Nearly 50% of the children with steroid sensitive nephrotic syndrome (SSNS) have a frequently relapsing (FR) or steroid dependent (SD) course, experiencing steroid toxicities and complications of immunosuppression. The study aimed to compare parameters between children with infrequent relapsing (IFR) and FR/SD nephrotic syndrome and to identify the factors associated with a FR/SD course.
MethodsA retrospective analysis of medical records from 2009 to 2014, of children with SSNS attending the pediatric nephrology clinic in a tertiary care medical college and hospital.
ResultsOut of 325 children (226 males) with SSNS, 213 were IFR and 112 were FRNS/SDNS. The median age of onset was 34 (IQR 24–48) months. The median time to the first relapse was 4 (IQR 3–7) months and 6 (IQR 4–12) months in FR/SD and IFR group respectively. Multivariate logistic regression analysis showed “adequate treatment (≥12 weeks) of the first episode” (odds ratio 0.56, 95% CI 0.34–0.91; p value=0.02) and “shorter median time to the first relapse” (odds ratio 1.04, 95% CI=1.01–1.08; p value=0.04) to be independent predictors of FR/SD course.
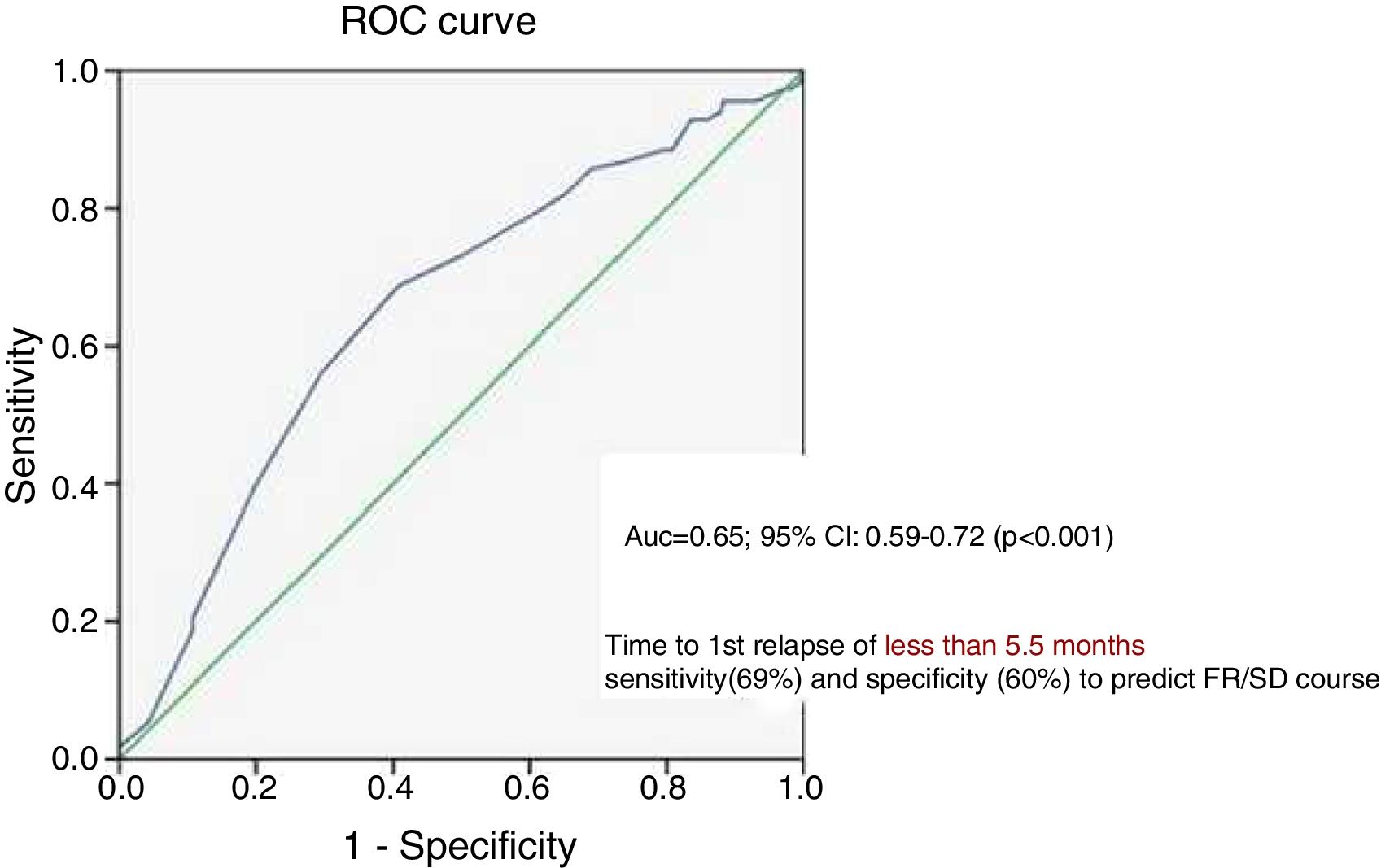
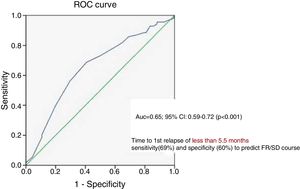
An ROC curve was constructed which showed that time to first relapse <5.5 months was associated with a sensitivity of 69% and specificity of 60% in predicting a FR/SD course.
ConclusionAdequate treatment of the first episode is associated with less chance of an FR/SD course. After treatment of first episode, the first relapse occurring within 5.5 months may predict a frequently relapsing or steroid dependent course.
