Introducción: determinar el filtrado glomerular al ingreso como predictor de mortalidad tras un Síndrome Coronario Agudo (SCA). Pacientes y método: se analizaron 290 pacientes que ingresaron por SCA durante el año 2003. Se valoró la función renal al ingreso mediante la fórmula de estimación del Filtrado Glomerular (FG) MDRD. Se estratificaron en tres grupos: pacientes con FG ≥60 ml/min/1,73 m2; n = 186, pacientes con FG <60 y >_30; n = 93 y pacientes con FG <30; n = 11. Resultados: todos los pacientes con FG <30 ml/min presentaron un SCA sin elevación del segmento ST, los cuales eran de edad más avanzada con mayor prevalencia de eventos cardiovasculares previos (accidente vascular cerebral, de arteriopatía periférica, y de infarto de miocardio). La realización de pruebas diagnósticas fue menor. La mortalidad hospitalaria fue del 27,3% en los pacientes con FG <30 ml/min, 7,5% en los pacientes con FG entre 30 y 60 ml/min, y del 3,8% en los pacientes con FG ≥60 ml/min. Tras dos años de seguimiento, la mortalidad fue del 27,3% en los pacientes con FG <30 ml/min, del 20,4% en los pacientes con FG entre 30 y 60 ml/min, y del 10,2% con FG ≥60 ml/min. Al ajustar por otras variables pronósticas, los pacientes con FG <30 ml/min presentaron una mayor mortalidad tanto durante el ingreso como en el seguimiento a dos años. Conclusiones: la reducción del FG es un factor de riesgo independiente de mortalidad tras un SCA. El uso de las fórmulas de estimación del FG en el seguimiento de dichos pacientes tiene valor pronóstico.
Introduction: renal glomerular filtration rate on hospital admission in patients presented with an acute coronary syndrome as a predictor for mortality. Patients and methods: The study analysed 290 patients admitted on hospital with an acute coronary syndrome during one year (2003). Renal function was estimated using the renal glomerular filtration rate by the MDRD formula. Patients were stratified in three groups: patients with a GFR > or = 60 ml/min/1,73 m2; n = 186, patients with GFR < 60 or > 30; n = 93 and patients with GFR<30; n = 11. Results: 66.6% of patients were males and 66.5% were older than 65 years old. 54.5% suffered from hypertension and 39% were diabetics. All patients with GFR < 30 ml/min had an acute coronary syndrome without elevation of ST segment. They were the oldest with a major proportion of previous cardiovascular events as cerebrovascular disease, peripheral vascular disease or myocardial infarction. Diagnostic procedures and treatments were less administered in patients with GFR < 30ml/min. Although in the univariate analysis demonstrated that hospital mortality was related to GFR < 30ml/min, sex, ageing, Killip > 1, ventricular function and cTnT elevation, only GFR < 30ml/min, ageing, heart failure and ventricular dysfunction persisted significant in the multivariate analysis. Hospital mortality was 27.3% in patients with GFR < 30ml/min, 7.5% in patients with GFR between 30-60ml/min and 3.8% in patients with a GFR > or = 60ml/min. Mortality after two years follow up was 27.3% in patients with GFR<30ml/min, 20.4% in patients with GFR between 30-60ml/min and 10.2% in patients with a GFR > or = 60 ml/min. Mortality ( hospital mortality and after two years of follow up) was increased in patients with GFR< 30ml/min, ageing, heart failure and diabetes after adjusted for other prognostic factors. Conclusions: A reduced glomerular filtration rate is an independent risk factor for mortality in patients with an acute coronary syndrome. Estimation of the renal glomerular filtration rate might be used as prognostic value in these patients.
INTRODUCTION
Renal failure is a risk factor in the development of coronary disease1,3-5 and is associated with a poorer prognosis of cardiovascular disease to such an extent that the risk of death in patients with kidney disease, particularly from cardiovascular disease, is higher than the risk of requiring renal replacement treatment.6
The findings obtained from clinical trials7,8 and from studies involving patients with ACS9-11 suggest that there is a link between impaired renal function and a poorer prognosis of ACS, as well as with a decrease in the use of conventional treatment and reperfusion therapy.
Despite the fact that these studies highlight a link, it is worth emphasising that in most clinical trials renal failure (generally measured by the level of plasma creatinine) has consistently been one of the exclusion criteria and therefore the information that we have cannot be generalised and applied to a non-selected population of patients with ACS.
