Objetivos: Los objetivos del presente trabajo fueron conocer qué métodos de anticoagulación se emplean en la práctica habitual en los pacientes en hemodiálisis (HD) en España, de qué criterios dependen y las complicaciones derivadas de su uso. Material y métodos: Es un estudio de diseño transversal basado en dos tipos de encuestas, una de centros y otra de pacientes. La primera fue contestada por 87 unidades de HD de adultos que incluían 6.093 pacientes, y 2 unidades pediátricas; 43 centros (48,3%) eran de titularidad pública y 46 (51,7%), privada/concertada. En la encuesta de pacientes se analizaban 758 pacientes elegidos al azar de manera aleatoria en 78 unidades de HD. Resultados: A) Encuesta de centros: La mayoría de los centros de adultos (n = 61, 70,2%) disponían tanto de heparina de bajo peso molecular (HBPM) como de heparina no fraccionada (HNF), 19 (21,8%) sólo emplean HBPM y 7 (8%) utilizaban exclusivamente HNF. Las criterios más frecuentes para el empleo de HBPM fueron indicaciones médicas (83,3% de los centros) y la comodidad en la administración (29,5%). Los métodos más empleados para el ajuste de la dosis eran la coagulación del circuito (88,2% de los centros), el sangrado del acceso vascular tras la desconexión (75,3%) y el peso del paciente (57,6%). B) Encuesta de pacientes: La distribución del tipo de heparina empleada fue: 44,1% HNF, 51,5% HBPM y 4,4% diálisis sin heparina. La HBPM se utiliza más frecuentemente en los centros públicos (64,2% de los pacientes) que en los privados/concertados (46,1%) (p < 0,001). La HBPM se utilizaba con mayor frecuencia en la hemodiafiltración en línea que en la HD de alto flujo (p < 0,001). Un 45,5% de los pacientes recibían antiagregantes, un 18,4% anticoagulantes orales y un 5% ambos. El 4,4% de los pacientes tuvo complicaciones hemorrágicas en la última semana y el 1,9% complicaciones trombóticas. Las complicaciones hemorrágicas fueron más frecuentes en los pacientes que tomaban anticoagulantes orales (p = 0,01). No había asociación entre el tipo de heparina y las complicaciones hemorrágicas. Conclusiones: Se puede concluir que existe una gran disparidad de criterios en la prescripción de la anticoagulación en HD. Es aconsejable revisar los resultados propios y externos, y posiblemente crear una guía de anticoagulación en hemodiálisis.
Objectives: This study’s objectives were to determine which anticoagulation methods are commonly used in patients who are undergoing haemodialysis (HD) in Spain, on what criteria do they depend, and the consequences arising from their use. Material and Method: Ours was a cross-sectional study based on two types of surveys: a "HD Centre Survey" and a "Patient Survey". The first survey was answered by 87 adult HD units serving a total of 6093 patients, as well as 2 paediatric units. Among these units, 48.3% were part of the public health system and the remaining 51.7% units were part of the private health system. The patient survey analysed 758 patients who were chosen at random from among the aforementioned 78 HD units. Results: A) HD Centre Survey: The majority of adult HD units (n=61, 70.2%) used both kinds of heparin, 19 of them (21.8%) only used LMWH and 7 of them (8%) only used UFH. The most frequently applied criteria for the use of LMWH were medical indications (83.3% of HD units) and ease of administration (29.5%). The most frequently used methods for adjusting the dosage were clotting of the circuit (88.2% of units), bleeding of the vascular access after disconnection (75.3%), and patient weight (57.6%). B) Patient Survey: The distribution of the types of heparin used was: UFH: 44.1%, LMWH: 51.5%, and dialysis without heparin in 4.4% of patients. LMWH was more frequently used in public medical centres (64.2% of patients) than in private medical centres (46.1%) (P<.001). LMWH was more frequently used in on-line haemodiafiltration (HF) than in high-flux HD (P<.001). Antiplatelet agents were given to 45.5% of patients, oral anticoagulants to 18.4% of patients, and both to 5% of patients. Additionally, 4.4% of patients had suffered bleeding complications during the previous week, and 1.9% of patients suffered thrombotic complications. Bleeding complications were more frequent in patients with oral anticoagulants (P=.001), although there was no association between the type of heparin and the occurrence of bleeding or thrombotic complications. Conclusions: We are able to conclude that there is a great amount of disparity in the criteria used for the medical prescription of anticoagulation in HD. It is advisable that each HD unit revise their own results as well as those from other centres, and possibly to create an Anticoagulation Guide in Haemodialysis.
INTRODUCTION
In haemodialysis (HD), a common issue arises in the form of coagulation of the extra-corporeal blood circuit, which must be prevented, normally by administering heparin. The objective is to use the lowest possible dose of anticoagulant so as to maintain the dialyser and venous chamber free from blood cell debris. Another objective is to be able to quickly achieve haemostasis at the vascular access points after the session. In general, the doses applied tend to be lower than the necessary amount for complete anticoagulation, although these doses vary widely between patients, and depend on both patient and HD characteristics.1,2 On the other hand, insufficient anticoagulation therapy can decrease the effectiveness of dialysis to purify the blood.1,2
Several different issues can arise from applying repeated and intermittent heparin to patients on HD programmes, which can involve over 600 cumulative hours per year. These include risk of bleeding and thrombotic complications (which are not always correlated with over or under-dosing), metabolic effects, primarily dyslipidemia, osteoporosis, and effects on blood cells, especially platelets.1,2
Since the 1980’s, low molecular weight heparin (LMWH) has been incorporated into daily clinical practice as an alternative to conventional, or unfractionated heparin (UFH), with the goal of improving efficacy and safety, reducing the secondary side effects produced, and facilitating patient management in terms of dosage adjustments and administration regimens.3-5 Several different studies have shown that LMWH and UFH have similar levels of efficacy and safety.6-7 As regards side effects, studies have shown that LMWH produces a lower increase in plasma triglyceride levels8,9 and lower incidences of thrombocytopoenia10 and osteoporosis11 than UFH. The ease of administration, higher cost, persistence of anticoagulation activity several hours after the HD session, risk of accumulation using high and frequent doses, and the complexity of adjusting doses using laboratory control tests are also factors to take into account when prescribing LMWH over UFH. Thus, whereas the guidelines recommend using LMWH over UFH,12 in current clinical practice, there is no established consensus for prescribing one type of heparin or the other.