Casi el 50% de los niños con síndrome nefrótico sensible a esteroides (SNSE) presentan un curso frecuentemente recurrente (FR) o dependiente de esteroides (DE) y padecen toxicidades por esteroides y complicaciones por la inmunodepresión. El estudio tuvo como objetivo comparar los parámetros entre los niños con recurrencias infrecuentes (RI) y el síndrome nefrótico FR/DE, e identificar los factores asociados con un curso FR/DE.
MétodosUn análisis retrospectivo de las historias clínicas de 2009-2014 de los niños con SNSE que asisten a la clínica de nefrología pediátrica en una facultad de medicina y un hospital de atención especializada.
ResultadosDe 325 niños (226 varones) con SNSE, 213 fueron RI y 112 fueron SNFR/SNDE. La mediana de edad de inicio fue 34 (RIC: 24-48) meses. El tiempo medio hasta la primera recaída fue 4 (RIC: 3-7) meses y 6 (RIC: 4-12) meses en los grupos FR/DE e RI, respectivamente. El análisis de regresión logística multivariante mostró «tratamiento adecuado (≥ 12 semanas) del primer episodio» (razón de posibilidades: 0,56; IC del 95%: 0,34-0,91; valor p=0,02) y «tiempo medio más corto hasta la primera recaída» (razón de posibilidades: 1,04; IC del 95%: 1,01-1,08; valor p=0,04) para ser factores predisponentes independientes del curso FR/DE.
Se construyó una curva ROC que mostró que el tiempo hasta la primera recaída < 5,5 meses se asoció con una sensibilidad del 69% y una especificidad del 60% en la predicción de un curso FR/DE.
ConclusiónEl tratamiento adecuado del primer episodio se asocia con menos posibilidades de un curso FR/DE. Después del tratamiento del primer episodio, la primera recaída que ocurre dentro de los 5,5 meses puede pronosticar un curso frecuentemente recurrente o dependiente de esteroides.