Even though there is a reciprocal relation between the levels of creatinine and the renal GFR, this relationship may vary substantially in one person over the course of time.12 Therefore, it is possible to find seemingly normal levels of plasma creatinine which correspond to a glomerular filtration rate below 60ml/min. Generalised formulas that estimate the GFR, like the Cockcroft-Gault formula13 or the MDRD formula14 which evaluates renal function in elderly patients, obese patients and female patients with more accuracy, provide a more precise analysis of renal function which could be useful in the treatment of patients with ACS.
With regard to the early prognostic stratification following coronary syndrome, we know that only the risk model in the GRACE15 study and the risk score in the CADILLAC16 study on NSTE-ACS evaluated renal function as a risk factor, whereas in other frequently used risk scales like the TIMI17,18 scale, renal function is not mentioned.
Therefore, the aim of this study is to establish the link between the different grades of renal failure on the basis of the estimated GFR at admission into hospital and general mortality, both during admission and during the two-year follow up period for patients admitted into hospital with ACS.
METHODS
A total of 333 patients were admitted into Terrassa Hospital with ACS between 1 January and 31 December 2003. A diagnosis was made on the basis of the new definition,19 and patients admitted with the following profiles were admitted: a) chest pain with an increase in markers of myocardial injury or a positive exercise stress test or a history of coronary disease; b) chest pain with changes in the electrocardiogram (ECG) suggestive of myocardial ischaemia; and c) no chest pain but an increase in markers of myocardial injury and changes in the ECG suggestive of myocardial ischaemia and/or a positive provocative test for ischaemia during admission. Patients were divided according to the presence of ST segment elevation: 1) ACS with ST segment elevation: when the ST segment elevation was evident in at least two derivations for more than 20 minutes; 2) unclassifiable ACS: patients with pacemakers, left bundle branch block (LBBB) or preexcitation; and 3) no ST segment elevation: when patients fulfilled the ACS criteria and did not belong to the two aforementioned categories.
The first patient admitted with ACS during this period was considered a valid subject for this study. Subsequently, the medical history and previous cardiovascular risk factors of a group of 290 patients that were admitted consecutively were retrospectively analysed.
Given the complexity of the hospital, an early non-invasive ACS strategy was applied to all patients.
The follow-up period lasted two years (until 31st January 2006) and was undertaken by consulting the patients’ medical histories and/or enquiring by phone during the month of February 2006, without counting patients lost during the follow up period. Patients on haemodialysis were not excluded.
The study was accepted by the Research Assessment Committee of the Terassa Hospital.
The creatinine measurements taken at admission were analysed in the hospital’s internal laboratory using standardised methods with a coefficient of variation below 2%. The GFR was estimated using the MDRD equation.14 The level of cardiac troponin T (cTnT) was also verified in the internal laboratory, the cut off point was established at 0.1ng/ml and the maximum value during the ischemic event was analysed.
The main parameter evaluated was general mortality both during admission and the two-year follow up period.
Patients were divided into three groups based on their basal Glomerular Filtration Rate (GFR): GFR ≥ 60ml/min/1.73m2, GFR ≥ 30 and < 60ml/min/1.73m2 and GFR < 30ml/min/1.73m2, following the classification set out in the guidelines established by the National Kidney Foundation. Patients with a GFR ≥ 60ml/min/1.73m2 were considered the reference group, bearing in mind that the MDRD formula has been developed for patients with chronic kidney disease (and therefore with a GFR below 60ml/min.)
The quantitative variables that have a normal distribution are presented as the mean (standard deviation) and were compared using the Student’s t-test or the ANOVAtest. The quantitative variables that have a non-normal distribution are presented as the median (interquartile range) and have been analysed using the Mann-Whitney U-test. Qualitative variables are presented as absolute values and percentages with regard to the GFR classification and have been analysed using the χ2 test.
In order to carry out the evaluation of mortality a descriptive analysis was undertaken using the Kaplan-Meier test, comparing the different GFR groups using the log rank test. Furthermore, the Cox proportional hazard model was used for the regression study and the multivariate analysis was carried out using the backward elimination of variables that had a value of p < 0.30 in the univariate analysis, as well as those variables that were considered clinically relevant. Coefficients were expressed as a Hazard Ratio (HR) with a 95% CI. All p values were bilateral and were considered statistically significant if they were below 0.05. SPSS software for Windows®, version 11.00, in Spanish was used for the analysis.