In addition to the individualisation of the type and dose of heparin to be used, other aspects of this treatment also lack standardised criteria, such as system priming with or without heparin (and if so, the dose to be used), the mode of administration, and the prescription for anticoagulation based on the HD technique used. For their part, elderly age and cardiovascular comorbidity already necessitate oral anti-platelet and/or anticoagulant treatment in an undetermined percentage of prevalent HD patients, for which there are no general recommendations when considering prescribing anticoagulation therapy during an HD session.
Given the heterogeneity of the possible variables, approaching to this subject first involves defining the current situation in clinical practice, that is to say, document which methods are being applied in the various dialysis centres around the country. For this reason, the Task Force for Anticoagulation in Haemodialysis of the Spanish Society of Nephrology (S.E.N., for its initials in Spanish) proposed a study based on surveys completed by all of the haemodialysis units in Spain, with the objectives of, firstly, assessing which anticoagulation methods are being used in Spain, secondly, what criteria define which methods to use, and finally, which method is more commonly associated with bleeding and thrombotic complications.
MATERIAL AND METHOD
Ours was a cross-sectional descriptive study based on two different types of surveys: one survey for haemodialysis centres, and another for patients. The first survey was designed to evaluate the anticoagulation policies used at public and private HD centres. The patient survey analysed individual anticoagulation data from a randomly chosen 10-patient sample from each centre. The surveys were distributed and collected between May and September 2008.
The survey for dialysis centres collected information on the type of heparin used, dose and method of administration, and circuit priming. The survey also included a section on the criteria used for deciding whether to administer LMWH or UFH, with the following possible responses: 1) medical criteria (dyslipidemia, thrombocytopenia, etc.). 2) Dosing. 3) Cost. 4) Dialysis technique. 5) Vascular access. 6) Other. Finally, we asked for information on the adjustment methods used for dosing UFH and LMWH.
In addition to the questions regarding the anticoagulation methods used for each patient, the patient survey included questions on diagnosis of diabetes, haemoglobin levels, vascular access type, membrane type, dialysis technique, duration of HD sessions, and pump flow. We also asked if the patient was receiving additional anticoagulant and/or anti-platelet treatment, as well as whether any bleeding or thrombotic complications arose in the previous week.
We performed all statistical analyses using SPSS statistical software, version 15.0. We analysed qualitative variables using absolute frequencies and percentages, while quantitative variables were assessed using mean, standard deviation, median, minimum, and maximum. We applied tests of normality (Kolmogorov-Smirnov) and homoscedasticity (Levene) prior to applying parametric tests. We compared more than 2 groups using one-way ANOVA tests for normally distributed continuous variables, and Kruskal-Wallis tests for non-parametric variables. For comparisons of group means, we used Student’s t-tests in the case of normally distributed continuous variables, and Mann-Whitney U-tests for non-parametric variables. In the case of discreet variables, we used chi-square or Fisher’s exact tests when necessary. Following these comparisons, we selected those variables with a P-value <.100 for use in a logistic regression model. The level of statistical significance was set at 5%.
This study has been approved by the Spanish Society of Nephrology.
RESULTS
For a better comprehension of the results obtained, we have separated this section into two parts, corresponding to the data obtained in the surveys for haemodialysis centres and the data for patient surveys.
Haemodialysis Centre Survey
We compiled surveys from 89 haemodialysis centres throughout the country, constituting 29% of all such centres in Spain. Of these, 43 (48.3%) were public entities, and 46 (51.7%) were private. Of the 89 centres that responded to the survey, only 2 were paediatric units, and these were excluded from the general statistical analysis. The remaining 87 centres corresponded to adult patients, and at the moment the survey was taken, these centres treated a total of 6093 patients.
The data obtained from these 87 surveys are as follows:
1. Type of Heparin
The majority of the centres surveyed (61; 70.2%) utilised both types of heparin, 19 (21.8%) only administered LMWH, and 7 (8%) only used UFH. Although there was a certain tendency to use LMWH to a greater extent at public centres than private ones, this difference was not statistically significant (P=.073). The types of LMWH available at the 80 centres were: enoxaparin (60%), bemiparin (32.6%), nadroparin (21.3%), dalteparin (12.5%), and tinzaparin (11.3%).
