We present the case of a 22-month-old girl assessed by a multidisciplinary team as she had seizures that were difficult-to-manage that started when she was 6 months old and she had bilateral polycystic kidney disease. Her parents were healthy and not consanguineous. She was born as a result of her mother's second pregnancy, an unmonitored single-foetus pregnancy complicated by HELLP syndrome. She was delivered by Caesarian section after 36 weeks, required resuscitation at birth and had generalised cyanosis. Her birth weight was 1700g (DE −3.8) and her birth length was 46cm (DE −2.5). She was hospitalised at 8 months of age due to tonic–clonic seizures, followed a torpid course with global delay in maturation delay.
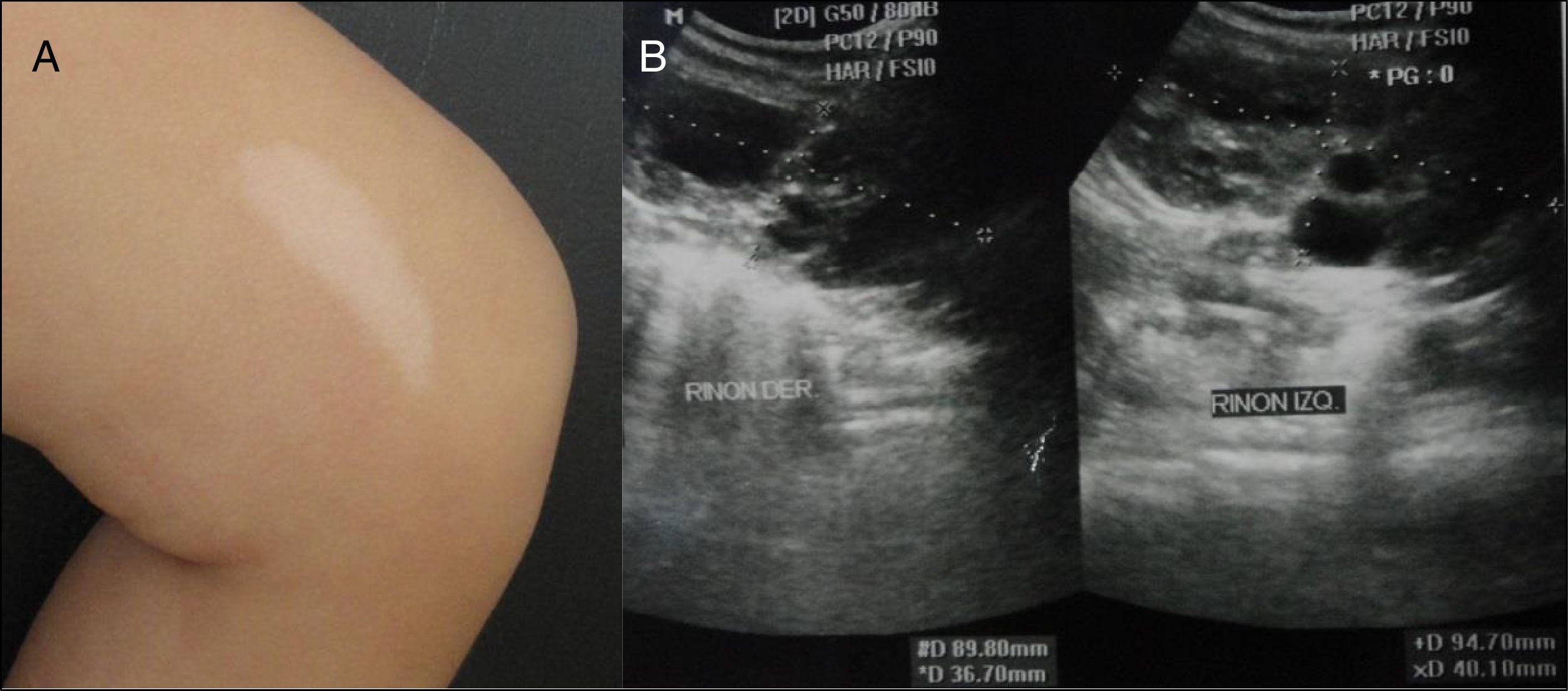
On physical examination, she had a tendency towards dolichocephaly with an unusual facies characterised by a prominent forehead; a concave nasal bridge with a flattened tip; upturned nostrils; and a short, wide philtrum. She had 7 hypochromic lesions; 2 were ash-leaf that corresponds to the largest in her lumbar region and on her left thigh (Fig. 1a).
