Background: The daily pill burden in hemodialysis patients is one of the highest reported to date in any chronic disease. The adherence to prescribed treatment has implications on the quality of life, the survival of patients, and the economic cost of their treatment, this being a priority public health issue. Objective: To evaluate the adherence to pharmacological treatment examining, among the possible causes of non-adherence, psychosocial factors such as depression, anxiety, cognitive impairment and social support. Method: Transversal-observational study of thirty five patients that suffer from chronic renal disease and who are on manteinance hemodialysis, evaluated by self-reported measures. Results: Non-adherent patients have significant higher depression index than adherent patients. Anxiety, cognitive impairment and social support do not show a significant relation with the degree of adherence or compliance with farmacological treatment. Conclusions: These results suggest that psychological intervention in chronic haemodialysis patients with a severe depression index could increase the degree of fulfillment and general well-being of renal patients.
Introducción: Los pacientes en hemodiálisis (HD) son uno de los colectivos que toma mayor cantidad de comprimidos en comparación con otros enfermos crónicos. La adherencia al tratamiento prescrito tiene implicaciones en la calidad de vida, la supervivencia y el coste económico de su tratamiento, siendo este último un tema prioritario de salud pública. Objetivo: Evaluar la adherencia al tratamiento farmacológico en pacientes en HD crónica examinando, entre las posibles causas de la no adherencia, factores psicosociales como depresión, ansiedad, deterioro cognitivo y apoyo social. Material y métodos: Estudio observacional transversal llevado a cabo en treinta y cinco pacientes con enfermedad renal crónica en HD, evaluados mediante cuestionarios administrados por personal especializado. Resultados: Los pacientes no adherentes presentan índices de depresión significativamente más elevados que los adherentes al tratamiento farmacológico. La ansiedad, el deterioro cognitivo y el apoyo social no muestran relación estadísticamente significativa con el grado de cumplimiento. Conclusiones: Estos resultados sugieren que la intervención psicológica en pacientes en HD con mayores índices de depresión podría aumentar el grado de cumplimiento y bienestar general del enfermo renal.
INTRODUCTION
Patients on haemodialysis (HD) are one of the groups that take the most medicine in comparison to other chronically ill patients. These people do not always follow the recommendations given by medical staff regarding their medication, lifestyle or diet. It is known that not adhering to the prescribed treatment has implications on quality of life, patient survival and economical cost of their treatment, making this a priority topic in public health1.
According to the World Health Organisation, the definition of adhering to treatment would be: “The degree to which the behaviour of a person corresponds to the instructions agreed with a medical professional in terms of taking medication, following the recommended diet and making changes in lifestyle”. In addition, it sets out that there is a series of risk factors that would be related to the lack of adherence1, among which social and emotional factors can be found. Among the social factors, social support, i.e. obtaining resources from interaction with other people has shown to be a determining factor in survival and adherence to treatment2.
In regard to emotional factors, in spite of the high rates of depression in patients on HD, varying between 25%-50%3,4, studies that take into account adherence to treatment in relation to emotional problems are scarce. Some recent data affirm that depression and anxiety are two of the most frequent psychological conditions in kidney patients, which increases the lack of adherence and non compliance with the dietary restrictions as well as the indirect suicide attempts5,6.
In a systematic revision7 on the adherence to oral medication in patients on HD, which includes 19 studies with a variable number of patients (from 19 to 6251), the degree of non-adherence went from 3% to 80%. In 58% of the studies, degrees of non-adherence greater than 50% (average of 67º%) were found8. The psychosocial factors were only analysed in one of them.
Furthermore, various studies focusing on analysing the determining factors of non-adherence with samples of elderly patients argue that a possible cause for not complying with treatment is due to low morale. Along this same topic, another of the factors described as a cause for non-adherence in this group could be forgetfulness, encouraged by deterioration in cognitive functioning and the high proportion of elderly people who live alone and have little support9. For these reasons, it would be interesting to find out if psychosocial factors such as depression, anxiety, cognitive impairment and social and family support have a significantly effect in compliance with medical prescriptions.
The aim of this study is to evaluate adherence to pharmacological treatment in patients on HD examining, among the possible causes for non-adherence, psychosocial factors such as depression, anxiety, cognitive impairment and social support.
MATERIAL AND METHOD
Aim
To study the adherence to pharmacological treatment in a sample of patients on HD and the psychosocial factors such as depression, anxiety, cognitive impairment and social support, that might have an influence on it.
Design
This is a cross-sectional observational study on prevalent patients on HD dated July 2013.