2. Criteria Used for LMWH
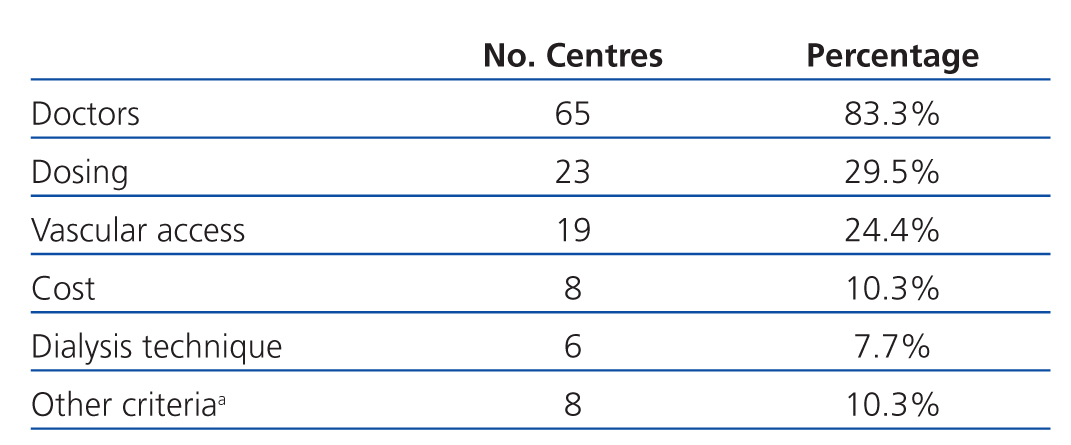
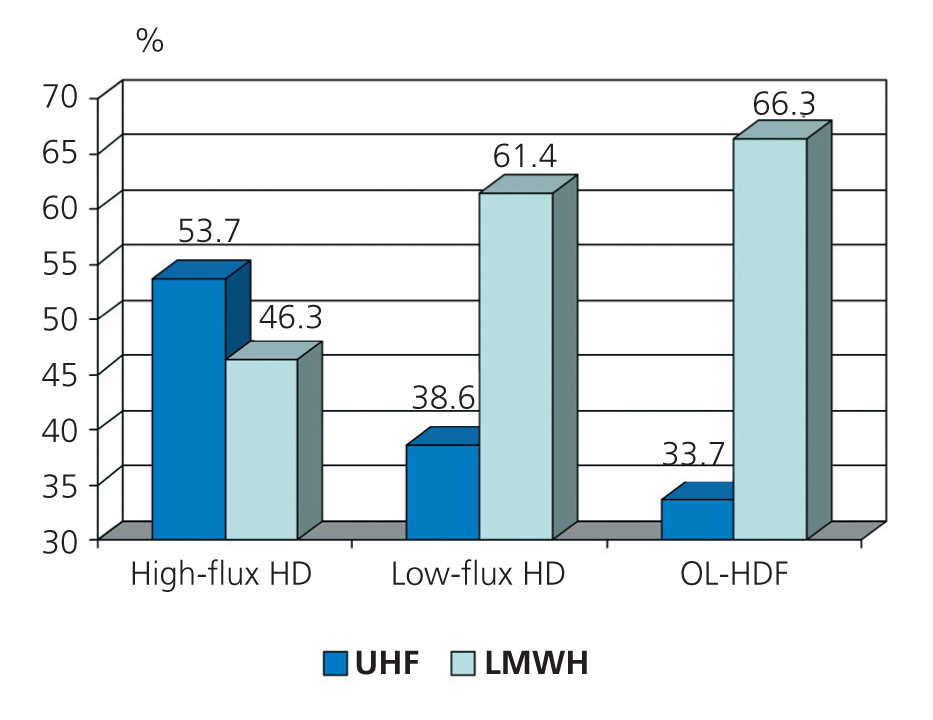
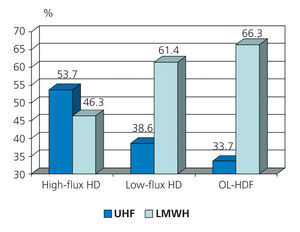
This was a multiple choice question, and the percentages for each response were calculated for the 78 centres that responded (Table 1).
3. Type of HD Priming
There is a wide variability in both the use of heparin priming and the dose used. We can summarise that:
-If UFH was used during HD (68 centres), the majority used UFH for priming (86.7%), 7.4% did not use heparin for priming, and 5.9% did so with or without heparin depending on the patient.
-If LMWH was used (73 centres), 21.9% of centres did not use heparin priming, 71.3% did so with heparin, and 6.8% either used or did not use heparin, depending on the patient.
The heparin dose used for priming ranged between 1000UI and 10 000UI. However, regardless of the type of heparin used in the HD session, the most commonly used dose was 5000UI (66% of centres when UFH was used, and 67.6% of centres when LMWH was used), followed by 2500UI (17% with UFH, and 16.2% with LMWH).