An MRI scan showed patch-shaped multi-focal areas with hyperintense behaviour on T2 flair in both parietal hemispheres not leading to a mass effect on the surrounding structures. A sleep electroencephalogram was abnormal due to paroxysmal activity with bursts of points and acute waves in the fronto-polar and right temporal regions. An eye ultrasound showed a raised lesion with a hypoechoic internal structure in the papillary area, consistent with an astrocytic hamartoma of the optic nerve of the right eye. A transthoracic echocardiogram showed tumour in the right ventricular outflow tract suggestive of rhabdomyoma neither causing obstruction nor resulting in haemodynamic repercussions. A kidney ultrasound showed an increase in volume in both kidneys, 9.4cm×4.0cm for the left kidney and 9cm×3.6cm for the right kidney. It revealed the formation of fluid-filled cysts, some of which had thick walls. The largest one, in the lower pole of the right kidney, was 6cm×3.1cm (Fig. 1b). A kidney profile, as well as other serum analysis, was found to be within the reference values.
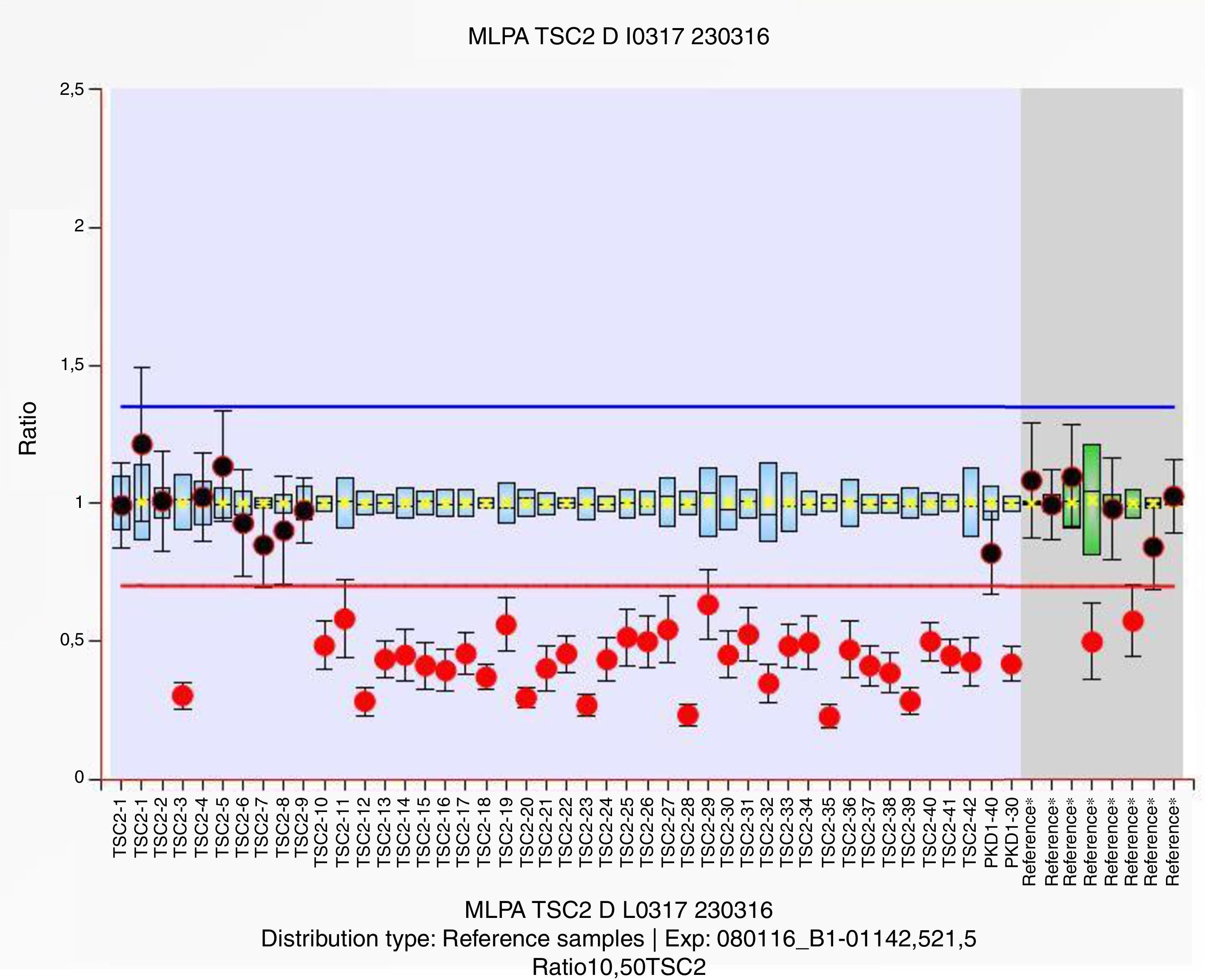
DNA was extracted, and mass sequencing of the TSC1 and TSC2 genes was performed on the MiSeq (Illumina) platform. This revealed 2 polymorphisms in heterozygosis in TSC1, GAA/GAG, c.1335A>G, p.Glu445Glu and ATG/ACG, c.965T>C, p.Met322Thr with rs7862221 and rs1073123 references, respectively. A multiplex ligation-dependent probe amplification study (MLPA P337) showed a deletion in heterozygosis of the probes located in exons 10–42 of the TSC2 gene, as well as exons 30 and 40 of the PKD1 gene (Fig. 2).
Tuberous sclerosis complex (OMIM #191100 and #613254) is a multi-system disorder that exhibits an autosomal dominant inheritance pattern. It is characterised by multiple hamartomas of the brain, eyes, heart, kidneys and skin.1–3 It has a broad, variable phenotypic spectrum that includes seizures, intellectual