Patients
Prevalent patients on HD of the HD unit in the Infanta Leonor University Hospital in Madrid. For ease of access, the patients in the morning shift were preferably selected.
Inclusion criteria were: a) patients over the age of 18; b) to have been on HD for more than one month; c) to meet the physical, mental and linguistic criteria to be able to answer the questions on the questionnaires; d) to provide their informed consent.
Informed consent
The aims of the research are explained and the informed consent is collected to be able to carry out the necessary surveys and study their data, in accordance with the regulations of the Data Protection Agency.
Methods
Variables analysed
A standardised sheet was created for patients on dialysis in order to obtain information on demographic variables such as age, sex, relating to the HD technique, current living situation and if they receive help or assistance at home.
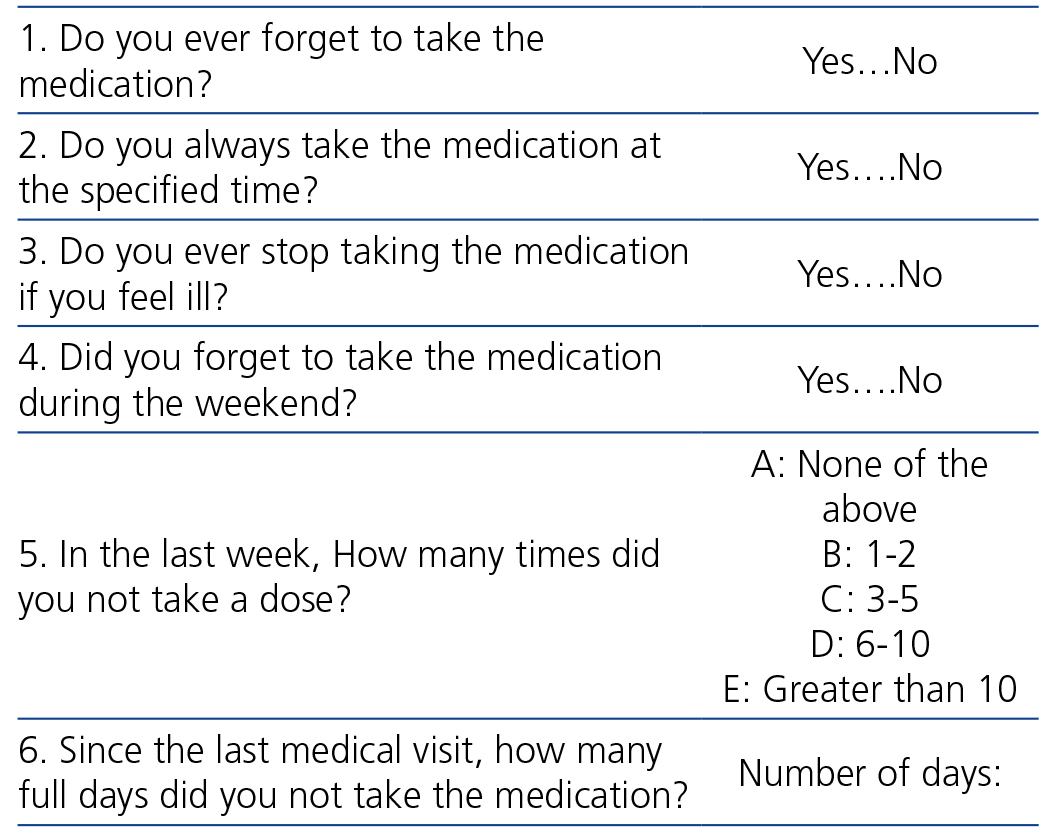
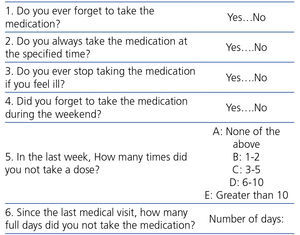
The degree of treatment compliance was measured by the Simplified Medication Adherence Questionnaire (SMAQ)10, validated on the Spanish population of patients on renal replacement therapy (Table 1). This questionnaire consists of six dichotomous questions so any response in the sense of non-adherent will mean that the patient is considered non-adherent.
