La enfermedad renal crónica (ERC) y las complicaciones que de ella se derivan se han convertido en un importante problema sanitario, tanto por los recursos que se requieren en los estadios finales de la enfermedad como por las complicaciones secundarias que conlleva, por lo que su diagnóstico precoz es considerado hoy de gran importancia. Las guías KDIGO 2013 recientemente publicadas basan la definición y clasificación de la ERC en los valores de filtrado glomerular y albuminuria como criterios de estadiaje y marcadores pronóstico de la enfermedad. Las ecuaciones MDRD y MDRD-IDMS (cuando se utilizan valores de creatinina obtenidos por métodos con trazabilidad al método de referencia) son las más utilizadas, pero tanto las guías internacionales KDIGO 2013 como el nuevo documento de consenso sobre la ERC 2013, en el que han participado diez sociedades científicas bajo la dirección de la Sociedad Española de Nefrología, recomiendan su sustitución por la ecuación CKD-EPI. Nuestro objetivo ha sido, tal y como hicimos con ecuaciones previas, elaborar unas tablas que permitan conocer el valor del filtrado glomerular estimado mediante la ecuación CKD-EPI a partir de la concentración sérica de creatinina, la edad y el sexo, y de este modo proporcionar un instrumento que facilite la difusión de esta nueva ecuación, especialmente en ámbitos en los que no se calcule de modo automático.
Chronic kidney disease (CKD) and its complications have become a major healthcare problem, both due to the resources that are required in the final stages of the disease and to secondary complications. As such, its early diagnosis is considered to be very important nowadays. The recently published 2013 KDIGO guidelines base the definition and classification of CKD on glomerular filtration values and albuminuria as staging criteria and prognostic markers of the disease. The MDRD and MDRD-IDMS equations (when creatinine values can be traced to the reference method) are those most used, but both the 2013 KDIGO international guidelines and the new 2013 CKD consensus document, in which ten scientific societies participated under the direction of the Spanish Society of Nephrology, recommend to be replaced by the CKD-EPI equation. Our objective has