4. Dosing
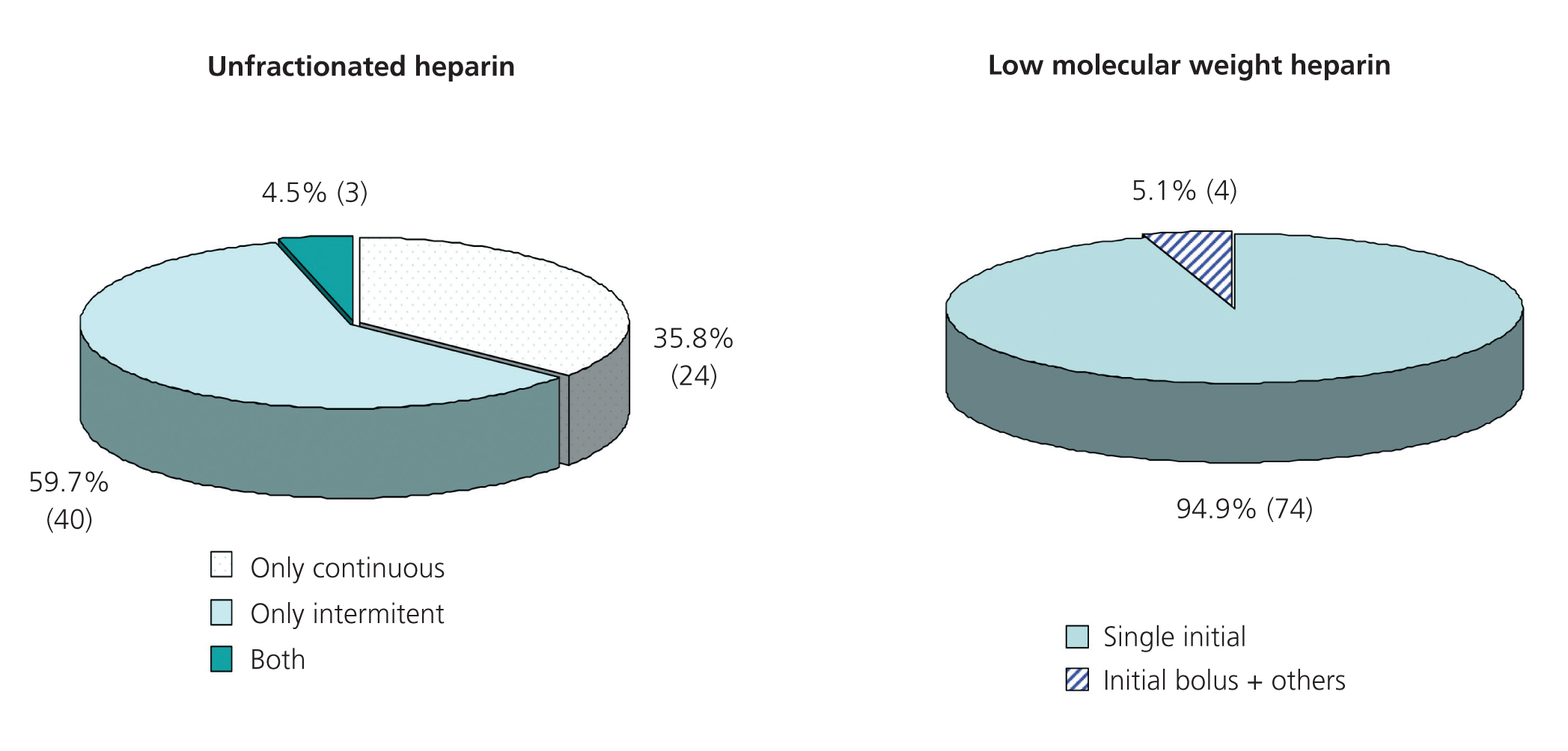
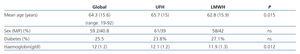
The methods of administration employed for heparin doses are summarised in Figure 1. Regardless of the method of administration for UFH throughout the HD session, the majority of centres used an initial bolus (92.6% when using a continuous dose, 97.6% when using an intermittent dose).
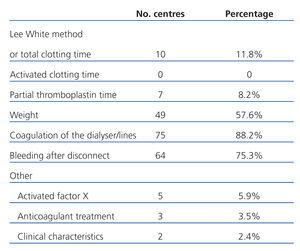
5. Adjustment Methods for the Heparin Dose
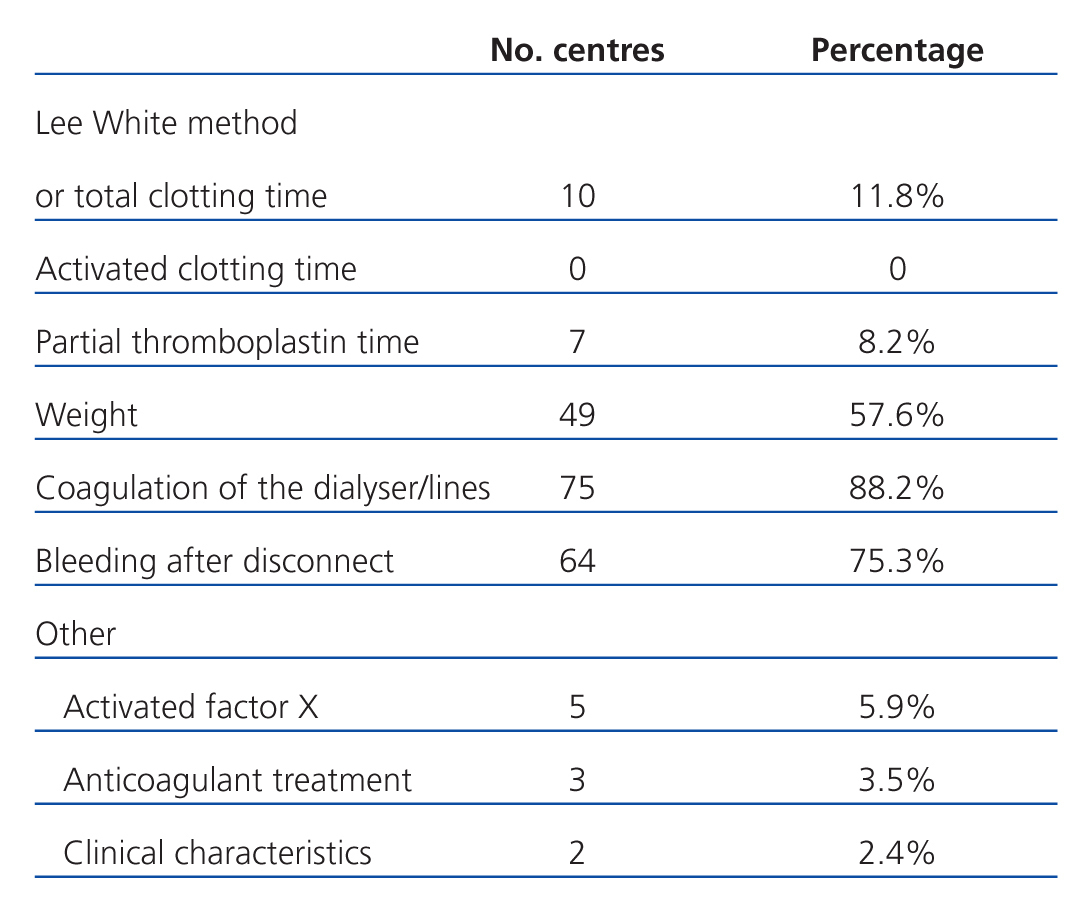
We received 85 responses for this section from the 87 surveys sent. As such, the percentages for this question were calculated over 85, and the results are summarised in Table 2. The general rule was that several factors were taken into account when adjusting the dose used. This was a multiple choice question that allowed us to assess the possible combination of factors in this context. Among these, the most common combinations used were: “weight + coagulation of the dialyser/lines + bleeding after disconnect” in 30 centres (35.3%) and “coagulation of the dialyser/lines + bleeding after disconnect” in 17 centres (20%), with all others being much less common.
