Background and aims: Contrast-induced nephropathy (CIN) has a growing incidence in which renal vasoconstriction and medullary hypoxia are important mechanisms. Therapeutic approaches are very restricted and there is a considerable interest in advancing preventive strategies. Adrenomedullin is a relatively novel peptide having antioxidant, vasoactive and vasodilatory properties. We aimed to investigate whether adrenomedullin might have a preventive role against the development of experimental CIN. Methods: Wistar albino rats (n=24) were allocated randomly into four equal groups of 6 each; Control (C), Adrenomedullin (A), Contrast Media (CM) and Adrenomedullin plus Contrast Media (ACM). All rats were deprived of water from day 1 to day 4 during 72 hours. Then, intravenous administrations of chemicals were performed. Adrenomedullin was given at dose of 12µg/kg to groups A and ACM. A single dose of high-osmolar contrast media; diatrizoate (Urografin 76%, Schering AG, Germany) was injected to groups CM and ACM at dose of 10mL/kg. On day 1 and 6 blood samples were drawn for renal function tests and inflammatory markers including TNF-α IL-1β, IL-6 and IL-18. After sacrification, kidney histologies were examined with hematoxylin-eosin staining. Results: Compared to CM group, serum cystatin-C levels on 6th day were found significantly lower in ACM group (p<0.05). Additionally, daily protein excretion rates, absolute changes in daily urine output and creatinine clearance values were significantly lower in ACM group than those in CM group (p<0.05). In histopathological evaluation, regarding the degree of tubular damage and medullary congestion scores, ACM group had slightly better scores compared to CM group; however the differences did not reach significance as shown in inflammatory markers. Conclusion: This study demonstrated a beneficial impact of adrenomedullin on deteriorated renal function tests in an experimental CIN model. Adrenomedullin might be a candidate agent for prophylaxis of CIN. However, further studies are needed to shed more light on this issue.
Antecedentes y objetivos: La incidencia de la nefropatía inducida por contraste (NIC) está aumentando y la vasoconstricción renal y la hipoxia medular son mecanismos importantes. Los enfoques terapéuticos son muy limitados y existe un gran interés en avanzar en las estrategias preventivas. La adrenomedulina es un péptido relativamente nuevo con propiedades antioxidantes, vasoactivas y vasodilatadoras. Nuestro objetivo es investigar si la adrenomedulina puede jugar un papel preventivo frente al desarrollo de la NIC experimental. Métodos: Se distribuyeron ratas Wistar albinas (n = 24) de forma aleatoria en cuatro grupos de 6: control (C), adrenomedulina (A), medio de contraste (MC) y adrenomedulina más medio de contraste (AMC). Las ratas no ingirieron agua desde el día 1 al día 4 (durante 72 horas). Posteriormente, se les administraron las sustancias de forma intravenosa. Los grupos A y AMC recibieron una dosis de adrenomedulina de 12 µg/kg. Los grupos MC y AMC recibieron una única dosis de medio de contraste de alta osmolaridad: 10 ml/kg de diatrizoato (Urografin 76 %, Schering AG, Alemania). Los días 1 y 6 se tomaron muestras de sangre para realizar análisis de función renal y de marcadores inflamatorios, incluidos el TNF-α, IL-1β, IL-6 e IL-18. Tras el sacrificio, se examinaron las histologías renales con tinción hematoxilina-eosina. Resultados: En comparación con el grupo MC, los niveles de cistatina C sérica fueron significativamente inferiores en el grupo AMC (P < 0,05). Además, la tasa de excreción diaria de proteínas, los cambios absolutos en el gasto urinario diario y los valores de aclaramiento de la creatinina fueron significativamente inferiores en el grupo AMC que en el grupo MC (P < 0,05). En la evaluación histopatológica, en lo que respecta al grado de daño tubular y los valores de congestión medular, el grupo AMC presentaba niveles ligeramente mejores en comparación con el grupo MC. Sin embargo, según los marcadores inflamatorios, las diferencias no presentaron significación estadística. Conclusión: El estudio ha demostrado que la adrenomedulina resulta beneficiosa en los análisis de función renal deteriorada en un modelo experimental de NIC. Por lo tanto, la adrenomedulina puede ser un candidato para la profilaxis de la NIC. No obstante, se necesitan más estudios que arrojen luz sobre este tema.