To evaluate the clinical variables, the following questionnaires were applied:
1. Spanish adaptation of the The Beck Depression Inventory (BDI-II), by Beck, Steer and Brown (1996) by Sanz, García-Vera, Espinosa, Fortún and Vázquez (2005) 11,12: used to evaluate the intensity of symptoms of depression. It is a self-administered questionnaire with 21 items. In each one, the patient must choose the sentence that best describes their state during the last two weeks from between four alternatives ordered from minor to serious severity. Each item is valued from 0 to 3 depending on the alternative chosen and after adding up the points a result varying from 0 to 63 can be obtained. The cut-off points used for grading the intensity of the symptoms of depression are as follows: 0-13 points minimal depression; 14-19 points: mild depression; 20-28 points: moderate depression, and 29-63 points: severe depression.
2. The Beck Anxiety Inventory (BAI), by Beck, Epstein, Brown and Steer (1988) adapted to Spanish by Magán, Sanz and García-Vera (2008)13,14: used for evaluating the presence of symptoms of anxiety and their severity. It is a self-report inventory made up of 21 items. Each item on the BAI takes a symptom of anxiety and for each one of these, the evaluated person must indicate the degree to which they have been affected by this during the last week, using a Likert scale of four points: 0 (nothing at all), 1 (mildly, it did not bother me much), 2 (moderately, it was very unpleasant, but I could stand it), 3 (severely, I could barely stand it). Each item is valued from 0 to 3 depending on the answer and after adding up the points from each item an overall total is obtained whose range is from 0 to 63. The cut-off points used for grading the intensity of the symptoms of anxiety are as follows: 0-7: minimal anxiety; 8-15: mild anxiety; 16-25: moderate anxiety, and 26-63: severe anxiety.
3. The Mini Mental State Exam, by Folstein, Folstein and McHugh adapted to Spanish by Lobo, Sanz et al (2002)15,16 was used to measure cognitive state. It is a test with 30 questions in which the evaluator asks the person to perform tasks and they respond to the questions asked. The Mini Mental detects cognitive disorders by evaluating the following areas: orientation in time and space, coding, attention and concentration, recollection, language and visual construction. Points are given depending on the number of correct answers in the tests, so high scores show a better congnitive functioning. The overall score varies between 0 and 35. The cut-off points used for grading cognitive damage are as follows: 0-10 points severe damage; 11-20 points: moderate damage; 21-26 points: average damage, and 27-35 points: minimal damage.
4. The MOS Questionnaire on social support by Sherbourne and Stewart (1991) adapted to Spanish by De la Revilla (2005)17,18 was used to measure social support. It is a multidimensional questionnaire that allows the evaluation of quantitative aspects (size of the social network) and qualitative aspects (dimensions of the social support): It consists of 20 items. The first evaluates structural support and the rest evaluate functional support. Five dimensions of social support are explored: psychological, informative, tangible, positive social interaction and affection. The interviewee is asked, by means of a 5 point scale, how frequently each type of support is available to them. The factorial analysis advises to join the psychological and informative support items, leaving 4 subscales at the end, which independent scores can be obtained for: psychological support (items 3, 4, 8, 9, 13, 16, 17 and 19 instrumental support (items 2, 5, 12 and 15 positive social interaction (items 7, 11, 14 and 18) and emotional suppot (items 6, 10 and 20). The overall rate of social support is obtained by adding the 19 items together. Social support is scarce when the rate is lower than 57 points. When the scores are lower than the following parameters, support will be needed: psychological support: 24, instrumental support: 12, social interaction: 12, and emotional support: 9.
Procedure and statistical analysis
The tests were applied during the HD sessions. The comorbidity of each patient was checked in their medical records and the Charlson Index was calculated.
Quantitative variables are presented as means and standard deviations (± SD), or as medians (range) in abnormal distribution values.
To compare two independent continuous variables, Student's t test was used for unpaired samples. To compare discrete variables, the χ2 test was used as well as Fisher's test when it was necessary (n<5).Pearson’s correlation coefficient was calculated. A value of P <.05 was considered to be statistically significant.
Statistical analysis was performed and graphics were created using SPSS software version 15.0 (SPSS, Chicago, USA).
RESULTS
The samples was made up of 35 subjects, 22 males and 13 females, with an average age of 68.3 (14) years. Of them, 14 were diabetic; the average body mass index was 24.8 (5.1) (range 17.7-40.4) kg/m2. The average Charlson Index was 5.85 (2-12).
