La incidencia de ictus es mayor entre los pacientes en hemodiálisis (HD) que en la población general. En este estudio observacional se analizaron los datos de los pacientes incidentes en HD en el Hospital Universitario Marqués de Valdecilla de Santander (España), durante un período de 40 años (1971-2011). El número total de pacientes que iniciaron hemodiálisis fue de 1453. El período total de seguimiento fue de 4982,22 pacientes/año. Ochenta y cuatro pacientes sufrieron un accidente cerebrovascular. La incidencia acumulada de accidentes cerebrovasculares fue de 5,8 %, con una tasa de incidencia de 1686 ictus por 100 000 pacientes-año. La tasa de incidencia en el primer año en HD fue de 1803 ictus por cada 100 000 pacientes-año, un 6,5 % superior a la media observada a lo largo de todo el período estudiado. En el resto del período, las tasas oscilaron entre 356 y 1626 ictus por cada 100 000 pacientes-año. Factores significativos relacionados con la aparición de ictus fueron: diabetes, infarto de miocardio o angina de pecho, hipertensión, arteriosclerosis/claudicación intermitente, antecedentes de accidente cerebrovascular antes de la HD y fibrilación auricular. Los niveles de hemoglobina en el grupo con ictus fueron prácticamente idénticos a los de la cohorte no ictus (11,92 ± 2,07 g/dl, en comparación con 11,68 ± 2,12 g/dl). Por último, el 60,7 % de la población ictus recibió eritropoyetina con dosis media de 9611 UI/semana, en comparación con el 51,9 % y una dosis de 9544 UI/semana en la cohorte no ictus, sin diferencias significativas entre los grupos. En conclusión, en la población en HD la incidencia de ictus es 7-10 veces superior a la población general y se asocia a factores tradicionales, pero no con niveles de hemoglobina ni dosis de eritropoyetina.
The incidence of stroke is higher substantially among hemodialysis patients than in the overall population. In this observational cohort study, we analysed data from incident hemodialysis patients at Valdecilla University Hospital in Santander (Spain) during a 40-year period (1971-2011). A total number of 1453 patients were started on hemodialysis The total follow-up period was 4982.22 patients/year, with 84 patients having stroke. The cumulative incidence of stroke in our patients was 5.8%, with an incidence rate of 1686 strokes per 100 000 patient-years. The incidence rate in the first year was 1803 strokes per 100 000 patients-year, 6.5% higher than its average over the period studied. In the remaining period, the rates ranged between 356 and 1626 strokes per 100 000 patients-year. Significative factors related to stroke were: diabetes, myocardial infarction or angina, hypertension, arteriosclerosis/intermittent claudication, history of stroke before the HD and atrial fibrillation. Haemoglobin levels in the cohort stroke were virtually identical to those of the not stroke cohort (11.92±2.07g/dL, compared to 11, 68±2.12g/dL). Finally, 60.7% of the population of the stroke cohort received erythropoietin with mean dose of 9611IU/week, compared to 51.9% and a dose of 9544IU/week in the not stroke cohort, without significative differences among groups. In conclusion, in haemodialysis population the incidence of stroke is 7-10 times higher than in the general population. It is associated with well known factors for stroke but not with haemoglobin levels or erythropoietin dose.
INTRODUCTION
It is known that the decline of renal function is significantly associated with a high cardiovascular risk and that cardiovascular complications1-6 in dialysis patients are the cause of mortality in half of cases7.
Among cardiovascular complications, stroke has been analysed in haemodialysis (HD) patients, although studies do not allow adequate measurement of the incidence rates due to the methodological differences of their design, in the analysed parameters or in the study population, such as: age, previous comorbidities, ethnicity and duration of follow-up. The studies by Sanchez et al8. and Power et al9. analysed the occurrence of strokes in populations on HD and in their respective groups. For the periods analysed they indicated incidence rates of 2410/100 000 patient-years (only ischaemic stroke) and 1730/100 000 patient-years, respectively. The most recent results on stroke incidence in the overall population in Spain are compiled in the IBERICTUS study10. Their conclusions laid down incidence rates standardised to the European population as to 2006 of 176 cerebrovascular events (confidence interval [CI] 95 %: 169-182) for 100,000 residents. This means that the incidence in patients on HD is at least 10 times higher than that of the general population.
