La mucormicosis rino-órbito-cerebral es una infección micótica potencialmente mortal en los pacientes inmunosuprimidos. Los principales factores de riesgo para adquirirla son la diabetes mellitus mal controlada, la sobrecarga de hierro, la inmunosupresión potente y el uso crónico de esteroides. En esta revisión presentamos el caso de un paciente trasplantado de riñón que, luego del tratamiento de un rechazo agudo con dosis altas de esteroides e inmunosupresión potente con tacrolimus más micofenolato, presentó mucormicosis rino-órbito-cerebral de rápida progresión con necesidad de tratamiento quirúrgico agresivo, suspensión de la inmunosupresión y tratamiento antifúngico potente.
Rhino-orbital-cerebral mucormycosis is a potentially fatal mycotic infection in immunosuppressed patients. The main risk factors for acquiring this infection are poorly controlled diabetes mellitus, iron overload, potent immunosuppression and chronic steroid use. In this review, we present the case of a kidney transplant patient who, after treatment of an acute rejection episode with high doses of steroids and potent immunosuppression with tacrolimus and mycophenolate, presented with rapidly progressing rhino-orbital-cerebral mucormycosis that required aggressive surgical treatment, immunosuppression discontinuation and potent antifungal treatment.
INTRODUCTION
Rhino-orbital-cerebral mucormycosis (ROCM) is a rapidly progressing mycotic infection and is associated with high morbidity and mortality in immunosuppressed patients, with the requirement for multidisciplinary medical and surgical management. We present the case of a kidney transplant patient with ROCM that was managed successfully in our institution.
CASE STUDY
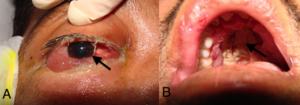
A 33-year-old male patient, with a history of end-stage renal disease secondary to polycystic disease. He received a transplant from a deceased donor in another institution in 2007. He received immunosuppression with prednisone, tacrolimus and mycophenolate mofetil. In March 2012, a renal biopsy was performed, which showed Banff IA acute cellular rejection. He received treatment with 1500mg methylprednisolone, 50mg/day prednisone, 3000mg/day mycophenolate and 7mg/day tacrolimus XL. A month later, the patient had a fever and frontal and retro-ocular headache, with decreased sensitivity in the right side of his face. He was assessed and diagnosed with acute sinusitis and was started on treatment with amoxicillin. The patient did not improve and began to display eye proptosis, upper right maxillary oedema, greenish rhinorrhoea, diplopia, epiphora, ulcerations on the palate, seizures and an increase in nitrogen compounds. He was therefore transferred to our institution. On admission, he was febrile, with oedema in the right side of the face, extensive ulcerations in the hard palate, eye proptosis, ophthalmoplegia, loss of vision in the right eye and impaired renal function (Figure 1). We performed a MRI of the brain, which showed involvement of the paranasal sinus, the right orbit, the frontal lobe, cavernous sinuses, right basal ganglia and the ipsilateral thalamus area (Figure 2). On the basis of these findings, we diagnosed the patient with ROCM, and as such, we started treatment with liposomal amphotericin B, we discontinued immunosuppression and the patient underwent multidisciplinary radical surgery in which the surgeons carried out sinusitis drainage, right frontal cerebral abscess drainage, extensive resection of soft tissue and bone in the right side of the face, enucleation, tracheostomy and gastrostomy (Figure 3). The cultivations and pathology confirmed infection by Mucor (Figure 4). E. cloacae, C. sedlakii and ESBL (extended-spectrum beta-lactamase) positive K pneumoniae.
An MRI showed that there was still brain involvement due to the disease. However, given the area involved and serious consequences of more radical surgery, we decided to continue with medical management (Figure 5). As such, after the radical surgery, the patient completed his treatment over 6 weeks with liposomal amphotericin B, meropenem, linezolid and posaconazole, in addition to having his wounds treated twice a week. He was then discharged with a prescription of 400mg posaconazole every 12 hours, 50mg ciclosporin every 12 hours, 5mg prednisone per day and nutrition by gastrostomy. Six months later, the patient was in good general condition, without signs of active infection and with acceptable renal graft function (creatinine of 1.5mg/dl). He underwent successful reconstructive surgery. Six months after reconstruction, the patient was in a good general condition and is currently on a plan to complete his facial reconstruction process (Figure 6).