Children with idiopathic steroid sensitive nephrotic syndrome (SSNS) constitute a major proportion of patients attending a pediatric nephrology clinic. Despite the fact that SSNS has a favorable renal prognosis in most patients, 60–90% of them tend to relapse and 40–50% has a frequently relapsing (FRNS) or steroid dependent (SDNS) course.1–3 Children with FRNS or SDNS experience the morbidities of steroid toxicity including cushingoid features, hypertension, hyperlipidemia, hyperglycemia, serious infections, growth retardation, stunted growth associated with active disease and treatment, and osteopenia among morbidities and steroid adverse events. They are also subjected to other immunosuppressive agents and have an overall poor quality of life.4 Identifying at the very outset or early in the follow up, which SSNS children would have a FR/SDNS course is the Achilles heel of any pediatric nephrologist.
Earlier, many authors did try to identify factors which could predict a FR/SDNS course of nephrotic syndrome. However, most of the studies were retrospective and involved small sample of patients varying from 35 to a maximum of 150.6–10
Ours is a tertiary care center with a large follow-up of patients in the nephrology clinic. So we aimed to study their demographic parameters, disease pattern and treatment detail and also assessed the determinants studied by other authors as predictors of a subsequent FR/SD course.
MethodologyA retrospective analysis of the medical records of children with SSNS, attending the pediatric nephrology clinic of a tertiary care medical college, from 2009 to 2014, was done. Children between 6 months to 18 years of age, who had a diagnosis of SSNS till their last follow up and were having relapses, were eligible for the study, excluding those with incomplete medical records, a follow-up less than 6 months, non-compliance to treatment and secondary causes of nephrotic syndrome. Details regarding demographic parameters, disease course and treatment were obtained. The subjects were grouped in to 2 categories: infrequently relapsing nephrotic syndrome (IFRNS) and FRNS/SDNS. As per Indian Society of Pediatric Nephrology (ISPN) guidelines, FRNS was defined as the occurrence of ≥2 relapses in the initial 6 months or ≥3 relapses in any 12 months; SDNS was defined as the presence of two consecutive relapses while on tapering doses of prednisolone or within 14 days of cessation of steroid therapy. The children with nephrotic syndrome were treated in our hospital as per ISPN treatment protocols.11 An adequate treatment of the first episode was considered as oral prednisolone 2mg/kg/day for 6 weeks, followed by 1.5mg/kg on alternate days for a minimum of 6 weeks.11
Demographic, treatment and disease parameters were compared between the 2 groups of subjects. Shapiro-Wilki test was used to check for normality. In case of non-Gaussian distribution, median with inter-quartile range was calculated and Mann–Whitney U test was used to compare medians. Categorical variables were compared by Chi-square tests. Univariable and multivariable logistic regression were used to assess the role of possible risk factors (gender, age of onset, time to first relapse, adequate treatment of first episode, occurrence of serious complications requiring hospitalization during the course of disease) in predicting an FR/SD course. In case of multivariable analysis, Hosmer and Lameshow Goodness of fit test was used to assess model fit. The sensitivity and specificity was calculated for the factor which was found to independently predict a frequently relapsing or steroid dependent course. A Receiver Operating Characteristic (ROC) curve was also constructed to evaluate the performance of the predictive factor. All analyses were done by SPSS version 20 and significance was taken at a p-value of 0.05 with 95% confidence interval.
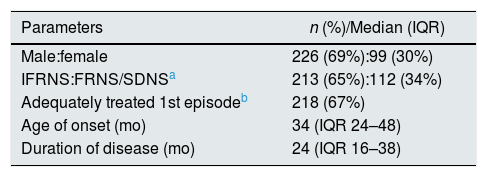
ResultsRecords of a total of 325 children (male:female – 2.3:1) with SSNS, fulfilling the inclusion criteria were analyzed. The median age of onset was 34 (IQR 24–48) months. Children having FRNS or SDNS course together constituted 35% while those having an IFRNS course were 65%. The median duration of follow-up was 24 (IQR 16–38) months. The demographic parameters and disease details are shown in Table 1.
Demographic parameters and disease characteristics of children with steroid sensitive nephrotic syndrome.