INTRODUCTION
Contrast-induced nephropathy (CIN) is a complex form of acute kidney injury (AKI) that is defined as an acute reduction in renal functions secondary to iodinated contrast media administration. In today’s clinical practice, radiological procedures requiring intravascular administration of iodinated contrast media are increasingly being used for diagnostic and therapeutic purposes. On the other hand, by virtue of increment in aging populations, the incidences of arterial hypertension, diabetes mellitus and coronary artery diseases have been persistently growing up, leading also an increase in potential candidates for such kinds of radiological procedures.1 It should be noted that CIN is responsible for most of the hospital-acquired AKI cases2 and associated with increased health care costs, prolonged hospital stays3 and increased mortality rates at the present time.3,4 In future, CIN definitely seems to be a greater problem.
The proposed pathophysiologic mechanisms for CIN are outer-medullary hypoxia due to decreased renal blood flow resulting from renal artery vasoconstriction, tubular obstruction as well as direct tubular toxicity,5 decreased nitric oxide production and increased oxidative stress.6,7 Nevertheless, it still remains to be a poorly understood phenomenon and there is a considerable interest for preventive strategies some of which have been suggested in subjects with preexisting renal dysfunction.8 However, beside extracellular volume expansion, a generally accepted and precise preventive strategy has not been proven up till now.
Adrenomedullin, a 52-amino acid peptide with structural homology to calcitonin gene-related peptide was isolated from a human pheochromocytoma in 1993.9 Since then, its potent immunomodulatory, antioxidant, vasoactive and vasodilatory properties have been shown in different studies.10-12 Of note, its considerable roles in systemic and local circulation, regulation of cardiovascular system and other hormonal secretions have also been discovered.13 In setting of rat models, it was shown that adrenomedullin attenuated the renal ischemia/reperfusion injury14 and improved survival in case of hemorrhagic shock and gut ischemia/reperfusion injury.15,16 However, its probable preventive effect has never been searched in a CIN rat model.
In the presented study, using a rat model, we tested preventive effects of adrenomedullin mainly through its vasodilatory and anti-inflammatory properties against the development of CIN.
MATERIALS AND METHODS
Animals
The study included 24 female Wistar albino rats (6 weeks old with a mean weight of 205.0±12.9 gram) obtained from the Animal Care and Research Center of Gazi University. During 24-hour urine accumulation periods (on days 1 and 6), rats were kept individually in metabolic cages. During other processes, they were kept in polycarbonate cages. Rats were housed at a temperature of 22-25°C, humidity of 40-70%, with 12 hour light and dark cycles. Drug administrations, blood samplings and daily weighing procedures were performed between 9:00 and 10:00 a.m. to minimize circadian variation. The study was approved by the Experimental Animals Ethics Committee of Gazi University.
Experimental design and drugs
The study design for CIN induction was constituted by preliminary evaluations on three rats. We attained anuria and approximately 15% weight loss by prolonged water deprivation to 72 hours. Histopathologically, tubular necrosis and medullary congestions appeared after injection of a relatively high dose diatrizoate (10mL/kg) following water deprivation. Therefore, in the presented study we planned to implement 10mL/kg dosage of diatrizoate following 72-hour water deprivation period for CIN induction.
Rats (n=24) were allocated randomly into four equal groups of 6 each; Control (C), Adrenomedullin (A), Contrast Media (CM), and Adrenomedullin plus Contrast Media (ACM). All rats were deprived of water from day 1 to day 4 during 72 hours but allowed free to access to standard rat chow. Contrast-induced nephropathy was induced by a single intravenous administration of high-osmolar contrast media diatrizoate (Urografin 76%, Schering AG, Germany) at dose of 10mL per kg (approximately 2mL), into the tail vein under ether anesthesia. Diatrizoate was administered to groups CM and ACM. Adrenomedullin was also administered by intravenous route into the tail vein at dose of 12µg per kg to groups A and ACM. Adrenomedullin dosage was determined based on a recent trial’s methodology, which has studied the effect of adrenomedullin on renal ischemia and reperfusion injury in a rat model.14 Similar with the volume of other injections, adrenomedullin was administered in 2mL of 0.9% saline. In ACM group, adrenomedullin and contrast media injections were performed consecutively. Only 2mL of 0.9% saline was injected to group C. All injections were performed on the fourth day, after 72 hours of dehydration period.