RESULTS
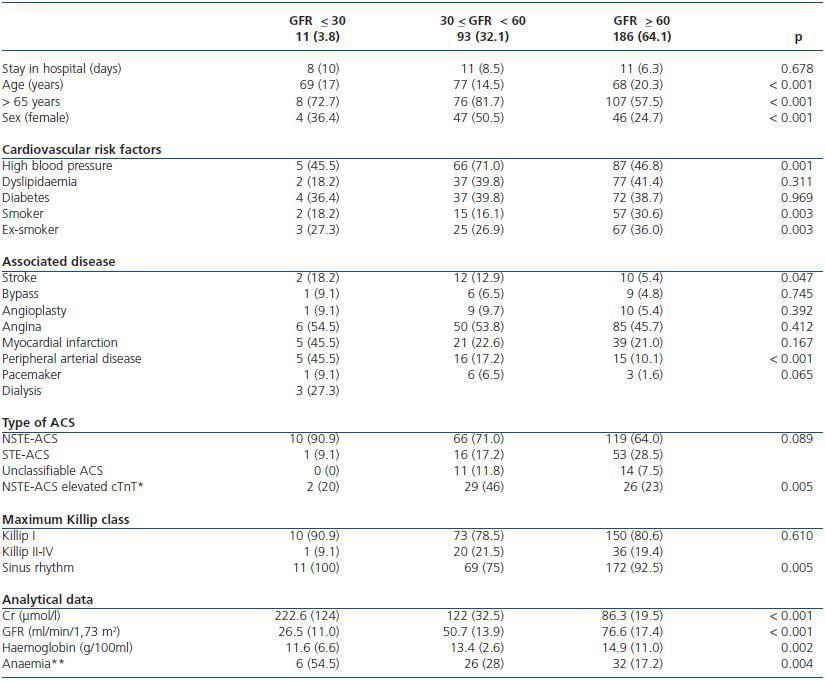
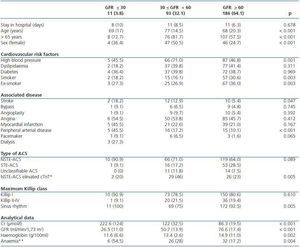
A total of 290 patients (table 1) were included in the study. Of these, 66.6% were male and the mean age (interquartile range) was 71 (20); of these patients 66.5% were over 65 years of age. 54.5% suffered from high blood pressure, 40% had dyslipidaemia, 39% were diabetic and 58.3% were smokers or ex-smokers. 8.3% had suffered a stroke, 12.4% had peripheral arterial disease, 48.6% had a history of ischemic heart disease in the form of angina and 22.4% had suffered a previous myocardial infarction. Angioplasty had been carried out on 6.9% of patients and 5.5% had undergone coronary revascularization surgery. Three patients (1%) were on dialysis. 67.2% had been admitted with NSTE-ACS (of which 30.6% had elevated cardiac troponin T cTnT), 24.1% with STE-ACS and 8.6% with unclassifiable ACS.
The patients with chronic renal failure (30 ≤ GFR < 60 and GFR < 30ml/min/1.73m2) presented the following differentiating characteristics: elderly, predominantly male, high blood pressure, coronary as well as cerebral artery disease and above all peripheral arterial disease (45.5% of patients with a GFR < 30, 17.2% with a GFR < 60 versus 10.1% of patients in the group with a GFR ≥ 60), as well as lower haemoglobin levels with 54.5% patients in the GFR < 30 group suffering from anaemia (defined as haemoglobin < 13g/100ml in men and < 12g/100ml in women), 28% in the group with a 30 ≤ GFR and < 60 versus 13.2% in patients with a GFR ≥ 60.
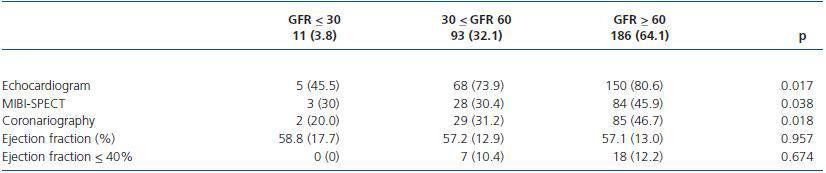
With regard to the additional examinations carried out, electrocardiograms were performed in 77.2% of cases, the stress exercise test (which was gammagraphic in all cases) on 40.4% of patients and a coronariography on 40.7%. It is clear from table 2 that echocardiograms, ergometry tests and blood testing in particular were carried out less frequently on patients that belonged to the groups 30 ≤ GFR < 60 and GFR < 30ml/min/1.73m2.