been, as with previous equations, to develop tables that display the estimated glomerular filtration rate value using the CKD-EPI equation from serum creatinine concentration, age and sex, and thereby provide an instrument that facilitates the dissemination of this new equation, particularly in settings where it is not calculated automatically.
INTRODUCTION
Chronic kidney disease (CKD) is a major healthcare problem, as has been stated in different epidemiological studies,1-3 not only because patients who reach end-stage ESRD require many healthcare resources, but also due to the high cardiovascular disease burden, hospitalisation and premature death inherent in its diagnosis.4
With the aim of preventing or delaying complications associated with CKD,5 in 2002, the American National Kidney Foundation (NKF) Kidney Disease Outcome Quality Initiative (K/DOQI) published clinical guidelines to define and classify it into different stages.6 In 2005, the Kidney Disease: Improving Global Outcomes (KDIGO) international initiative accepted the definition and classification initially proposed by the K/DOQI7 with minor modifications, and in January 2013, it published guidelines on the diagnosis, classification and management of CKD that confirm the previous definition of CKD and classify it into stages based on glomerular filtration rate (GFR) values and the degree of albuminuria.8
In recent years, GFR has been considered the best index for assessing renal function. Given that it is not feasible to measure it in daily practice, various equations have been developed that allow its estimation from serum creatinine concentration, age, sex and race. However, other renal lesion markers have been required to define CKD when the GFR is >60ml/min/1.73m2 (albuminuria, haematuria, abnormalities in imaging tests, etc.), fundamentally due to the imprecision and inaccuracy of estimated glomerular filtration rate (eGFR) equations, especially for higher values.6-8 Although many equations have been published, the most used in our country are those of the Modification of Diet in Renal Disease9 study, whether in its classical version MDRD-410 or IDMS-MDRD, according to whether the serum creatinine method is traceable with respect to the isotopic dilution mass spectrometry (IDMS)11 reference measuring procedure. These equations also have been used to assess CKD prevalence in epidemiology and public health studies.12,13
The Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) is a research group dependent on the National Institute of Diabetes and Digestive and Kidney Disease which has been set up to develop equations to estimate the GFR using data from different studies. In 2009, this group published a new equation using standardised creatinine methods, obtained from a population with higher GFR values, with a mean eGFR of 93.2ml/min/1.73m2 being obtained using the CKD-EPI equation compared to 86.3ml/min/1.73m2 with the IDMS-MDRD equation.14 This is the equation recommended by the new 2013 KDIGO guidelines, given that it is more accurate than IDMS-MDRD for high GFR values, although it is highly imprecise, and as such, it is not useful for classifying CKD in stages 1 and 2, with signs of renal lesion also being required for the latter.8 The improvement in the predictive capacity of the real GFR, especially between values of 60 and 90ml/min/1.73m,2 and its greater capacity in the prognosis of overall mortality, cardiovascular episodes and risk of ESRD15 mean that we must consider the new CKD-EPI equation as the equation of choice in the future. In fact, the recently published “Chronic Kidney Disease Consensus Document”, in which ten scientific societies participated under the direction of the Spanish Society of Nephrology (S.E.N.), recommends using this equation.16
However, the recommendation to use CKD-EPI has not yet been implemented by most clinical laboratories,9 and as such, there is a need for tools that allow serum creatinine concentration to be quickly converted to the eGFR value using this equation. With this objective in mind, we have calculated and designed a table that allows the GFR to be estimated from serum creatinine concentration, age and sex, using the CKD-EPI equation, as we did previously with the IDMS-MDRD formula.17
METHODS
To create these tables, we used a spreadsheet with the Excel 7 software (Microsoft, USA). They are the result of applying the CKD-EPI formula to the mean values for age and creatinine concentration intervals, according to sex. Given the characteristics of the majority population in our country, we have omitted the correction factor for black individuals.