The risk factors that have been considered in the case of stroke in patients on dialysis are essentially similar to those evaluated in the general population. However, there are some factors in HD patients that have been associated to their risk of stroke: level of haemoglobin (Hb) and/or dose of erythropoietin (Pfeffer et al.) or simply the start of HD (Murray et al.).11,12
The aim of this study is to analyse the incidence of strokes in our HD population over 40 years (November 1971 – November 2011), the factors associated with the appearance of strokes with special attention to Hb levels and erythropoietin doses, and also to evaluate the time of appearance in relation to the start of HD.
MATERIAL AND METHOD
Retrospective observational study of patients from the inpatient and outpatient HD unit of the University Valdecilla Hospital in Santander (Spain) between November 1971 and November 2011. The follow-up period for each patient covers from their HD start date until its termination due to death, transplant, change to peritoneal dialysis, transfer to other centre or closing of the study.
Stroke diagnosis in the database was obtained from the following diagnoses: transitory ischaemic attack (TIA), acute cerebrovascular accident (CVA), hemiparesis, hemiplegia, brain haemorrhage, stroke, embolic stroke of the middle cerebral artery, ischaemic infarction in the left frontal operculum, lacunar infarction, multiple lacunar infarctions with pseudobulbar dysarthria or cerebral ischaemia.
A total of 1453 patients were included in the study. The total follow-up period was 4982.22 patients-year, which represents an average follow-up period of 3.43 ± 4.65 patients-year.
The following variables were analysed: demographic data, previous history of cerebrovascular events, diabetes diagnosis at the start of HD, previous history of ischaemic disease (currently presenting angina, previous myocardial infarction, coronary intervention and/or bypass grafting), hypertension, atrial fibrillation, advanced peripheral arterial disease, type of vascular access, Hb levels and weekly dose of erythropoiesis-stimulating agents (ESA) for those patients who have them prescribed.
For the analysis of results, the population was divided into two cohorts: STROKE cohort (n = 84) and NOT STROKE cohort (n = 1369). The levels of Hb and ESA calculated in the stroke cohort correspond to the average from the three months prior to the occurrence of the stroke. In the NOT STROKE cohort, these parameters correspond to the mean of the whole observation period (Hb1 and ESA1). With the aim of comparing these indices more closely, we obtained the means of Hb and ESA dose (Hb2 and ESA2) that the patients presented three months before the mean time of the stroke’s appearance in the stroke cohort (5.15 years).
The statistical analysis was carried out using SPSS software, version 17 (SPSS Inc., Chicago). A P value of <.05 was considered to be statistically significant. The quantitative variables were presented as mean and standard deviation and the qualitative variables as number and percentage. The comparison between groups was carried out using the Student t-test or χ2 according to the type of variable. The curves for incidence of stroke were estimated using the Kaplan-Meier method.
RESULTS
Incidence
The cumulative incidence of cases of strokes among our patients was 5.8 % for a total follow-up period of 4982.22 patients-year, which implies an incidence rate of 1686 strokes per 100,000 patients-year. The population distribution by sex was: males 65.7 % and females 34.3 %. In the stroke cohort, the distribution by sex was: males 59.5 % and females 40.5 %. The mean period on HD of the general population was 3.43 ± 5.65 years, although the stroke cohort was on HD for a mean period of 5.53 ± 5.71 years.
Without taking into consideration the cases of TIA, the stroke distribution was 66.67 % ischaemic and 33.33 % haemorrhagic. This implies an increase of the latter in HD with respect to the general population10, in which the ischaemic/haemorrhagic relation is 80 % vs. 20 %.
