a nephrotic syndrome together with 3 criteria of SLE (thrombocytopenia, ANA and anti-DNA positive).7 In the biopsy, there was no endocapillary proliferation or thickening of the capillary wall and the IgG deposits were exclusively mesangial, which exclude proliferative (III, IV) and membranous LN (V). The presence of mesangial IgG indicated that it was not an idiopathic minimal change disease. Therefore, in spite of the lack of electronic microscopy, the diagnosis of LP was very likely, as opposed to an LN I/II with podocytopathy. With this diagnosis it is assumed that our patient presented an SLE7 with corresponding therapeutic implications. The treatment of LP is not definitively established.8,9 Although its prognosis is uncertain, relapse rate is high, which appear to be lower and later if one immunosuppressant is added to the treatment.5,6 So, in addition to the induction treatment, a maintenance treatment is probably required. Corticosteroids are used for induction, although the protocol is not definitely established.5,6,8,9 In our patient, remission was achieved at 2 months, after maintaining 1mg/kg/day of prednisone. Regarding maintenance treatment, there is not enough evidence to recommend any specific medication (anticalcineurinics, azathioprine, mycophenolate mofetil or ritxumab, among others).5,6,10 In the series by Hu et al.5,6 the few patients treated with mycophenolate mofetil did not relapse. In our case, after remission, mycophenolate mofetil was added, along with a progressive decrease in prednisone, until its suspension at 18 months, without a relapse.
The pathophysiologic relationship between podocytopathy and SLE is unknown, but identifying a LP has diagnostic and therapeutic implications, as our case shows. Finally, taking into account all the above considerations and the fact that cases of relapse have been described in which LP has been transformed into another type of LN, it would possibly be justified to include LP as a subtype in the LN classification. All this would allow, in the future, to define the frequency, prognosis and treatment for this condition.
Please cite this article as: Muray Cases S, Herranz Marín MT, Alcázar Fajardo C, Andreu Muñoz AJ, Cabezuelo Romero JB. Podocitopatía como inicio de un lupus eritematoso sistémico. Nefrologia. 2018;38:674–675.