There were no differences between the groups with regard to ventricular function (11.4% had ≤ 40% ventricular function) nor in relation to the seriousness of the coronary disease those who underwent a coronariography: 12.8% did not present any significant lesions according to the angiography, blood vessel disease affecting a single vessel was detected in 30.3% of cases and affecting multiple vessels in 56.9%. No differences were observed with regard to the proportion of patients who underwent revascularisation which was 61.1% of the total number of patients who underwent catheterisations, using the percutaneous approach in 48.5% of cases and the surgical approach in 12.6%.
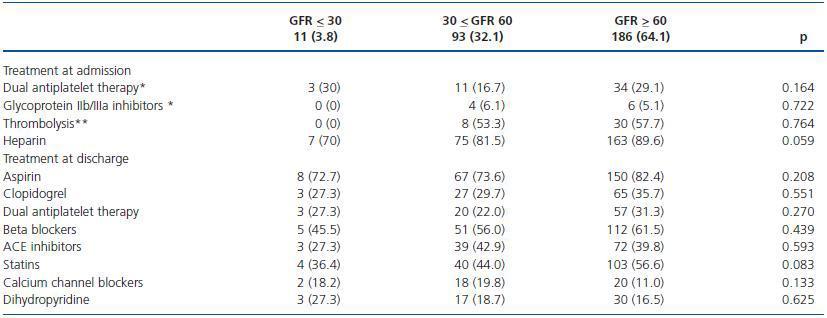
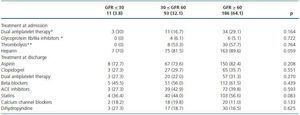
The treatments administered during admission as well as at discharge can be found in table 3. Thrombolysis was recommended for 56.7% of patients with STE-ACS. Dual antiplatelet therapy was given to 24.9% of patients with NSTE-ACS and glycoprotein IIb/IIIa inhibitors were used in only 5.2% of cases. Although it was not statistically significant, the decrease in the use of anticoagulant doses of heparin in groups with 30 < GFR < 60ml/min/1.73m2 (81.5%) and GFR < 30ml/min/1.73m2 (70%) compared to the group with a GFR > 60ml/min/1.73m2 (89.6%) does seem to be of some clinical importance. There were no differences in the treatment administered to patients at discharge.
THE IMPORTANCE OF KIDNEY DISEASE STAGES WITH REGARD TO HOSPITAL MORTALITY
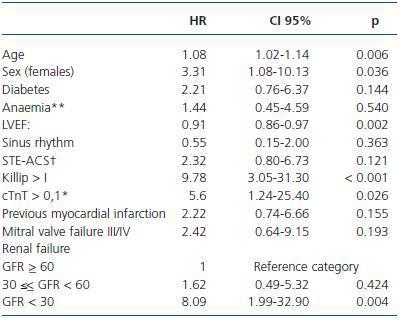
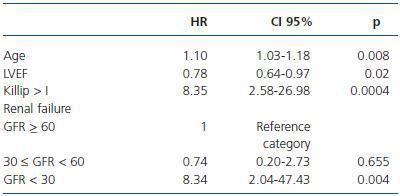
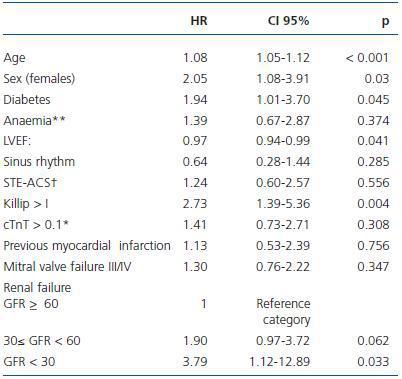
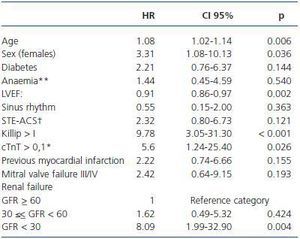
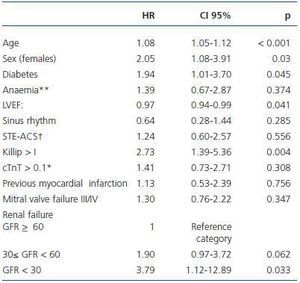
Hospital mortality in our sample was 5.9 and 3.8% in the group with a GFR ≥ 60 ml/min/1.73m2, 7,5% in the group with a 30 ≤ GFR < 60ml/min/1.73m2, and 27.3% in the group with a GFR < 30ml/min/1.73m2. The Cox regression study was carried out. The univariate analysis showed that the variables associated with hospital mortality were a GFR < 30ml/min/1.73m2, age, being female, Killip > I, ventricular function and elevated cTnT (table 4.) These statistically significant variables were included in the multivariate analysis, as well as other variables of clinical relevance, for example stratified renal function, anaemia, sinus rhythm, diabetes mellitus, the type of ACS, the cause of myocardial infarction and moderate-serious mitral valve failure (table 5.) Severe renal function impairment, heart failure during admission, age and ventricular function were the independent factors linked to higher hospital mortality.