Biochemical analysis, renal function assessment and measurement of inflammatory parameters
Baseline blood samples were drawn from the tail vein on day one under ether anesthesia while the final blood samples were withdrawn from the abdominal aorta at the end of the study (day 6). On day 1, samples were obtained for serum blood urea nitrogen (BUN) and creatinine (Cr) which were used as indicators of renal functions. Additionally, on the same day samples were obtained for also plasma sodium (Na), urine Cr and Na which were used for calculations of creatinine clearance (CrCl) and fractional Na excretion rates (FENa). Creatinine clearance was calculated using the U×V/P formula (U, urine Cr mg/dl; V, urine volume mL/min per 100g; P plasma Cr mg/dL) and was expressed as mL/min/100g. Fractional Na excretion was calculated as (urine Na / plasma Na) × (plasma Cr / urine Cr) × 100. Serum and urine Cr were evaluated by the Jaffe method and BUN was measured by a kinetic ultraviolet assay method in an autoanalyzer. Plasma and urine Na were measured in an autoanalyzer.
On day 6, blood samples were withdrawn for measurements of cystatin-C, tumor necrosis factor-alpha (TNF-α), interleukin-1 beta (IL-1β), interleukin-6 (IL-6) and interleukin-18 (IL-18). Chemicals and kits were from Sigma–Aldrich and Sigma Diagnostic (St. Louis, MO, USA). For the evaluation of Cystatin-C Biovendor rat Elisa kit (Catalogue number: RD391009200R, for TNF-α and IL-1β Invitrogen rat Elisa kits (Catalogue number: KRC3011and KRC 0011), for IL-6 eBioscience Platinum rat Elisa kit (Catalogue number: BMS625) and for IL-18 Cusabio rat Elisa kit (Catalogue number: CSB-E04610r) were used. Cystatin-C and IL-18 values were given as ‘ng/mL’ and others were given as ‘pg/mL’.
Histopathological analysis of kidneys
On day 6, kidneys were excised by the application of general anesthesia via intraperitoneal xylazine (Rompun Flakon, 5mg/kg, Bayer, Istanbul, Turkey) and ketamine (Ketalar Flakon, 45mg/kg, Pfizer, Istanbul, Turkey). After adding 10% formalin, the right kidneys were preserved for histopathological evaluation. Right renal tissues taken for histopathological evaluation were cut longitudinally from the top pole to the bottom pole, and placed in 10% neutral formalin for 72h. Samples were processed with routine histological procedures and 4-5µ thick sections were cut from the paraffin blocks obtained from the tissue. Sections were stained with hematoxylin-eosin and analyzed using a Leica DM 4000 B microscope. During the evaluation of tissue damage, vacuolization, degeneration, necrotic differences in renal proximal and distal tubules, and congestion in interstitial spaces were semi-quantitatively scored by an assessment in randomly selected areas. According to this assessment:
Statistical analysis
All statistical analyses were carried out using SPSS for Windows, Version 18.0 (Chicago, USA). For the presentation of measurable continuous quantitative variables; mean and standard deviation or median and interquartile range (IQR) were used depending on the distribution of variables. Frequencies and percentages were used for categorical data. For comparison between groups more than two, analysis of variance (ANOVA) was applied, and for the post-hoc study, the Bonferroni test was used. We also assessed the significance of the differences between baseline and 6th day values by using paired samples t test. p<0.05 was accepted as the significance limit.
RESULTS
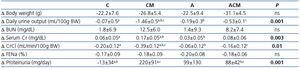
We have not experienced any loss of rats during the study. The study groups were similar in terms of baseline body weight and renal function parameters, but only baseline proteinuria levels were slightly significant between the study groups. After three days of dehydration period, all rats lost approximately 10-15% of their baseline body weight and the differences were significant (p<0.01) for all groups (Table 1).