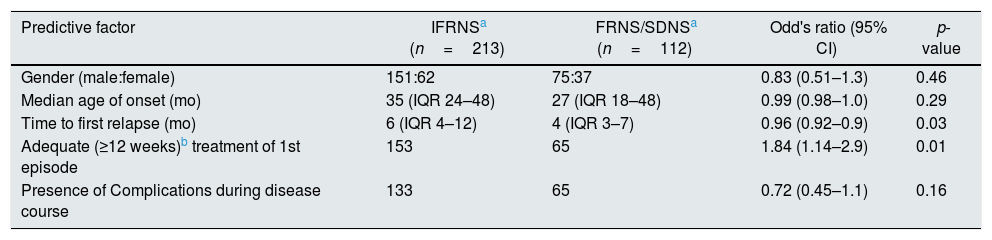
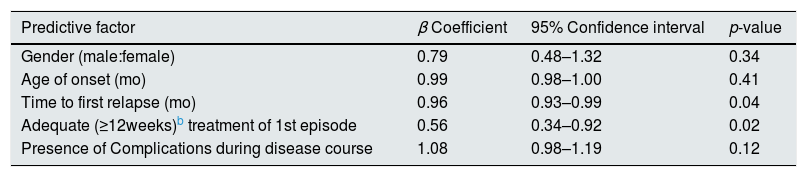
Possible factors like gender, age of onset, time to first relapse, adequate (≥ 12 weeks) treatment of first episode, occurrence of serious complications requiring hospitalization during the course of disease, were compared between IFRNS and FRNS/SDNS groups by both univariable (Table 2) and multivariable analyses (Table 3). It was found that inadequate treatment of the first episode of nephrotic syndrome for a period less than 12 weeks was associated with 1.8 (95% CI 1.1–2.9) fold risk of a frequently relapsing or steroid dependent course. Also, after treatment of the initial episode, the shorter the time to first relapse, the more were the chances of having a subsequent FR/SD course.
Univariable analysis to assess possible predictors of FR/SD course in children with steroid sensitive nephrotic syndrome.
| Predictive factor | IFRNSa (n=213) | FRNS/SDNSa (n=112) | Odd's ratio (95% CI) | p-value |
|---|---|---|---|---|
| Gender (male:female) | 151:62 | 75:37 | 0.83 (0.51–1.3) | 0.46 |
| Median age of onset (mo) | 35 (IQR 24–48) | 27 (IQR 18–48) | 0.99 (0.98–1.0) | 0.29 |
| Time to first relapse (mo) | 6 (IQR 4–12) | 4 (IQR 3–7) | 0.96 (0.92–0.9) | 0.03 |
| Adequate (≥12 weeks)b treatment of 1st episode | 153 | 65 | 1.84 (1.14–2.9) | 0.01 |
| Presence of Complications during disease course | 133 | 65 | 0.72 (0.45–1.1) | 0.16 |
Multivariable analysis to assess possible predictors of FR/SDa course in children with steroid sensitive nephrotic syndrome.
| Predictive factor | β Coefficient | 95% Confidence interval | p-value |
|---|---|---|---|
| Gender (male:female) | 0.79 | 0.48–1.32 | 0.34 |
| Age of onset (mo) | 0.99 | 0.98–1.00 | 0.41 |
| Time to first relapse (mo) | 0.96 | 0.93–0.99 | 0.04 |
| Adequate (≥12weeks)b treatment of 1st episode | 0.56 | 0.34–0.92 | 0.02 |
| Presence of Complications during disease course | 1.08 | 0.98–1.19 | 0.12 |
Hosmer and Lameshow Goodness of fit – 0.37.
An ROC curve was constructed to assess the predictive performance of “time to first relapse” which showed an AUC of 0.65 (95% CI 0.6–0.72) (p<0.001) (Fig. 1). Further, it was seen that “time to first relapse” less than 5.5 months was associated with a sensitivity of 69% and specificity of 60% in predicting a frequently relapsing or steroid dependent course.