Patient Survey
Of the 89 centres that responded to our surveys, 80 provided patient data, with a total of 770 patients surveyed. The general statistical analysis did not include 12 patients (10 due to non-compliance with the full range of questions asked at one centre, and 2 who were paediatric patients). In this manner, a total of 758 adult patients were included in the analysis from 78 different dialysis centres, of which 34 (43.6%) were public and 44 (56.4%) were private. The most important characteristics of these patients are summarised in Table 3.
The most relevant data obtained in the patient survey can be summarised as:
1. Anticoagulation in the Study Population
We obtained data on 733 patients, of which 323 (44.1%) received treatment with UFH, 378 (51.5%) with LMWH, and 32 (4.4%) received no anticoagulation during dialysis. At public centres, 64.2% of patients received LMWH, whereas 46.1% of patients received this type of heparin at private centres (statistically significant difference; P<.001).
The heparin dose was quantified in 291 patients, 186 of which received UFH and 105 received LMWH. The mean dose of UFH was 2988 (1706) UI (range: 500-9500UI, median: 3000UI) and the mean dose of LMWH was 3598 (1601) UI (range: 1000-8000UI, median: 3500UI).
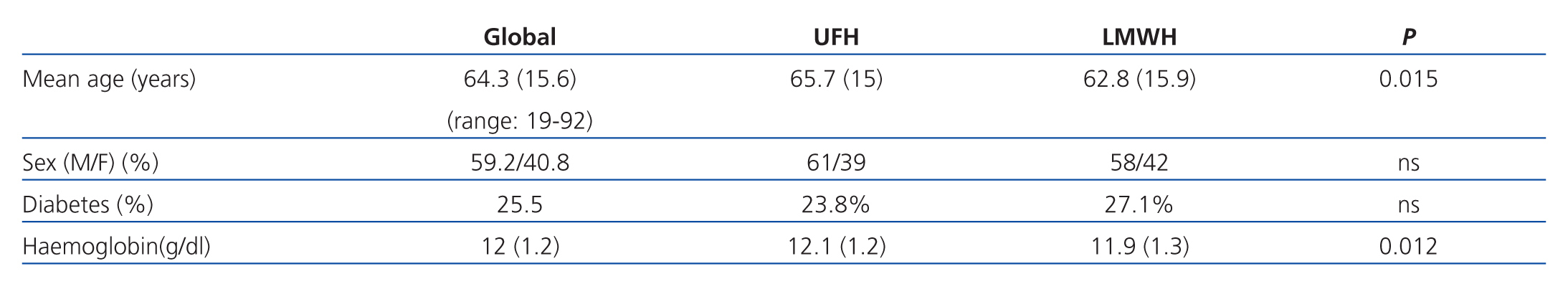
2. Anticoagulation According to Patient Characteristics
Upon analysis of patient characteristics based on the type of heparin used, we observed no differences in terms of sex or prevalence of diabetes. However, patients that received LMWH tended to be younger, and had lower haemoglobin levels (Table 3). There were no differences in the heparin doses prescribed (for both UFH and LMWH) in terms of age, sex, haemoglobin levels, or diagnosis of diabetes.
3. Anticoagulation According to Vascular Access
The distribution of vascular access types in the 758 patients that responded to this part of the survey was: autologous arteriovenous fistula (AVF): 68.5%, prosthesis: 7.8%, and catheter: 23.7%. There were no differences in terms of the distribution of the different types of vascular access between public and private centres. In patients with AVF, LMWH was utilised more frequently (56% vs 44%) whereas patients with prostheses were administered UFH more frequently (62% vs 38%) (P=.048). In patients with a catheter, the rates of using the two types of heparin were similar.
There were no differences in terms of the heparin doses prescribed (whether for UFH or LMWH) based on the type of vascular access used.