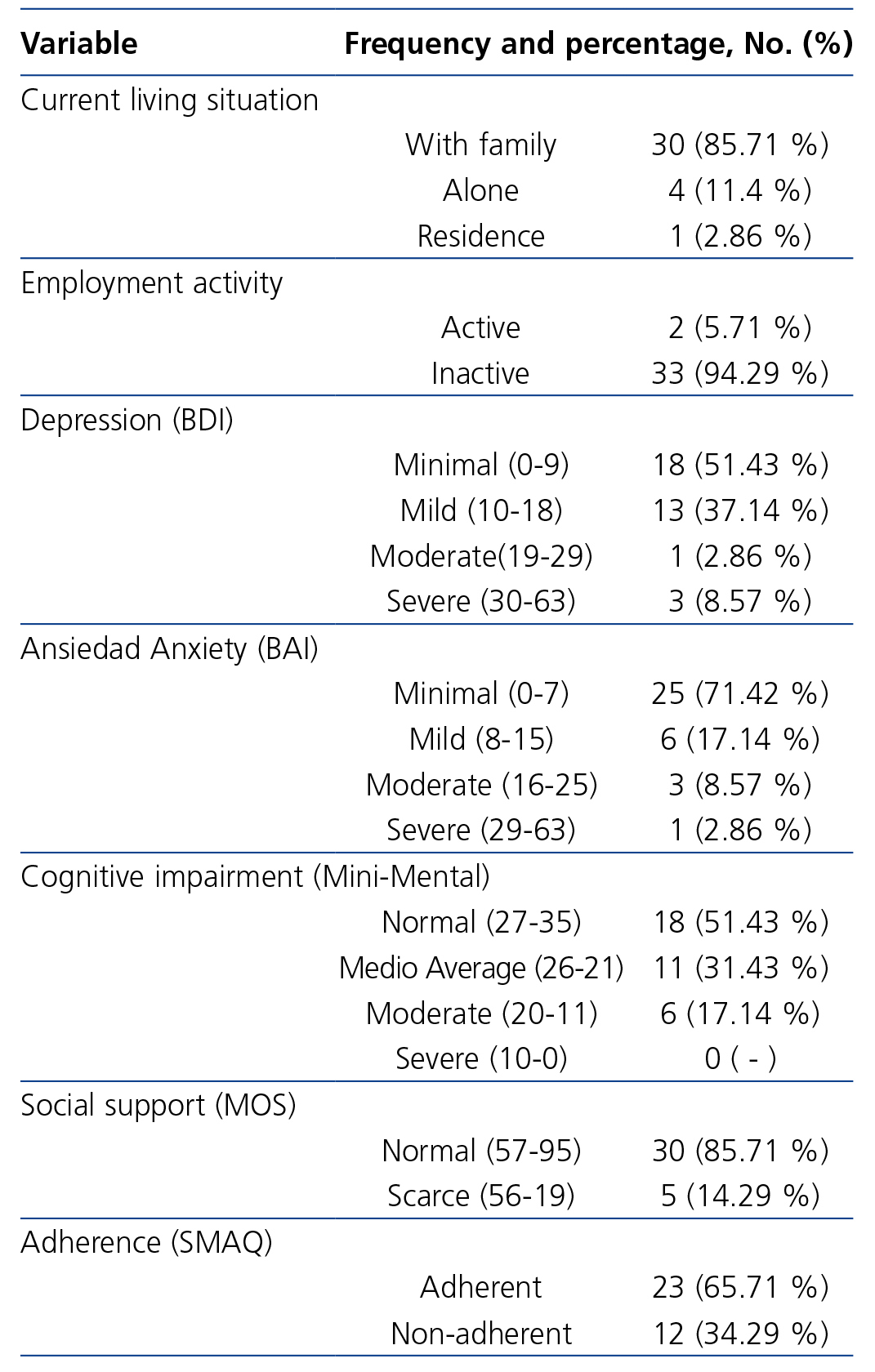
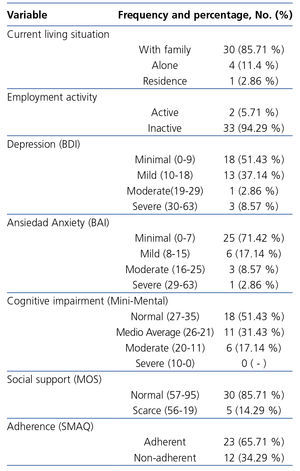
85.71% of the subects lived with family and 94.29º% were out of work, either on leave or retired (Table 2).
All the patients were dialysed three times a week with high-flux dialysers and synthetic membranes. The average time on HD was 81 (2-329) months. The length of the sessions was equal to or greater than 4 hours, apart from the patients with residual renal function greater than 5ml/min average clearing of urea and creatinine. 16 patients were dialysed in post-dilution on-line haemodiafiltration with more than 20l of infusion per session. The average eKt/V was 1.8 (0.45) (range 1.1-2.78). All HD machines had ultrapure dialysate.
