Introducción: Las actuales guías recomiendan la medición periódica del flujo vascular (Qa). Los métodos actualmente validados son la ecografía-Doppler (ED) y la ultrasonografía dilucional. Objetivo: Analizar la aplicación práctica de la termodilución (TD) en la medición del Qa respecto a la ED. Material y métodos: Estudio transversal realizado en 64 pacientes (41 varones) en programa de hemodiálisis; 59,9 años con 54 FAVI y 10 politetrafluoroetileno (PTFE). El Qa de referencia se determinó por ED en la arteria humeral (fístula arteriovenosa [FAVI]) y en el tramo de punción arterial (PTFE). Para el análisis de concordancia se utilizó el método de Bland-Altman y el coeficiente de correlación intraclase (CCI). Resultados: El Qa obtenido por ED resultó 1426 ± 753 ml/min FAVI y 1186 ± 789 ml/min PTFE. Los valores obtenidos por TD fueron 1372 ± 770 FAVI (sesgo 54,6; CCI 0,923) y 1176 ± 758 PTFE (sesgo 10,2; CCI 0,992). En el subgrupo de 28 pacientes portadores de FAVI radio-cefálicas latero-terminales el Qa obtenido por ED resultó 1232 ± 767 ml/min. A nivel de la arteria radial 942 (CCI 0,805); arteria radial-cubital 1.103 (CCI 0,973); vena cefálica 788 (CCI 0,772) y TD 1026 (CCI 0,971). Se detectaron 5 estenosis significativas; Kt posrevascularización mediante catéter balón de angioplastia (ATP): 79 l (61; p = 0,043) y Qa-TD post-ATP 895 ml/min (663; p = 0,043). Conclusiones: La TD resultó un método indirecto automatizado útil en la medición del Qa. En el subgrupo de pacientes con FAVI radio-cefálicas resultó más preciso el sumatorio de flujo obtenido en arteria radial y cubital. Sin embargo, la TD también presentó una excelente correlación con la arteria humeral.
Introduction: The current clinical guidelines recommend indirect measurement of vascular access blood flow (Qa) as one of the most important components in vascular access maintenance programmes. The best-known methods are doppler ultrasound (DU) and saline dilution method. Objective: This study evaluates the efficiency of Qa measurement using the thermodilution method (TD) in comparison with DU. Material and Method: Cross-sectional study in 64 patients on haemodialysis (41 males); mean age: 59.9 years, with 54 AVFs and 10 PTFE. Qa reference values were obtained with DU in the brachial artery (AVFs) or at the zone of arterial puncture (PTFE). Bland-Altman and interclass correlation coefficients (ICC) were used to study accuracy. Results: Mean values obtained with DU-Qa were 1426 ± 753 mL/min for AVFs and 1186 ± 789mL/min for PTFE grafts. The mean Qa with TD was 1372 ± 770 for AVFs (bias: 54.6; ICC: 0.923) and 1176 ± 758 for PTFE (bias 10.2; ICC 0.992). In the 28 patients with radiocephalic side-to-end AVFs, the mean DU-Qa was 1232 ± 767mL/min. Qa values were measured in the radial artery: 942 (ICC 0.805); radial-ulnar artery: 1103 (ICC 0.973); cephalic vein: 788 (ICC 0.772), and with TD: 1026 (ICC 0.971). We detected 5 cases of significant stenosis. After endovascular treatment, mean Kt was 79 liters (61; P=.043) and mean TD-Qa was 895mL/min (663; P=.043). Conclusions: TD represents a good indirect method of Qa measurement. In patients with radiocephalic AVFs, Qa measurements in the radial and ulnar artery are more accurate. Therefore, in this situation the TD method obtained an excellent correlation with values taken from the brachial artery.
INTRODUCTION
Studies have shown that patients on haemodialysis programmes with arteriovenous fistulas maintain patency for a longer period of time and incur fewer complications.1 In this context, the various clinical guidelines on vascular accesses (VA) recommend periodical application of different programmes of active follow-up and monitoring.2-4 The main objective of these programmes is the early application of the available range of endovascular and surgical corrective therapies designed to avoid the need for central venous catheters, which imply increased morbidity and mortality rates due to infectious complications.5
Of the available second-generation monitoring methods for measuring VA flow (Qa), those considered as the “gold standard” include the saline-dilution method and colour Doppler ultrasound (UD).6 Despite this, modern haemodialysis monitors utilise other indirect and dilutional techniques for automatically estimating Qa through ionic dialysance7 and thermodilution (TD).8 Our group recently reported a study carried out in 50 stable patients on an ambulatory haemodialysis programme, concluding optimal concordance of Qa derived from the temperature monitor as compared to saline-dilution as a reference value.9
No studies to date have evaluated the concordance of Qa values between TD and DU measurements. One of the primary limitations of the saline-dilution method and ultrasound for measuring Qa is that both techniques lack an external apparatus. In the case of ultrasound control, it is not possible to automatically determine flow during the dialysis session, and this method is also susceptible to possible biases in measurements related to the angle of insonation and variations in vessel diameter.10 Based on the available scientific evidence, controversy persists regarding which is the best location for measuring Qa with ultrasound in patients with an internal arteriovenous fistula (IAVF), especially in radio-cephalic side-to-end anastomoses (SE). In this context, Wiese et al.11 suggested that measurements in the radial artery could underestimate flow due to feedback from the ulnar arterial access and palmar arch.