4. Anticoagulation According to the Technique and Membrane Type Used for Dialysis
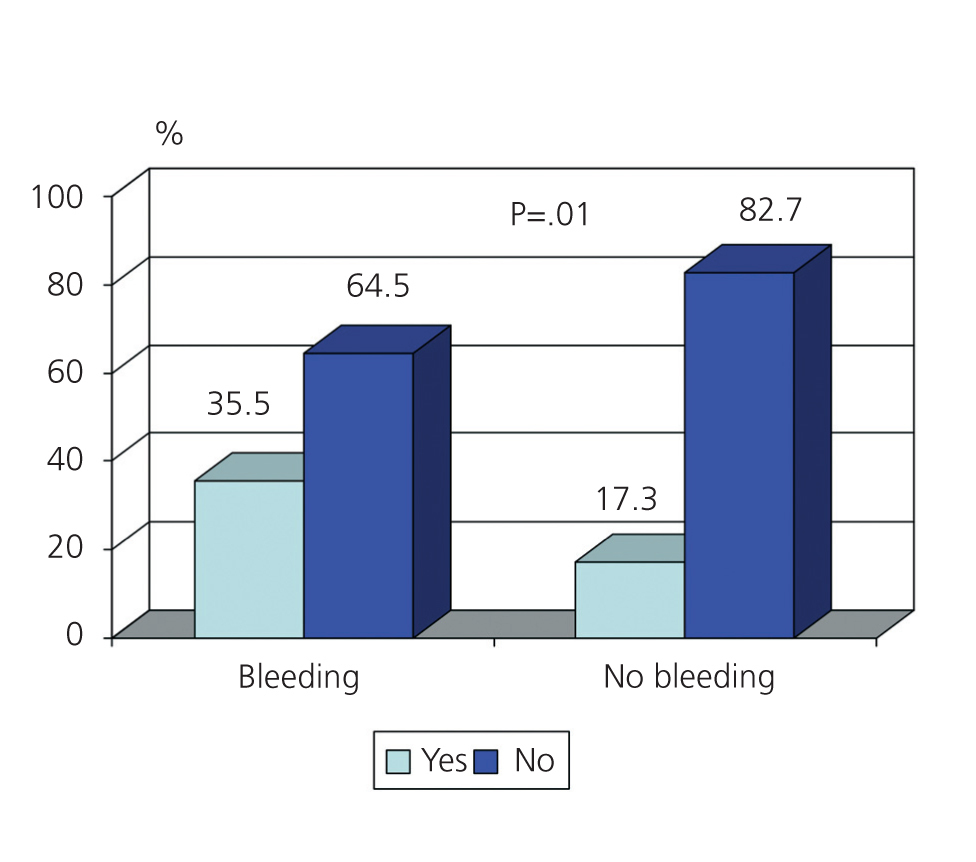
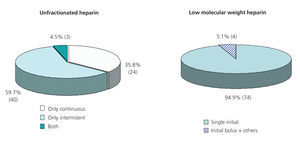
The dialysis technique used was recorded for 757 patients, of which 413 (54.6%) received high-flux HD, 249 (32.9%) received low-flux HD, and 95 (12.5%) received on-line haemodiafiltration (OL-HDF). At public centres, the distribution was: high-flux HD: 47.5%, low-flux HD: 30.7%, and OL-HDF: 21.7%, whereas at private centres, the distribution was 59.8%, 34.5%, and 5.7%, respectively (P=.001).
The distribution of the type of heparin used according to the dialysis technique used is represented in Figure 2.
The types of membranes used for dialysis were: cellulose: 6.1%, polysulfone: 59.5%, polyethersulfone: 12.2%, polyamide: 15.8%, AN69: 3.7%, and other: 2.7%. We observed no significant differences in terms of the type of membrane used between public and private centres. There were also no significant differences in the type of heparin administered (UFH vs LMWH) based on membrane type.
The heparin doses prescribed were similar regardless of the HD technique or membrane type used.
5. Anticoagulation According to Time on Dialysis and Pump Flow
The mean duration of HD sessions was 231 (26) minutes (range: 120-310 minutes), with the most common duration of sessions being 4:00-4:30 hours (n=440; 59.2%), followed by the interval of 3:30-4:00 hours (n=172; 23.1%), and >4:30 hours (n=63; 8.4%). There was no correlation between the type of heparin used and the duration of the HD session. As was expected, the dose of heparin prescribed was significantly lower in patients with shorter dialysis sessions (less than 4 hours) as compared to sessions lasting >4 hours, both when employing UFH (2443±1246UI vs 3264±1804UI; P=.003) and LMWH (2828±1234UI vs 3870±1630UI; P=.002).
Mean blood pump flow was 346 (47) ml/min (range: 150-500ml/min). Pump flow was significantly higher in the group that received UFH as compared to the group that received LMWH (351±42ml/min vs 339±51ml/min; P=.001).
6. Anticoagulation in Haemodialysis and Anti-platelet and/or Anticoagulant Treatment
We acquired survey responses regarding anti-platelet and/or oral anticoagulant treatment from 727 patients. Of these, 331 (45.5%) received anti-platelets, 134 (18.4%) received oral anticoagulants, and 36 (5%) received both. Overall, 425 (58.5%) received some type of anti-platelet and/or anticoagulant treatment.
The majority of patients that received oral anticoagulant treatment (n=115; 85.8%) also required heparin during HD. LMWH was used somewhat more frequently in these cases, although this difference was not statistically significant (LMWH: 56.4%; UFH: 43.6%). The UFH dose prescribed in patients that also received coumarin-type drugs was lower than in those that did not (2279±1499UI vs 3105±1721UI; P=.012), whereas no significant differences were observed in the doses prescribed for LMWH (3913±1768UI vs 3439±1486UI, respectively).