disability and kidney and skin abnormalities, as well as an increased risk of malignancy.2,4 Its incidence is one in every 6000–11,000 live births.1 It is due to mutations in the TSC1 (OMIM #605284) and TSC2 (OMIM #191092) tumour suppressor genes, which encode hamartin and tuberin, respectively.1,3 The latter gene is located in 16p13.3 adjacent to the PKD1 gene (OMIM #601313), responsible for 85% of cases of polycystic kidney disease (OMIM #173900), which also has an autosomal dominant inheritance pattern.1,5 This is the most common hereditary kidney disorder, with an incidence of one in every 400–1000 live births.5
A large deletion which may encompass the genes TSC2 and PKD1 causes so-called TSC2/PKD1 contiguous gene syndrome (OMIM #600273).1,2,5 It was first reported by Brook-Carter et al. in 1994 in 6 patients with tuberous sclerosis complex with severe childhood polycystic kidney disease.6 It is characterised by large bilateral kidney cysts. These cysts may be congenital or of very early onset, which may alter the disease prognosis. It has been estimated that 5% of patients with tuberous sclerosis complex have polycystic kidney disease.1
Kidney complications represent the second leading cause of death after neurological impairment in tuberous sclerosis complex. Angiomyolipomas are the most common kidney abnormality in adults and children, and may be present in 16% of cases, in addition to small cysts and renal cell carcinoma.1,3
We present the case of a girl with a genetic and clinical diagnosis of TSC2/PKD1 contiguous gene syndrome, with an emphasis on multidisciplinary assessment given her pleiotropy and disease severity, as well as appropriate genetic counselling with a 50% risk of recurrence in descendants of affected individuals.
Please cite this article as: Cammarata-Scalisi F, Vidales Moreno C, Zara-Chirinos C, Bracho A, Pérez D. Síndrome de genes contiguos TSC2/PKD1. Nefrologia. 2017;37:663–665.