OBJECTIVES
Primary objective: to analyse the level of concordance of Qa measurements between TD and DU.
Secondary objectives:
MATERIAL AND METHOD
Observational and cross-sectional cohort study involving 64 stable patients (41 males) on a haemodialysis programme with a mean age of 59.9±15.4 years, with 54 IAVF (28 radio-cephalic and 26 brachial) and 10 polytetrafluoroethylene (PTFE) prosthetic grafts (5 brachio-axillary and 5 femoro-femoral). Median time on the dialysis programme was 30.5 months (P25-75: 11.7-92.2 months), using 5008S monitors (Fresenius Medical Care®) with bicarbonate and 1.5 or 1.8m2 polysulfone or helixone high-flux filters using post-dilutional online haemodiafiltration; Qb: 410.3±28.1ml/min; Qd: 534.3±117.1ml/min; Qi: 99.4±17.4ml/min. At the end of each haemodialysis session, we determined dosage through ionic dialysance (Kt).12
As regards causes of renal failure, 15 patients had vascular nephropathy, 13 had diabetic nephropathy, 16 were of an unknown cause, 10 had glomerular diseases, 9 had polycystic kidney disease, and 1 had tubulo-interstitial nephropathy.
Vascular flow rate measurement
Doppler ultrasound
DU was considered as the “gold standard” for measuring Qa. We took the mean value from three consecutive measurements taken one week after taking the TD measurement. The reference ultrasound value was obtained at the brachial artery in IAVF13 (4-5cm from the anastomosis) and at the arterial puncture site for prosthetic grafts. We used the colour Doppler ultrasound modality on the MyLab 25 ultrasound machine (Esaote®) for B-mode and haemodynamic analyses. In order to minimise bias when taking measurements, we adjusted PRF and gain, and measured along the transverse-longitudinal axis of the central part of the vein, with a wide spectral window and an insonation angle >60º. In order to measure Qa, we traced the curve of one cycle, taking reference values for maximum velocity (peak systolic velocity) and minimum velocity. The ultrasound automatically provides mean velocity, the area based on the diameter measurement, and the value of Qa using the following formula:
DU-Qa = ∏ r2 (area) x Vm x 6014
R is the radius of the vessel and Vm is the mean velocity (cm/sec)
In the group of patients with radio-cephalic IAVF and SE anastomoses, we also determined Qa in the radial artery, sum of the radial-ulnar artery, and cephalic vein.
Thermodilution
TD is one of the non-invasive techniques available for the monitoring and follow-up of Qa, using recirculation values obtained using the blood temperature monitor (BTM®) with normal and reversed-position haemodialysis lines.15 This method, first described and validated by Schneditz et al.,8 is easy to apply since the BTM sensor is integrated into modern haemodialysis machines.
The measurement process begins by generating a “temperature bolus” by self-limiting the temperature of the dialysate fluid (-2ºC for 2 minutes). Initially, this thermal decrease is picked up by the venous line temperature sensor and, after mixing with the bloodstream and cardiopulmonary circulation of the patient, returns to the dialyser and is detected by the arterial line sensor. The difference between these two values obtained by the two sensors allows us to quantify the percentage of recirculation. This procedure is carried out with normal and reverse-position dialysis lines.
DU-Qa = Qs x (1-Rx) (1-Rn) / (Rx-Rn),
TD-Qa = Qs x (1-Rx) (1-Rn) / (Rx-Rn),
Qs represents effective blood flow (ml/min), Rn is the rate of recirculation with lines in the normal position (%), and Rx is the rate of recirculation obtained with lines in the reverse position (%).
All measurements taken using TD were obtained during the first 60 minutes of the dialysis sessions, with a minimum 5cm distance between puncture sites using a high-efficacy modality of haemodialysis with a Qb of 300ml/min and Qd of 500ml/min.