As regards priming, 77.9% of patients that received oral anticoagulants underwent heparin priming, with doses similar to those of other patients.
Patients receiving anti-platelet treatment had no differences from others in terms of the dose of heparin prescribed.
7. Anticoagulation and Bleeding Complications
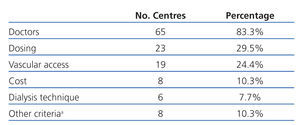
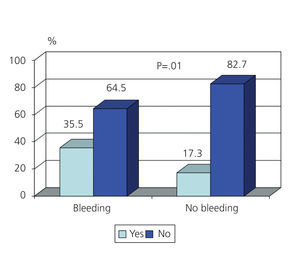
Of the 743 patients analysed in this section, 33 (4.4%) had experienced some type of bleeding complication within the previous week of filling out the survey. We observed no correlations between bleeding complications and age, sex, diabetes, or anti-platelet treatment. Patients with bleeding complications had significantly lower haemoglobin levels than patients that did not (10.9±1.4g/dl vs 12.1±1.2g/dl; P<.001), and received oral anticoagulation therapy more frequently (Figure 3). If we eliminate patients that received oral anticoagulants from the analysis, no significant differences were present in terms of the number of bleeding complications between patients receiving UFH and those receiving LMWH (P=.078).
8. Anticoagulation and Thrombotic Complications
Thrombotic complications in the week prior to taking the survey were reported in 14 of the 737 patients analysed (1.9%), with a greater frequency of occurrence in patients that received LMWH (P=.003). There were no significant differences in the dose of heparin prescribed, whether UFH or LMWH, between patients that experienced thrombotic complications and those that did not.
Finally, of the 2 paediatric centres asked to participate, 1 provided the surveys for 2 patients. Both received LMWH (enoxaparin), with heparin priming and high-flux HD using polysulfone.
DISCUSSION
Firstly, we would like to point out that both surveys can be considered valid for the analysis of our objectives. The number of centres, the geographic distribution of the various autonomous communities in Spain, the inclusion of both public and private centres, and the number of patients treated all lend strength to the haemodialysis centre survey. The patient survey was bolstered by the random selection of patients, lending similar characteristics to our sample as in other recent studies such as the Dopps III, which was considered representative of the adult Spanish population on dialysis.13 As such, the mean age, sex distribution, proportion of diabetic patients, mean haemoglobin values, and distribution of the different types of vascular accesses used are comparable between these studies.13
The primary objectives of our study were to assess the anticoagulation methods employed in Spain and what criteria they are based on. The near-50% distribution of the two types of heparin, despite the guideline recommendations that favour LMWH,12 indicate that, in clinical practice, there are additional criteria taken into account. Based on the type of data compiled, we cannot completely verify the reason for the lower frequency with which LMWH is used at private centres, even though availability was similar. The issue of costs could be an important factor; however, only 10% of centres indicated that cost was taken into account when deciding upon treatment. Whereas the greater costs of LMWH limited its use in the past, this currently does not appear to be an important limiting factor, with other criteria taking precedent in deciding upon whether to prescribe this drug.2
The risk of bleeding is the primary secondary side effect of anticoagulation therapy in HD. In our study, there was no association between bleeding complications and the type of heparin administered, which confirms previous observations that indicated a similar level of safety for both UFH and LMWH.6,7 We are not aware of the reason for the greater frequency of thrombotic complications observed in the group receiving LMWH. The possible reasons include a lower efficacy of this drug, inferior dosage adjustment, or the fact that LMWH was prescribed more frequently in complex patients with a greater tendency towards coagulability.
Medical criteria, followed by ease of administration, were the most commonly reported reasons for indicating LMWH. In addition to bleeding and thrombotic phenomena, dyslipidaemia,14 osteoporosis,15 and thrombocytopoenia16-19 are the most common side effects observed in the use of heparin in HD patients, and were surely considered within the medical criteria used to decide upon the prescription of LMWH in the patients included in our study. Several studies have demonstrated a lower increase in triglyceride levels in HD patients with LMWH than in those receiving UFH,8,9,14,20,21 although other studies did not corroborate with these findings.22-24 On the other hand, in patients without renal failure receiving prolonged treatment, the risk of developing osteoporosis is lower when utilising LMWH instead of UFH.15,25,26 In HD, LMWH has also been reported to cause osteoporosis at a lower rate than UFH,11,27 although no studies have clearly confirmed this phenomenon. Finally, in the population without renal failure, the incidence of thrombocytopenia induced by type II heparin is lower with LMWH than UFH,28,29 which has also been described in patients on HD.10
Both the survey for HD centres and the patient survey revealed that the type of vascular access was the third most common indication for employing LMWH. Although one study did show that the permeability of vascular accesses improves with the use of LMWH,30 to our knowledge, there are no studies that have shown any advantages from using a certain type of heparin over another when using autologous AVF or prosthesis.