Regarding the prescribed medication, the average number of pills taken daily was 10.97 (4-20).
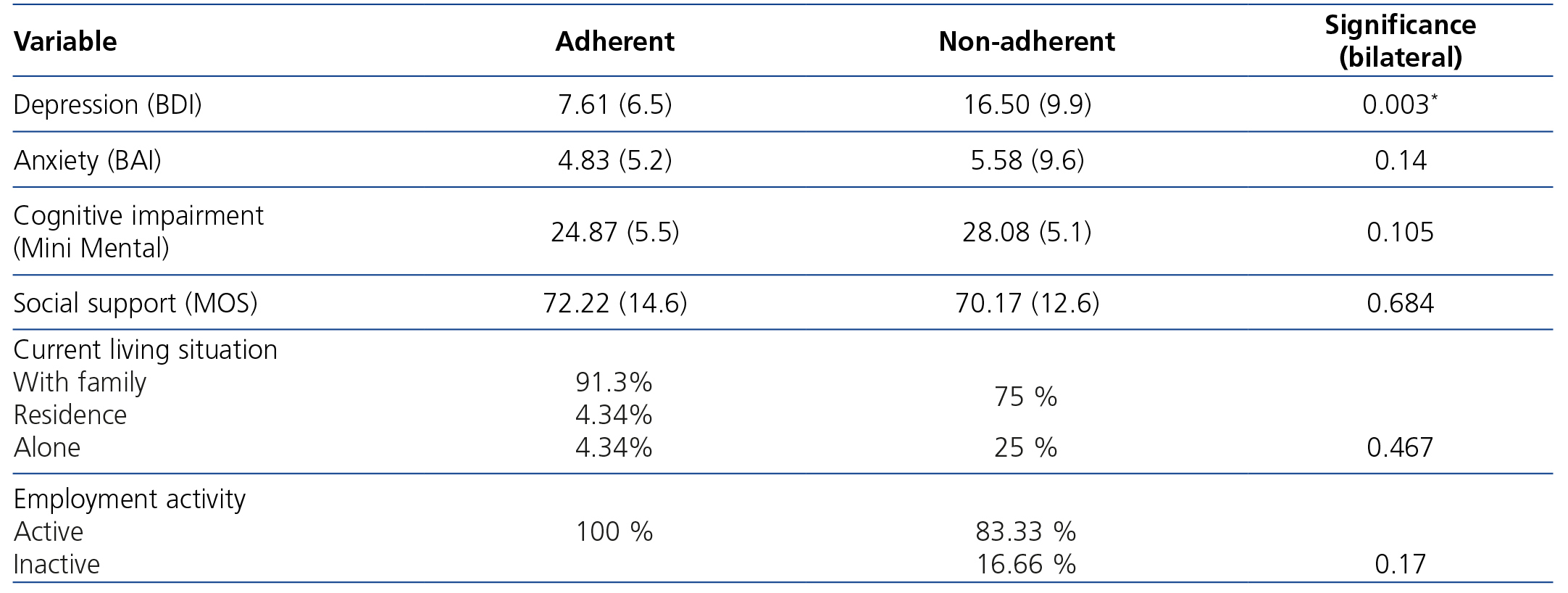
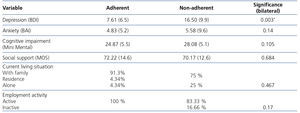
We found that 65.7% of the patients adhered to the pharmacological treatment vs. the 34.4% that did not (Table 2). There were no differences in adherence related to age or sex. Nor was a relationship found with the living or employment situation, but it must be considered that most patients lived with family and were not working. The non-adherent patients showed significantly higher rates of depression (P=.003) than those who adhered to the pharmacological treatment.
Adherence to the pharmacological treatment did not show significant differences in terms of anxiety, cognitive impairment or social support.
Other results
In regard to the psychological variables, 48.6% of the subjects showed average-to-moderate cognitive impairment, 40% suffered from mild-to-moderate depression and, to a lesser extent, 25.7% showed mild-to-moderate rates of anxiety (Table 2).
The females showed significantly higher levels of anxiety (P=.005) and cognitive impairment (P=.04) than the males.
Depression and anxiety were significantly related (r=0.63, P<.0001).