Statistical analysis
The values obtained were expressed in percentages or mean ± standard deviation. We used the Bland-Altman method16 and intra-class correlation coefficients (ICC) to analyse concordance between the two measurement methods. We used the non-parametric Mann-Whitney U-test to compare differences between quantitative variables. We considered a P-value of <.05 to be statistically significant in all cases. We used PASW statistical software, version 18, for all statistical analyses (SPSS Inc., Chicago, IL, USA).
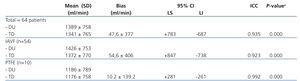
The mean Qa value obtained using DU was 1389±758ml/min. The DU-Qa value resulted in 1426±753ml/min for the group of patients with IAVF, and 1186±789ml/min in the PTFE group. Table 1 summarises the results in terms of concordance between TD and DU, and Figure 1 presents a graphical representation of the Bland-Altman mathematical model. The measurement bias between the two methods was defined as the difference in Qa values obtained between TD and DU. Figure 2 summarises the number of patients with IAVF or PTFE divided into categories based on the Qa values obtained from both methods using the current clinical VA guideline recommendations for cut-off values. DU measurements classified 92.2% of patients with IAVF as having a Qa≥500ml/min, and 7.8% as having a Qa<500ml/min. The results from TD were 90.6% and 9.4%, respectively. As regards the group of patients with PTFE prostheses, DU classified 70% as having a Qa≥600ml/min and 30% as having a Qa <600ml/min. The results obtained for Qa using TD in this group were 60% and 40%, respectively.
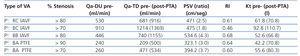
In the group of 28 patients with radio-cephalic IAVF with SE anastomoses, the mean Qa value obtained using ultrasound measurements in the brachial artery was 1232±767ml/min. The measurements taken from the radial artery with respect to the brachial artery resulted in a mean value of 942±595ml/min, with a mean bias of -290ml/min and an ICC of 0.805 (P<.01). The sum value of the radial and ulnar arteries for Qa was 1103±583ml/min, with a bias of -129ml/min and an ICC of 0.973 (P<.01). The mean value taken from the cephalic vein was 788±423ml/min, with a bias of -44ml/min and an ICC of 0.772 (P<.01). The results obtained using TD were 1026±431ml/min, with a bias of -206ml/min and an ICC of 0.971 (P<.01). Using the Qa value obtained from the brachial artery as a reference point, the radial artery corresponded to 76.5%, the sum radial-ulnar artery was at 89.5%, the cephalic vein at 63.9%, and the TD method yielded a value at 83.3% of the reference point.
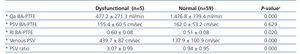
In our morphological and haemodynamic analysis of the study group, we detected 5 cases of significant VA dysfunction (3 IAVF and 2 PTFE). Table 2 and Figure 3 summarise the primary characteristics of this group of patients, as well as values for haemodialysis dosage (Kt) and Qa measured using TD post-revascularisation with percutaneous transluminal angioplasty (PTA). The post-PTA Kt value was 79l (61l in the pre-PTA measurement; P=.043), and the post-PTA Qa-TD was 895ml/min (663ml/min pre-PTA measurement; P=.043). Table 3 summarises the values obtained for the haemodynamic parameters using ultrasound control in patients with significant VA dysfunction and the rest of the group.
DISCUSSION
According to our results, TD is a useful automated and non-invasive method for measuring Qa, as compared to DU. The major clinical guidelines for VA recommend the active application of various multi-disciplinary programmes in order to facilitate early detection of significant vascular dysfunction.2-4 The main objective of these strategies is to promote optimal functioning of endovascular and surgical treatment measures with the goal of maintaining access patency and minimising the risk of thrombosis. Despite using second-generation Qa measurement methods, we must never forget the importance of a systematic physical examination. In the study by Asif et. al,17 involving 145 consecutive patients with dysfunctional IAVF, exploring the VA allowed for detecting and localising the stenosis in a high percentage of cases.
Qa estimation represents one of the most important predictive factors of significant dysfunction (stenosis or partial thrombosis). The criteria used for imaging tests include a reduction in absolute Qa values of <600ml/min in PTFE grafts or <500ml/min in IAVF.18,19 A temporary reduction of Qa>20%-25% with respect to baseline values must also be included among the criteria associated with high clinical suspicion. As shown in the study by Tessitore et al.,20 which involved a 5-year follow-up of 159 patients on haemodialysis with IAVF (62 monitored using the saline-dilution method), monitoring Qa was associated with an increase in the rate of detection of stenoses, reduced rates of thrombosis and central venous catheter placement, a greater economic benefit, and superior patency values during the first three years of follow-up after implantation of the vascular access point.