Associated factors
The previous comorbidities analysed in the STROKE cohort showed a higher relevance than that of the NOT STROKE cohort: diabetes 36.9 % vs. 21.2 %, infarction or angina 30.9 % vs. 16.2 %, hypertension 82.1 % vs. 52.8 %, arteriosclerosis/intermittent claudication 16.6 % vs. 6.4 %, history of stroke prior to HD 16.6 % vs. 5.9 %, atrial fibrillation 8.3 % vs. 4.1 % and use of warfarin 11.9 % vs. 1.7 %.
Of the STROKE cohort subjects, 61.9 % used internal arteriovenous fistulae (IAVF) and 38.1 % used a catheter; meanwhile in the NOT STROKE cohort, there was a distribution of 51.2 % and 48.7 %, respectively. Therefore, no significant differences were observed in the type of vascular access (AVF or catheter).
The distribution of treatment between the STROKE and NOT STROKE cohorts was as follows: darbepoietin: 47 % vs. 64 %; EPO alfa: 37 % vs. 24 %; CERA: 10 % vs. 7 %, EPO beta: 6 % vs. 4 %.
Hb levels in the STROKE cohort were almost the same as those in the NOT STROKE cohort (11.92 ± 2.07g/dl vs. 11.68 ± 2.12g/dl), with no significant differences. 60.7 % of the stroke cohort population received a prescription of ESA, with an average dose of 9611IU/week, compared to 51.9 % and a dose of 9544IU/week in the NOT STROKE cohort, with no significant differences in dosage between both groups (Table 1).
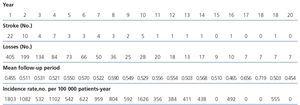
We did not observe special incidence rates during the first year, as other studies indicate. During the first year on HD, the incidence rate was 1803 strokes per 100 000 patient-years, a rate 6.5 % higher than the mean observed in the studied period. Table 2 and Figure 1 show the annual incidence rates throughout the first 20 years of the analysed period.
In Figure 2, the graph of the Kaplan-Meier curve can be seen, with respect to stroke-free survival throughout the evolution on HD.
DISCUSSION
In the cohort of patients on HD studied, the incidence of strokes, higher than in the general population, is associated with known cardiovascular risk factors, is independent to Hb levels and erythropoietin dose, and we did not find the precocity in the appearance of strokes following the start of HD that others have observed.
Our study shows an incidence rate of 1,686 strokes per 100 000 patients-year, which means an increase of 7-10 times with respect to the overall Spanish population10. This incidence is coherent with the majority of the studies analysed8,9,12,13, bearing in mind that the incidence of strokes has been associated, among others, with non-modifiable factors such as age, sex, race and geographical location.
We identified the following as risk factors for strokes: diabetes mellitus, arterial hypertension, history of stroke and previous cardiovascular disease. The increase of risk in patients treated with warfarin, also observed in other studies,14 should be interpreted with caution. It could be attributed to previous comorbidities that favour the appearance of strokes. However, there are some discrepancies over the importance of certain risk factors in the development of strokes in HD patients. Some studies13,15,16 indicate the following as possible risk factors for strokes: alcohol or tobacco consumption, dyslipidaemia, body mass index, CRP, transferrin saturation, glycated Hb, protein-to-creatinine ratio in the urine, serum albumin, treatment with vitamin K antagonists, antiaggregants, insulin or oral hypoglycaemic drugs and type of vascular access. Seliger et al17. indicate routine administration of heparin during HD as a possible cause of the increase of haemorrhagic strokes. On the contrary, other studies8,13 rule out the relation between some of these factors (tobacco, dyslipidaemia and serum albumin) and strokes.