The dialysis technique used was also one of the criteria employed for deciding whether to administer LMWH, which was prescribed at a greater rate than UFH in OL-HDF. On the other hand, the dose of LMWH was not significantly different when comparing between OL-HDF, low-flux HD, and high-flux HD. These data appear to contradict our understanding of the pharmacokinetics of LMWH during HD sessions. Several studies have shown that anti-Xa activity is significantly reduced in high-flux HD and convective techniques, as a consequence of the elimination of LMWH through the dialysate/ultrafiltrate. McMahon et al. showed that the anti-Xa activity in high-flux HD was lower than in low-flux HD when using the same dose of enoxaparin.31 Using continuous HD techniques, Isla et al. demonstrated significant enoxaparin losses in the ultrafiltrate/dialysate.32 Another study showed that anti-Xa activity at the end of the HD session was significantly lower on OL-HDF than low-flux HD.33 In any case, LMWH losses in dialysate are higher at the start of an HD session when administering boluses through the arterial branch of the HD system.10 For these reasons, in high-flux HD and even more so in HF and HDF techniques, some authors recommend administering LMWH at the start of the HD session in the venous branch of the extracorporeal blood circuit,10 or to administer it 3-4 minutes before starting dialysis.34 In our study, we did not analyse what type of administration was used (arterial or venous branch) or the moment of administration, since these questions were not included in the surveys.
As regards the type of material used in HD, platelet activation and coagulation varies according to the membrane used, such that the following sequence can be established based on these properties: unmodified cellulose membranes > unmodified AN69 > polysulfone > polyamide.35 In our study, we observed that the type of membrane used was not correlated with the type of heparin or dosage used in normal clinical practice. However, we must keep in mind that the majority of these patients were treated using synthetic membranes, primarily polysulfones/polyethersulfones.
It is interesting to point out that in patients receiving LMWH, the pump flow was significantly lower than in patients receiving UFH. Given that pump flow is directly related to heparin dose, these results should be interpreted taking into account that, given a higher risk of coagulation from a lower pump flow, LMWH tends to be used, probably with the goal of increasing efficacy, which would partly explain the greater incidence of thrombotic phenomena observed in this group.
Diabetes did not affect the use of heparin, neither type nor dose, which is in accordance with the current clinical mind-set that has rejected the antiquated and unproven idea that heparinisation in dialysis could increase the risk of ocular bleeding complications in these patients, which could worsen the prognosis of diabetic retinopathy.
The majority of dialyser producers recommend dialyser and circuit priming with saline solution and UFH, with the generally accepted standard dose of 5000UI, regardless of which type of heparin will be used in the HD session.36 However, in clinical practice, a significant percentage of HD centres in Spain do not employ heparin priming, especially when LMWH is used as an anticoagulant. Some next generation HD machines allow for priming with the dialysate fluid itself, removing the need for heparin, which reduces costs and simplifies the procedure. In the survey for HD centres, the dose used for heparin priming varied widely, which implies great heterogeneity in the anticoagulation practices within our country.
The surveys clearly show that dosing adjustments are for the most part made through trial and error, and that methods for measuring coagulation states in patients are rarely used. Due to the design of the survey, we do not know the reason for which 5.9% of centres determined an anti-Xa factor for adjusting LMWH dose. One of the possible indications is pre-HD measurements in patients with a daily dialysis regimen, where there is an evident risk of accumulation.35
In our study, we observed that over half of all patients on HD were also receiving treatment with oral anticoagulants and/or anti-platelets. Few previous studies have analysed this factor in prevalent HD patients. In the DOPPS study, approximately 30% of patients on dialysis took aspirin.37 In another analysis from one single centre, 25% of patients were receiving oral anticoagulants.38 An American study involving 41 425 incident patients on HD showed that 8.3% received warfarin, 10% clopidogrel, and 30.4% aspirin, and that the risk of death and hospitalisation from bleeding was greater in patients that received warfarin and clopidogrel, but not aspirin.39 Elliott et al.,40 in a systematic review of 28 publications, concluded that warfarin doubled the risk of severe bleeding in HD patients. These results coincide in part with our own, where there was a correlation between the appearance of bleeding complications and treatment with oral anticoagulants, and not with anti-platelets, although we do not know what proportion of patients were receiving aspirin or other anti-platelets.
The results from our surveys show that the majority of patients receiving oral anticoagulants required heparin during the dialysis session, which coincides with previous observations.41 With this in mind, we can make the general inference that oral anticoagulation is insufficient for preventing system coagulations in HD. Even so, our study produced the striking result that, while patients with oral anticoagulation had UFH prescriptions that were adjusted to lower amounts, this did not occur when LMWH was used, and these doses were not different between the two groups of patients.
As a final conclusion, there is a lack of general accordance in terms of which aspects are important for anticoagulation in patients on HD, such as which type of heparin to use (UFH vs LMWH), the type of administration for UFH (continuous or intermittent), the use of heparin and doses for priming, the methods for adjusting dosage, and the type of heparin to use based on the dialysis technique. As such, there is a notorious disparity in the criteria used in general daily practice for prescribing anticoagulation treatment in patients on HD, which necessitates a review of the results produced at each centre and on the national level, and possibly the creation of a guideline for anticoagulation in haemodialysis.
ACKNOWLEDGEMENTS
The task force received the valuable collaboration of Laboratorios Farmacéuticos Rovi S.A., who provided consistent technical support in the structuring and the surveys’ printing.
Conflicts of Interest
The authors have no conflicts of interest to declare.
Table 1. HD centre survey. Criteria for the use of LMWH vs UFH
Table 2. HD centre survey. Dose adjustment methods
Table 3. Patient survey. Baseline characteristics. Type of heparin administered according to age, sex, diabetes, and haemoglobin levels
Figure 1. HD centre survey. Heparin dosing
Figure 2. Patient survey. Type of heparin administered according to the haemodialysis technique employed
Figure 3. Patient survey. Treatment with oral anticoagulants in patients with and without bleeding complications in the previous week