DiscussionPediatric nephrologists are at a loss to identify, risk stratify and prognosticate parents of children with SSNS at the very outset. This issue has been researched by many authors, mostly by retrospective analysis of small sample of patients.6–10 Moreover, there is lack of uniformity in identifying risk factors among the different studies. In our study, we have analyzed relatively large numbers of children with SSNS from a single tertiary care center.
As in most studies, males constituted more than twice the number of female children (2.3:1).5–7,12,13 The median age of onset of nephrotic syndrome was 34 (24–48) months similar to that reported by Yap et al. and Constantinescu et al. though other authors have reported higher ages of onset of around 4.5 to 5 years.5,6,8,9,14 Compared to the data of other authors, we had a larger proportion of infrequent relapsers (213/315, amounting to 65%) compared to frequent relapsers/steroid dependent children.5,9,14 However, statistics from another center in India showed even higher fraction of IFRNS (89% of all relapsing children). The higher numbers of FR/SD in other centers could be due to a referral bias of difficult cases. Also, we have included children with a minimum follow-up of 6 months, a time relatively insufficient to develop in to a FR/SD pattern. Nevertheless, the subjects in our study had a median duration of follow-up of 24 (IQR 16–38) months, justifying the comparison in the two groups.
Among the risk factors compared between the two categories of relapsing nephrotic syndrome, it was found that adequate treatment [60mg/m2/d or 2mg/kg/d daily oral prednisone for 4–6 weeks followed by alternate-day medication as a single alternate day dose at 40mg/m2 or 1.5mg/kg; total duration of corticosteroid therapy of at least 12 weeks] had a significant protective effect against a frequently relapsing/steroid dependent course, reducing the chances of the latter to about 56%. Sinha et al. also found a modest reduction in the risk of frequent relapses by 30% with an initial treatment of ≥12 weeks. On the other hand, a recent study by Ali et al. on 80 children could not show any effect of the duration of treatment of first episode on future disease pattern. Earlier studies had over-estimated the effect of prolonged treatment (beyond 8–12 weeks) of the first episode of nephrotic syndrome, showing a lower risk of subsequent relapses with extension of treatment up to 7 months.7,15 However, more recent studies with lower rates of bias have demonstrated no benefit of prolonging therapy beyond 12 weeks.14,16 Our analysis further endorses the fact that, less than optimal treatment of 12 weeks, during the first episode, results in subsequent frequent relapses.
Time to the first relapse, after treatment of the first episode, was found to be another disease characteristic having an independent effect on future course. Our study showed that the first relapse occurring within a period of 5.5 months had a sensitivity of nearly 70% to predict a FR/SD course of nephrotic syndrome. Noer et al. had also found an increased possibility of FR course, when the interval between first steroid response and first relapse was <3 months.17 While some authors have conclusions parallel to our study, others have not analyzed this parameter.9,14,18 A younger age of onset has been shown by some authors as a pointer toward an FR/SD course.7,14 Contrary to these reports, our study, as well the prospective study from Australia did not find a relation between age of onset and the relapsing pattern of the disease.18 Unlike a couple of studies, in most others, including ours, gender had no bearing on future course of children with nephrotic syndrome.5,7,9,14,18 Longer time to achieve remission after the onset of nephrotic syndrome is an additional variable which has been shown by some authors to be a significant risk factor for a FR/SD course.5,6,18,19 Considering the retrospective nature of our study, it was difficult to obtain the exact value of this parameter uniformly across such large numbers of patients, thereby rendering us incapable of analysing it. Different authors have had conflicting views on hematuria being a risk factor for FR/SD course and our study does not deal with this variable.
ConclusionAfter having analyzed a large sample of children with SSNS, we identified two key factors-‘adequate treatment of first episode for at least 12 weeks’ and ‘time to first relapse’ which can independently predict a FRNS/SDNS course. This large study from a single center in the Indian subcontinent will clearly be generalizable to the population with SSNS and help in focusing on few pertinent risk factors for prognostication, close monitoring and future research.
Conflicts of interestThe authors have no conflicts of interest to declare.