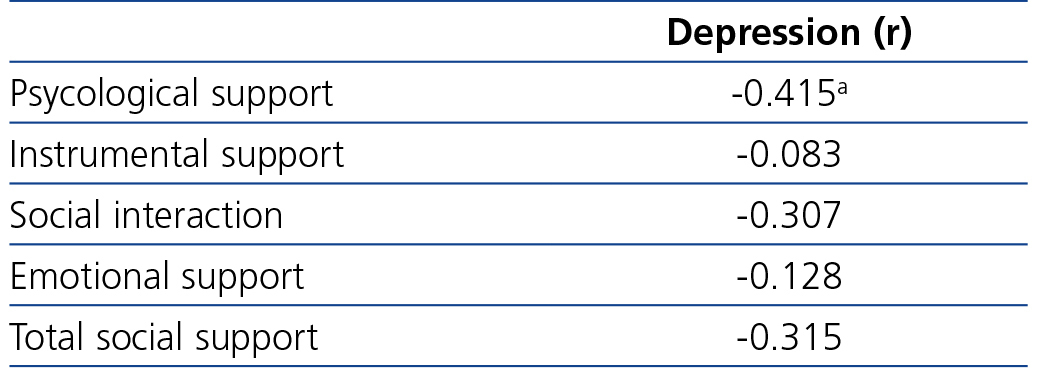
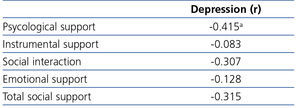
There is an inverse correlation between depression and social support in the emotional dimension, i.e., greater rates of depression are related to low levels of emotional support. The rest of the social support parameters had no connection to depression (Table 3).
DISCUSSION
The treatment adherence obtained was 66%, a statistic that agrees with research on adherence in chronic diseases19, additionally showing that the non-adherent patients had higher rates of depression.
Although the number of daily pills is high, we consider that the degree of adherence found in our unit is satisfactory. We believe that these good results could be due to the fact our patients were in constant communication with their healthcare professionals and said they were highly satisfied with their relationship with the medical staff in the annual survey carried out in the HD unit, within the ISO 9001 monitoring. Even so, a high percentage of patients did not adhere to the treatment, so investigating the causes of this is a very relevant aspect in order to improve it. Better adherence would possibly reduce the number of daily pills since in practice non-adherence provokes “inefficacy” and as a consequence, an intensification of the treatment.
There are few studies that relate adherence to treatment with the emotional problems of the patients on HD. Anxiety, cognitive impairment and social support are not connected to the degree of adherence to treatment (Table 4), although depression is. This finding is very important given that depression is a treatable condition and doing so could have a beneficial effect on the degree of adherence to treatment.
We believe that the lack of a relationship between anxiety and adherence to treatment could be due to the fact that part of the symptoms of physical anxiety registered on the questionnaires were actually symptoms from the renal disease or others (palpitations, sweating, dizziness, numbness, shaking)20.
Some studies argue that young patients tend to not to adhere to treatment21. In our study, we have not found a relationship between socio-demographic variables (age, sex) and adherence. Furthermore, bearing in mind the average age of the sample (68.3 years), a certain amount of non-adherence could be expected due to the deterioration of cognitive functions, forgetfullness and the high proportion of elderly people who live alone and have little support. The results conflicting with data obtained in other research9 could be explained by the high levels of social support that most of the evaluated patients had, meaning that studies conducted in different countries might not be universal due to there being different social determinants depending on the culture.
If we focus on the results of the different questionnaires in isolation, we find that a quarter of the sample studied shows anxiety and 40% show mild or moderate depression which agrees with the prevalence found in other studies8,9. We also observe that the social support is high in most of the evaluated subjects and that a large proportion show average to moderate levels of cognitive impairment.
Studying the relationships, the results show that greater levels of depression are related to high degrees of anxiety. Similarly, low levels of emotional support are related to greater levels of depression (Table 3).
The main limitation of our study is that we had a small number of patients so it would be necessary to perform a broader study to better identify the problems and evaluate their solution in a second step.
As a conclusion and also as a reflection, we often underestimate the levels of depression and anxiety in the patients on dialysis, focusing our dedication and efforts on offering better dialysis and pharmacological treatment. This study shows the impact that depression has on adherence to treatment, so any psychological or pharmacological intervention on depresion could improve adherence to treatment. The problem is that few HD units normally have a psychologist present to evaluate and help the patients which could increase the degree of compliance and general well being of the renal patient.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. Simplified Medication Adherence Questionnaire
Table 2. Descriptive statistics
Table 3. Depression-social support correlation
Table 4. Differences between adherent and non-adherent patients and level of signification