RESULTS
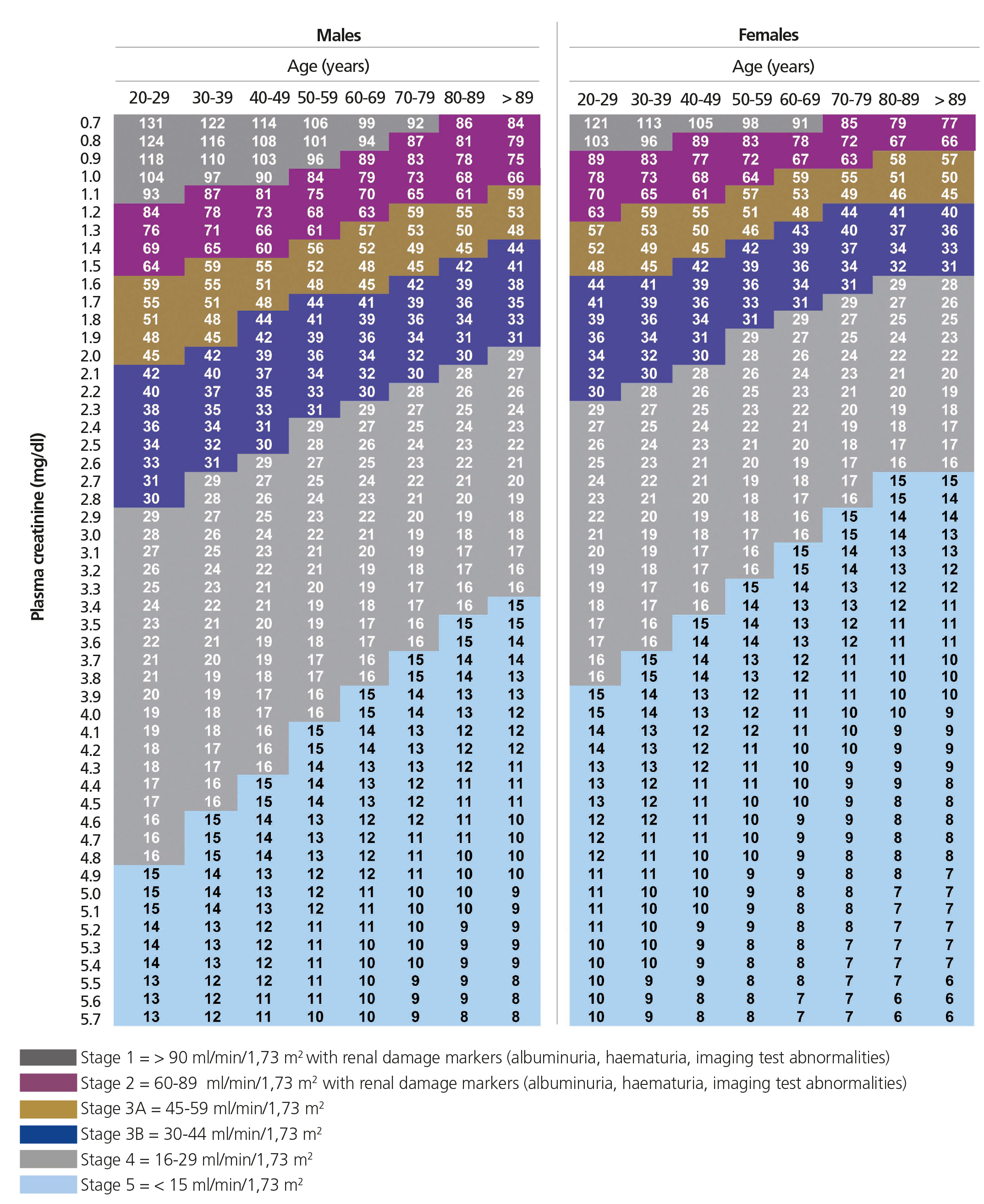
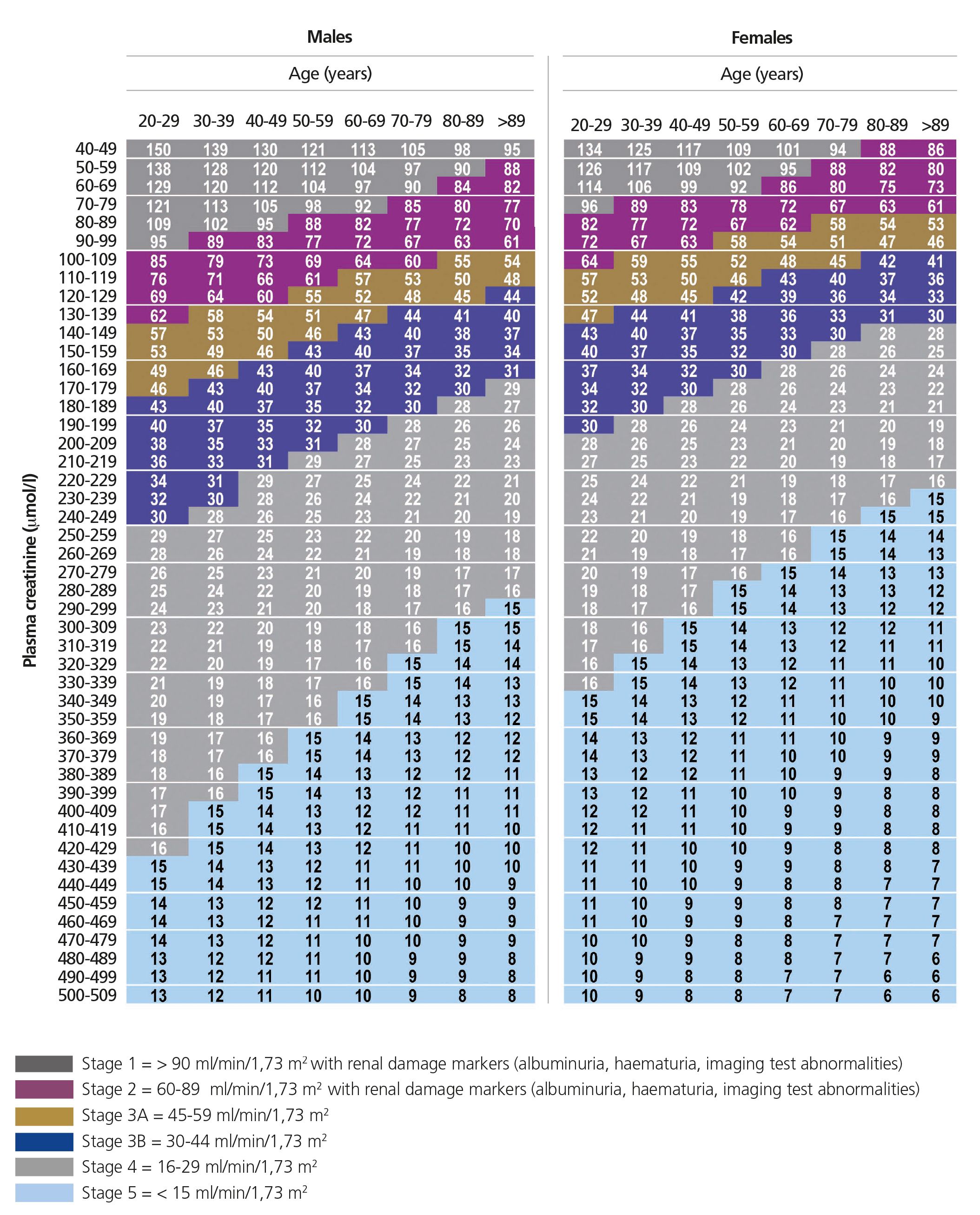
The tables show the eGFR value calculated using the CKD-EPI formula according to serum creatinine concentration, age and sex, using mean creatinine and age values for each interval and it is graded according to the different CKD stages. The results are displayed in two different tables, one in which serum creatinine concentration values are expressed in conventional units (mg/dl) and the other, which uses the International System (µmol/l) (Tables 1 and 2). The colour indicates the CKD stage to which the eGFR value corresponds.
DISCUSSION
As is well-known, most scientific societies,6,7,18-24 including the S.E.N. and the Spanish Society of Clinical Biochemistry and Molecular Pathology,25 currently advise using eGFR through equations obtained by measuring serum creatinine concentration, age, sex and race. These equations have been a great step forward in early diagnosis and classification of CKD stages, with resulting major advantages, since they allow different treatments to be established that are aimed at stopping or slowing down kidney disease progression and achieving early treatment of its complications (anaemia, secondary hyperparathyroidism, etc.).26-28
Until recently, the MDRD equation was recommended by most clinical guidelines and scientific societies6,7,18,29-31 and it has been demonstrated that the eGFR obtained from this equation is also useful for adjusting drug doses, since it is better suited than the Cockcroft-Gault equation for GFR32 values lower than 60ml/min/1.73m2. However, the MDRD equation has a series of limitations due to the population used in its development,33 who were individuals with different degrees of CKD, which resulted in its imprecision and systematic underestimation of the real GFR, particularly for GFR34-39 values greater than 60ml/min/1.73m2. This underestimation may cause some individuals to undergo unnecessary studies, receive non-optimal doses of renal clearance drugs or avoid important but potentially nephrotoxic diagnostic procedures.