Currently one of the most significant controversies, particularly from the TREAT study, is the involvement of the Hb value and/or the dose of erythropoietin in the appearance of strokes in HD patients. The TREAT11 study concluded that the use of darbepoietin alfa in diabetic patients with chronic kidney disease, not on dialysis and with moderate anaemia did not reduce the risk of death or appearance of cardiovascular or renal events, although it constituted a significant increase in the risk of strokes (hazard ratio of 1.92 95 % CI [1.38-2.68] P<.001). The univariate analysis of baseline variables in the population studied was not statistically significant in any of the cases, except that related to the use of ESA. However, post hoc studies to TREAT, such as that of Skali et al.18, concluded that a high number of stroke episodes (x2) with darbepoietin alfa in the TREAT study could not be attributed to any baseline characteristic or to differences post-randomisation in arterial pressure, Hb, platelet count or erythropoietin dose, which coincides with our results. In addition, in their nested case-control study, relation between the history of cardiovascular events and previous stroke and the occurrence of new stroke, which once again corroborates our findings, could be observed among the cases (stroke in the treatment arm).
An interesting aspect is the time of stroke appearance in incident patients on HD. In Spain, in the study by Sánchez Perales et al8, conducted on 449 incident patients on dialysis, the incidence of strokes during the first three years on dialysis was 2.4 per 100 patients-year, but there is no incidence data during the first year. Murray et al12. observed in both inpatients and outpatients that the number of strokes in the first month of HD increased its incidence by up to seven times. The reasons for this incidence increase in the first stages of HD are not clear, indicating as possible factors the decrease of cerebral perfusion and the rate of blood flow or19,20, in patients treated with ESA, the increase of the viscosity and the vascular resistance that could cause increases in blood pressure. This precocity and the factors related to the start of HD should be clarified with new data. However, we have not found such precocity and the appearance of strokes in our patients is not associated to the time of dialysis treatment. Consequently, the incidence in the first year was 1803 strokes per 100 000 patients-year and in successive years, apart from exceptions of absence of stroke in some patients, the incidence varied between 356 and 1626 strokes per 100 000 patients-year. The difference with Murray et al.’s study12 is that the number of diabetic patients was greater than in their study (around 53 %) and that it involved patients of a higher mean age (≥ 67 years). Despite the fact that in our series, as we have commented, this immediate precocity of the appearance of strokes following the start of HD was not seen, studies that clarify this difference with our results are necessary. These studies could shed light on aspects to be considered for improved stroke prevention, such as dialysis techniques, blood and dialysate flow, duration and frequency of sessions during the first month of treatment, anticoagulation techniques, etc.
The mean age at the start of HD was 61.89 ± 13.97 years in the STROKE cohort, compared to 58.07 ± 16.49 years in the NOT STROKE cohort. This reflects that, as was the case in the overall population, in undergoing HD the incidence of stroke increased with age10.
In our series, the mean period on HD of the general population was 3.43 ± 5.65 years, although the STROKE cohort was on HD for a mean period of 5.53 ± 5.71 years. The logical explanation for this is that one of the reasons for leaving the study is renal transplant, which obviously is higher in patients with less vascular comorbidity.
The strength of this study is fundamentally based on the fact that it belongs to one centre and on that the observation time is 40 years. Its weakness is that it is a retrospective observational study and that the small number of strokes throughout the evolution hinders a study based on propensity match score.
In summary, the incidence of strokes in HD patients is 7-10 times higher than in the general population. We found as risk factors for strokes in patients on HD: older age, diabetes, cardiovascular disease, arterial hypertension and history of stroke prior to starting HD. We did not find levels of Hb or elevated dose of ESA as factors associated with strokes. Contrary to other studies, we did not detect precocity in the appearance of strokes at the start of HD.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 2. Annual rates of the incidence of strokes.
Table 1. Summary of factors associated with strokes.
Figure 1. Evolution of the annual rate of incidence of strokes.
Figure 2. Kaplan-Meier Curve. Stroke-free survival throughout the haemodialysis period.