Renal function parameters
Compared to baseline values, daily urine volumes have significantly decreased in CM and ACM groups on the 6th day (p: 0.001 for both). Serum BUN and Cr levels have increased and CrCl levels have decreased significantly (p<0.05 for all three groups) in all groups except group A. On day 6, FENa showed a significant decrease in all study groups (p<0.005 for all groups). Baseline and day 6 daily urine volumes, serum Cr, BUN, CrCl, FENa and proteinuria levels were shown in Table 1.
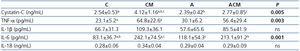
The differences in renal function parameters and body weights were calculated by subtracting the baseline values from the 6th day values. These delta (¿) values were also compared among the groups (Table 2). The absolute change value of serum Cr was found to be the highest in CM group. Absolute changes of daily urine output and CrCl in ACM group were significantly lower than those in CM group (p<0.05) (see Figure 1). Besides, proteinuria increased significantly in CM group compared with ACM group (p<0.05). Additionally, serum cystatin-C levels on day 6 were significantly lower in ACM group compared with CM group (p<0.05) (Table 3).
Inflammatory parameters
Among four inflammatory markers, all were found to be highest in CM group but only serum TNF-α and IL-6 (p: 0.001) levels were significantly different between the groups. The differences in serum TNF-α and IL-6 levels were significant between C and CM groups. However, the difference between the groups CM and ACM were not statistically significant in subgroup analysis (Table 3). Serum IL-1β and IL-18 levels seemed to be slightly elevated in CM group, but the difference did not reach statistical significance.
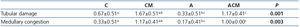
Histopathological findings
Compared to control group, in CM group, there were significant vacuolization, degeneration and necrotic areas in the tubules and congestion in the corticomedullary region. Compared with control rats, the mean scores for the degree of tubular damage and medullary congestion were significantly higher in the CM group (p<0.05). In the CM group, there were significant vacuolization, degeneration and necrotic areas in the proximal and distal tubules. There was also significant congestion in the corticomedullary region in the same group. Although, the ACM group had slightly better histopathological scores compared with the CM group, there were no statistically significant differences with regard to both histopathological parameters. Scores of histological findings of the groups were shown in Table 4.
DISCUSSION
In the presented study, a potential preventive effect of adrenomedullin in the development of CIN has been sought in a rat model. Administration of adrenomedullin immediately before injection of contrast media has let to significantly lower serum cystatin-C levels, urinary protein as well as lower absolute changes in CrCl and daily urine output compared to solely contrast media administration. Hence, it has been suggested that this molecule attenuated the acute deterioration of renal functions arising from intravenous injection of contrast media. As far as our knowledge, this study, for the first time, is showing in vivo efficacy of adrenomedullin to prevent the development of experimental CIN in a rat model.
Studies regarding the CIN pathophysiology suggested that, it is most likely due to decreased renal blood flow resulting from renal ischemia and direct toxicity to tubular epithelial cells.17,18 Adrenomedullin has receptors in glomeruli and distal nephrons19 and of note, it has been shown that intravenous infusion of this substance increases renal blood flow, glomerular filtration rate and consequently urine output through renal vasodilatation mechanisms.20,21 In a diabetic rat model, the local action of adrenomedullin has been shown as increased,19 reinforcing its contribution to dilatation of the glomerular capillaries. Besides glomeruli, adrenomedullin is also distributed in tubules, collecting ducts and vasculature of the rat kidneys.22 In a recent trial, it was shown that, adrenomedullin suppresses endoplasmic reticulum stress induced cell death in renal tubular epithelium, thereby exerting a protective effect on kidney.23 In addition, it is demonstrated that adrenomedullin promotes proliferation and regeneration of renal tubule cells after renal ischemia reperfusion injury by upregulating cyclin D1.24 From this point of view, we are supposed to observe some beneficial effects of adrenomedullin over deteriorated renal functions and renal histology resulted from intravenous contrast media administration. Supporting previous data, the declines in CrCl and daily urine output values were found significantly lower in ACM group compared to CM group. Additionally serum cystatin-C level was detected significantly lower in ACM group; whereas the absolute change values of serum Cr did not differ among the two groups. It should be noted that cystatin-C could predict development of AKI before increase in serum creatinine level as already shown in critically ill patients.25
In the presented study, we did not show any difference in tubular damage and medullary congestion scores of ACM group compared to those in CM group. This result probably suggests that the protective effect of adrenomedullin was mainly exerted on a functional manner rather than an anatomical level. Additionally, the model that we have used for induction of CIN might have prevented us from inducing a severe tubular damage in CM group. An invasive method could have led formation of anticipated histopathological changes and differences among the groups could be more prominent and have reached the significance.