Due to all of the above, the need to seek new renal function markers or new GFR estimation equations have been advocated, which may improve the results of MDRD, especially for GFR greater than 60ml/min/1.73m2. In 2009, the CKD-EPI group published a new equation developed from a population of 8254 individuals with different clinical characteristics, with or without kidney disease, which included serum creatinine concentration, age, sex and race as variables.14 The GFR was measured in all individuals by iothalamate clearance (mean 68ml/min/1.73m2, standard deviation = 40ml/min/1.73m2) and serum creatinine (mean 145μmol/l) using methods that were traceable with respect to the IDMS reference method. The mean age of the population was 47 years old, with 9% of patients aged between 66 and 70 years old and 3% older than 71. They developed different equations according to race, sex and serum creatinine concentration value. The comparison of CKD-EPI with IDMS-MDRD demonstrated that the former was more accurate, particularly with regard to GFR values greater than 60ml/min/1.73m2 and this was the reason for which the authors reached the conclusion that CKD-EPI should replace IDMS-MDRD in standard clinical practice, even though it was highly imprecise compared to directly measuring the GFR. The application of CKD-EPI in the NHANES study (1999-2006) (National Survey on Health and Nutrition Examination) demonstrated that the median eGFR was 94.5ml/min/1.73m2 compared with 85ml/min/1.73m2 estimated with IDMS-MDRD, with a CKD prevalence of 11.5% compared to 13.1%, a reduction basically caused by a decrease in cases classified by IDMS-MDRD as stage 3 CKD.
In a study published by our group, the first that attempted to assess the new CKD-EPI equation in our setting in a large patient cohort, we confirmed that the new equation produced higher values than those obtained with IDMS-MDRD, which resulted in a reclassification of patients to higher CKD stages, such that 9.8% of cases that were classified as stage 3b CKD were changed to 3a, 17% of 3a CKD were changed to stage 2 and 15.7% were changed from stage 2 CKD to stage 1.40 Furthermore, the analysis of age by subgroup demonstrated that this change towards higher GFR stages was greater in patients under 70 years of age. In the over 70 group, we observed a 90% concordance for CKD stages 2 to 5; by contrast, for those assigned to stage 1 CKD by IDMS-MDRD, a high number of cases were classified as stage 2 CKD by CKD-EPI. These data are similar to those obtained in a study carried out recently in our country in primary care, where fewer differences were observed between both equations for GFR estimation in older individuals than in the younger population.41 Similar results were reported in a recently published study in which it was observed that CKD-EPI is less biased and more accurate than MDRD also in an aged European population older than 74 years old, with the equation for this age range being as satisfactory as in young subjects.12
As was previously mentioned, we believe it is important to highlight that in various studies, the CKD-EPI equation was associated with a better prognostic classification than IDMS-MDRD with respect to overall mortality, cardiovascular episodes and end-stage renal disease.43-45 Likewise, the results of a recent meta-analysis conclude that CKD-EPI classifies fewer individuals with CKD and more reliably categorises the risk of mortality and ESRD than the IDMS-MDRD equation in a wide population range.15
New equations have recently been published based on serum creatinine concentration that aim to improve precision and decrease bias;46 the current guidelines consider their use to be acceptable provided that they demonstrate more accuracy than CKD-EPI. We should also remember that the use of cystatin C serum concentration or eGFR by equations from it is subject to variables that are not dependent on the GFR and that its methods of measurement are being standardised. For now its use is recommend as a confirmatory measurement in adults with a GFR between 45 and 59ml/min/1.73m2 without other renal lesion markers. In this case, the recommended equation is CKD-EPI for recently published standardised cystatin C.47
Due to the above, we believe that providing tools that allow a quick conversion of serum creatinine concentration to eGFR using this new equation could be useful, particularly when clinical laboratories do not have it incorporated in their reports, whether it be in our country or abroad, such as Latin America. It is important to note that the CKD-EPI equation is only applicable if standardised methods of measuring creatinine are employed. Furthermore, today, measuring eGFR is an important parameter on which many guidelines base the referral of patients to nephrologists, amongst others.
In summary, although the method currently recommended for determining the eGFR would be automatic calculation of CKD-EPI formulae by laboratories, in the meantime the availability of these tables allows the visualisation and conversion of standardised serum creatinine concentration by doctors, in order that they may transform it quickly and simply into a more clinically significant parameter, such as eGFR. Likewise, this additional information may provide a higher predictive capacity than isolated creatinine concentration or the eGFR equations used previously.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. Calculation of the glomerular filtration rate according to serum creatinine concentration (mg/dl) and age using the CKD-EPI equation (white individuals).
Table 2. Calculation of the glomerular filtration rate according to serum creatinine concentration (µmol/l) and age using the CKD-EPI equation (white individuals).