Currently, we can automatically obtain Qa estimates at no additional economic cost using techniques based on TD. In the study reported by Wang et al.,21 this dilutional method resulted in a sensitivity value of 81.8% and a specificity of 98.6% for detecting dysfunctional IAVF. According to the results reported by our research group, TD yields a strong correlation with the saline-dilution method in an intra-method validation test (Qb: 300ml/min; Qd: 500ml/min).9 Despite this, TD methods have certain limitations in measuring Qa with standard prescription parameters in high-flux haemodialysis and post-dilutional online haemodiafiltration.22 The mean Qa values obtained by TD in recent publications that included patients with IAVF were 1034ml/min and 1170ml/min, with no significant differences as compared to the saline-dilution and Delta-H methods, respectively.23,24 As shown in Table 1 and Figure 1, our results show that TD also presents a strong correlation with Qa values taken using ultrasound techniques, with an ICC>0.90 and a bias of 54.6ml/min and 10.2ml/min in patients with IAVF and prosthetic PTFE grafts. However, the confidence intervals (Table 1) and Bland-Altman graphical representation (Figure 1) show a greater degree of dispersion of values for Qa>1000ml/min. This phenomenon was also described in the study by Merino et al.25 when comparing ionic dialysance with the saline-dilution method. In these clinical situations, we believe that a significant reduction in baseline Qa values is more valuable as a screening method for patients that should undergo imaging tests in order to facilitate the early detection of significant VA dysfunction.
According to our results for the group of patients with radio-cephalic IAVF and SE anastomoses, values taken from the sum of the ulnar and radial arteries presented the greatest level of concordance with respect to reference Qa values taken from the brachial artery. The mean bias obtained was -129ml/min, 89.5% of the total brachial flow. Even so, measuring these values in practice may lead to bias, since this involves ultrasound evaluation of small-diameter arterial vessels. In this context, it would be interesting to apply TD as an automated indirect method with strong correlation to values taken from the brachial artery. Measurements taken from the efferent vein also are associated with errors related to variations in diameter, turbulence, and vibrations.11
DU represents a second-generation method that allows us to monitor VA through measurements of Qa, but also facilitates the assessment of other morphological and haemodynamic parameters. The morphological criteria that suggest the presence of a stenosis include a B-mode vascular reduction >50% accompanied by turbulent flow (aliasing) in the colour Doppler modality. Functional criteria include an elevation in peak systolic velocity or maximum velocity >400cm/sec (PSV), a PSV ratio between the stenotic and pre-stenotic areas >2 for IAVF or >3 for PTFE, an elevation in the brachial artery resistance index >0.6, or the aforementioned alterations in Qa values.11,26 As summarised in Table 3 and Figure 3, patients in our study with significant VA stenosis presented these haemodynamic abnormalities, as well as receiving a lower dose of haemodialysis (Kt). After endovascular revascularisation using an angioplasty balloon catheter, we observed a recovery of Qa as measured by TD (895ml/min vs 663ml/min; P=.043) and Kt (79l vs 61l; P=.043). The diagnostic sensitivity of DU for the diagnosis of significant stenoses ranges between 80% and 90%.27-29 Various studies have shown a greater rate of survival, fewer hospitalisations, and a significant reduction in health costs for patients under active monitoring with ultrasound techniques.30,31
One limitation of our study was the fact that we did not evaluate the impact of TD as a prospective monitoring programme for VA. As such, we find it necessary to design future studies focused on evaluating the efficacy of methods based on TD as a useful tool for the early detection of vascular dysfunction and for reducing thrombosis rates.
To conclude, TD is a useful automated indirect method for measuring Qa, with comparable results to those produced using DU. In patients with radio-cephalic IAVF and SE anastomoses, the most precise measurements were those derived from the sum of radial and ulnar arterial flow rates. However, in this clinical situation, TD produces excellent correlation with reference values taken from the humeral artery.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. General concordance results between vascular flow measurements obtained using thermodilution and Doppler ultrasound
Table 2. General characteristics of patients with significant vascular access dysfunction
Table 3. Comparative analysis of the different haemodynamic parameters obtained using Doppler ultrasound (pre-PTA) between cases with dysfunction and all other patients
Figure 1. Graphical representation using the Bland-Altman method for comparing measurements of vascular flow using Doppler ultrasound and thermodilution
Figure 2. Patient classification based on type of vascular access and vascular flow rate as measured using Doppler ultrasound and thermodilution
Figure 3. Progression of haemodialysis doses (Kt) and vascular flow rates determined using pre- and post-PTA TD with a balloon catheter in patients with significant vascular access dysfunction.