THE IMPORTANCE OF KIDNEY DISEASE STAGES WITH REGARD TO MORTALITY DURING THE FOLLOW UP PERIOD
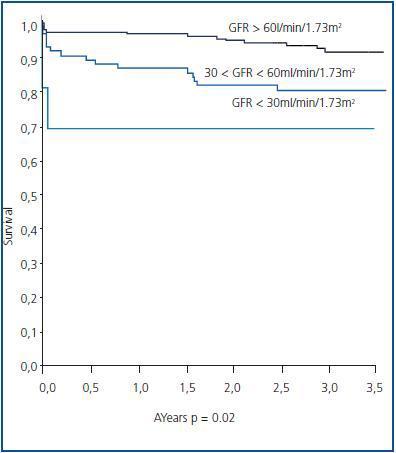
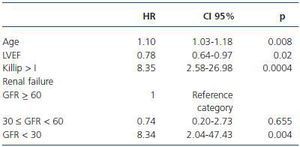
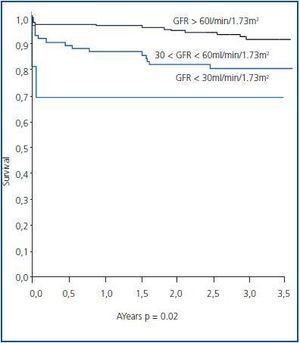
The mean follow up period for these patients after the coronary event was 2.4 (0.85) years. General mortality was 14.1 and 10.2% in the group with a GFR > 60ml/min/1.73m2, 20.4% in the group with a 30 < GFR < 60ml/min/1.73m2 and 27.3% in the group with a GFR < 30ml/min/1.73 m2. Figure 1 shows the Kaplan-Meier survival curves of the three groups of patients.
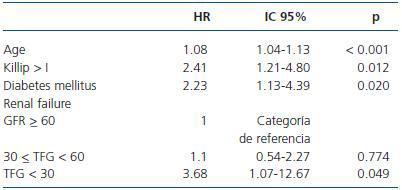
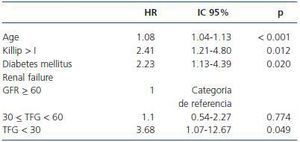
The univariate and multivariate regression analyses can be found in table 6 and 7 and they include the classification of renal function as well as age, sex and other risk factors associated with an unfavourable prognosis such as ventricular function, diabetes mellitus, heart failure, anaemia, sinus rhythm, the type of ACS, previous stroke and severe mitral valve failure. Once again, a GFR < 30ml/min continued to be an independent risk factor linked to mortality during the two year follow up period, as well as a cause of diabetes mellitus and heart disease, whereas while ventricular function was associated with a higher risk in the univariate analysis, it was less statistically significant in the multivariate analysis.
DISCUSSION
This observational study carried out on a non-selected population who were admitted into hospital with ACS clearly highlights the link between cardiovascular disease and kidney disease: patients with kidney disease who are admitted with ACS have higher cardiovascular morbidity, are older and undergo fewer additional invasive and noninvasive examinations, their prognosis is also unfavourable both during their stay in hospital as well as during the follow up period. Taking into account the higher cardiovascular morbidity and unfavourable prognosis, kidney disease could therefore reflect generalised arteriosclerosis.