Obstruction of tubules by urinary proteins is known to be associated with CIN.26 In the presented study, consistent with this data, intravenous injection of high dose diatrizoate has significantly increased daily protein excretion. Moreover, administration of adrenomedullin before iodinated contrast media has significantly decreased the excretion. Organ protective effects of adrenomedullin have been demonstrated in various cardiovascular diseases and diabetic nephropathy rat models.27 The exhibited anti-proteinuric effect of adrenomedullin shown in this study might be one of the potential renoprotective mechanisms of it. There is no data regarding the anti-proteinuric effect of adrenomedullin in literature and to our best of knowledge, this is the first study addressing this issue.
Besides its vasodilatory and antioxidant effects, it has been shown that adrenomedullin possesses anti-inflammatory properties also.11,28 Studies indicate that it suppresses secretion of TNF-α from murine RAW264.7 cells stimulated with endotoxin.29 Recent studies also demonstrated that, adrenomedullin suppressed TNF-α release from Kupffer cells significantly12 and it inhibits secretion of cytokine-induced neutrophil chemo-attractant in rat alveolar macrophages stimulated with endotoxin.30 We have used some mediators of inflammation like TNF-α, IL-1β, IL-6 and IL-18 in order to find out the anti-inflammatory effects of adrenomedullin. However, we could not find a significant difference between CM and ACM groups in post-hoc analysis. Inflammatory mechanisms seem to be less important in the pathogenesis of CIN and this may be the reason of this result.
After iodinated contrast media injection, direct toxic effects via release of free radicals and decreased anti-oxidant enzyme activities have been shown in experimental models.31,32 On the other hand, increased oxidative stress production has been exhibited in adrenomedullin gene-deficient diabetic mice compared to wild type counterparts.27 Hence, one could also assume contribution of anti-oxidant properties of adrenomedullin in CIN prevention. However, we have not evaluated oxidative stress in our study.
Although, present study is the first experimental research demonstrating the effectiveness of adrenomedullin against the development of CIN, it has several limitations. First, it is previously reported that creating an experimental contrast nephropathy model presents some difficulties33 and we also could not achieve to make a satisfactory CIN rat model. The mean tubular damage and medullary congestion scores were only 1.67 and 1.17, respectively. It has been previously shown that dehydration potentiates the vasoconstrictive effects of contrast media.34 The use of high-dose and high-osmolar-ionic contrast media, such as diatrizoate, is also another important risk factor for developing CIN.35 Therefore, we used a prolonged dehydration period before the administration of high-dose diatrizoate. However, no best method has been defined currently for making experimental CIN in rats. Second, we have not evaluated the effects of adrenomedullin on glomerular filtration rate directly. Third, as previously mentioned, we have not evaluated oxidative stress of which was most likely to be in the casual pathway of CIN in our study.
In conclusion, this study demonstrated the protective role of adrenomedullin against CIN. Adrenomedullin prophylaxis may be useful in the prevention of CIN; further studies are needed to shed more light on this issue.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. Baseline and the 6th day body weights, urine volumes, serum Cr, BUN, CrCl, FENa and proteinuria levels (n=6 each)
Table 2. The differences in body weights and renal function parameters after the experimental procedures compared to baseline values (n=6 each)
Table 3. Findings of Cystatin-C and inflammatory markers on 6th day (n=6 each)
Table 4. Histology findings in the four groups (n=6 each)
Figure 1. Comparison of absolute change of serum creatinine clearance levels among the study groups