DISCUSSION
Mucormycosis is an opportunistic and devastating mycotic infection caused by various types of filamentous fungi that are widely distributed all over the world. It is currently considered to be the third most common invasive mycosis after candidiasis and aspergillosis,1 although in kidney transplant patients, it was reported as the main cause.2,3 The prevalence of mucormycosis is around 3%-4% in autopsy records of high risk patients and its incidence has increased in recent decades in relation to the wider availability and use of immunosuppressant drugs for various therapeutic indications and also because of the great pandemic caused by metabolic diseases, such as diabetes mellitus.1,4
The fungi responsible for mucormycosis belong to the Zygomycete class, of the Mucorales order, represented by various genera, including Mucor, Rhizopus, Rhizomucor and Absidia.4 These fungi are characterised by rapid growth in undemanding culture media, at a wide range of temperatures, with an asexual reproduction process and the production of spores that are released into the environment. Under the microscope, they can be distinguished by their wide, aseptate hyphae (5-15 micras) with irregular branching.4-6
Of all clinical forms, ROCM is the most common in kidney transplant patients.3 It is usually caused by the fungus Rhizopus oryzae and is characterised by acute sinusitis with fever, headaches, epiphora and nasal congestion,5,9 with a generally rapid progression through vascular dissemination to adjacent structures and it can reach the brain parenchyma.9 Clinical predictors for dissemination of the disease mainly include palate ulceration, necrotic tissue and nasal turbinate involvement.7,9
The risk of developing a ROCM mainly depends on factors related to the susceptibility of the host in relation to their cellular immunity. The main risk factors in the transplant population are poorly controlled diabetes mellitus, iron overload, uraemia, broad spectrum antibiotic use, episodes of acute rejection, steroid use and potent immunosuppression.4,5,7,9-11
Mucormycosis diagnosis will always require histological confirmation, since imaging studies may suggest involvement due to this infection but they do not offer a diagnosis.12 However, given the magnitude of involvement, the rapid progression of local invasion and the implications that threaten the patient’s life, a high degree of suspicion is necessary and in the appropriate clinical context, early medical and surgical management would be indicated even without histological confirmation.4,9,13
The approach to treating ROCM is based on four key principles. Firstly, there should be early diagnosis based on a high degree of suspicion. Secondly, early initiation of treatment, both medical and surgical, ideally in the first 5 days, has demonstrated a lower mortality rate after 3 months (48.6% vs. 82.9%).7,14,15 Thirdly, it is important to try and eliminate the predisposing factor, particularly glucocorticoid use, which should be minimised or ideally discontinued.7,14,15 Fourthly, the most important element of ROCM management is extensive surgical debridement of the tissue involved, in order to cut off the link between angioinvasion, necrosis and poor penetration of the drug to the infected site.4,15 Antifungal therapy generally involves administration of polyenes such as amphotericin B in its deoxycholate or liposomal forms, in combination with posaconazole.4 The duration of medical treatment should be individualised for clinical and radiological resolution.16 However, it must be borne in mind that even in the best of circumstances and despite proper management, mortality due to this infection is around 45% in the local form, but can reach 93% in the rhinocerebral form.9,17
When the patient came to our hospital, he had an advanced infection, with extensive paranasal sinus, orbit and brain involvement. Multidisciplinary medical and surgical management allowed this infection to be successfully treated, although with major aesthetic and functional consequences.
In conclusion, mucormycosis should be suspected in all immunosuppressed patients who present with persistent upper respiratory symptoms not explained by other causes, and treatment should be aggressive and should include antifungal therapy and early surgery in order to avoid complications and progression to ROCM, which has a high morbidity and mortality rate, with devastating consequences.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Figure 1. Initial findings at diagnosis.
Figure 2. Findings in the MRI of the brain.
Figure 3. Postsurgical findings.
Figure 4. Histological findings.
Figure 5. Postsurgical MRI of the brain.
Figure 6. Patient six months after reconstruction.