Similar findings emerged in the GRACE study:20 the presence of cardiovascular risk factors, established cardiovascular disease, and, most importantly, that the prevalence of kidney disease in ACS patients was similar to that observed in our study: 64.5% of patients had normal or slightly impaired renal function, 28.9% had moderate renal dysfunction and 6.7% had severe renal dysfunction. The results showed an increase in the risk of death and bleeding in patients with moderate or severe kidney disease compared to the group with normal renal function. In the case of this study, the risk was significantly higher in the group with greater renal function impairment; however, although the risk was greater in the group with a GFR between 30 and 60ml/min, it was not statistically significant (in the hospital results and during the follow up period.) The use of thrombolysis, glycoprotein IIb/IIIa inhibitors and coronary intervention was less common in groups with impaired renal function and in the treatment administered at discharge. In the case of this study, we did not observe any significant differences in relation to this point, although the percentage of beta blockers and angiotensin II receptor blockers used was slightly lower, which was not the case for antiplatelet therapy and statin treatment. Furthermore, it seems that the “therapeutic nihilism” evident in these groups of patients21-23 cannot be justified, despite the possible toxic effects of cardiovascular treatment. Moreover, when these drugs are monitored correctly, the treatments used by the general population are also safe and patients hardly experience any renal function impairment, obtaining the same1,2,5,8,24,25 or even greater benefits. Three patients on dialysis were included in the group with a GFR < 30ml/min (n = 11). After analysing their demographic characteristics in relation to mortality, we observed that one of the patients had died and the other two had survived by the end of the study without having been admitted because of a cardiovascular condition. It is suggested that the increase in risk is proportional to the decrease in glomerular filtration. In the same way, Facila et al.11 also observed a direct increase in risk without a cut off point after which patients showed an increased risk. Similar observations have recently been made by other authors26-28 highlighting that the risk probably depends as much on renal function impairment as on the increased presence of cardiovascular risk factors like diabetes and symptomatic arteriosclerosis. Chronic kidney disease is considered a cardiovascular risk factor per se.1
The generalised use of formulas to estimate the GFR on the basis of plasma creatinine in clinical practice enables us to obtain more accurate information about renal function. Taking into account the link between renal function and the prognosis of patients with ACS, the estimation of the GFR in these patients is useful both during the initial clinical evaluation and the outpatient follow up.
As in any retrospective analysis, our study has some limitations, including selection bias, the bias inherent when basing a study on a limited population and a single centre. As a result, the conclusions are less representative of the general population. The formula used to calculate creatinine clearance (MDRD) was developed for populations with chronic kidney disease and therefore its use should be limited to this particular group and not applied to subjects without renal disease. Furthermore, the calculation of renal function requires figures that are stable, which was not possible in this group of patients because of their haemodynamic condition at admission.
Another limitation affecting this study was the asymmetric nature of the groups, given that there were fewer patients in the advanced chronic kidney disease group. The high prevalence of arteriosclerosis is well known among these patients and therefore cardiovascular mortality is more probable than the development of kidney disease. The increased mortality justifies the lower number of patients with ACS and advanced chronic kidney disease in our study.
Furthermore, we also observed a higher mortality in the group of patients with a GFR < 30ml/min at admission. This may be due to the patients’ deteriorated condition and the effects of symptomatic or asymptomatic cardiovascular disease in its later stages.
CONCLUSIONS
The findings of this study suggest that for patients with ACS, the GFR is an important and independent predictor of hospital mortality and general mortality during the two-year follow up period.
Higher mortality is associated with higher grades of kidney disease and less aggressive treatment during the patient’s stay in hospital. These findings confirm the importance of taking into account the GFR when dealing with patients with ACS.
Table 1. General clinical and analytical characteristics of patients admitted with acute coronary syndrome according to their glomerular filtration rate in ml/min/1.73m2
Table 2. Additional examinations and ventricular function
Table 3. Treatment administered during admission and at discharge
Table 4. Analysis of hospital mortality. Cox regression. Univariable. Variables with a value of p < 0.3 and clinically important variables
Table 5. Analysis of hospital mortality. Cox regression. Multivariable
Table 6. Analysis of mortality during the follow up period. Cox regression. Univariable. Variables with a value of p < 0.3 and clinically important variables
Figure 1.
Table 7. Analysis of mortality during the follow up period. Cox regression. Multivariable