To the Editor,
Tubulointerstitial nephritis (TIN) with uveitis (TINU) is a rare disease whose pathogenesis is unknown.
We present the case of a boy 9 years of age examined for glycosuria. The patient had asthenia, anorexia and had lost more than 5kg body weight in the course of 1 month. No prior infections. The patient experienced nocturnal enuresis which was treated with desmopressin; that treatment was suspended 2 months before onset of the listed symptoms.
Examination revealed high blood pressure (maximum 135/97mm Hg), with other values being normal.
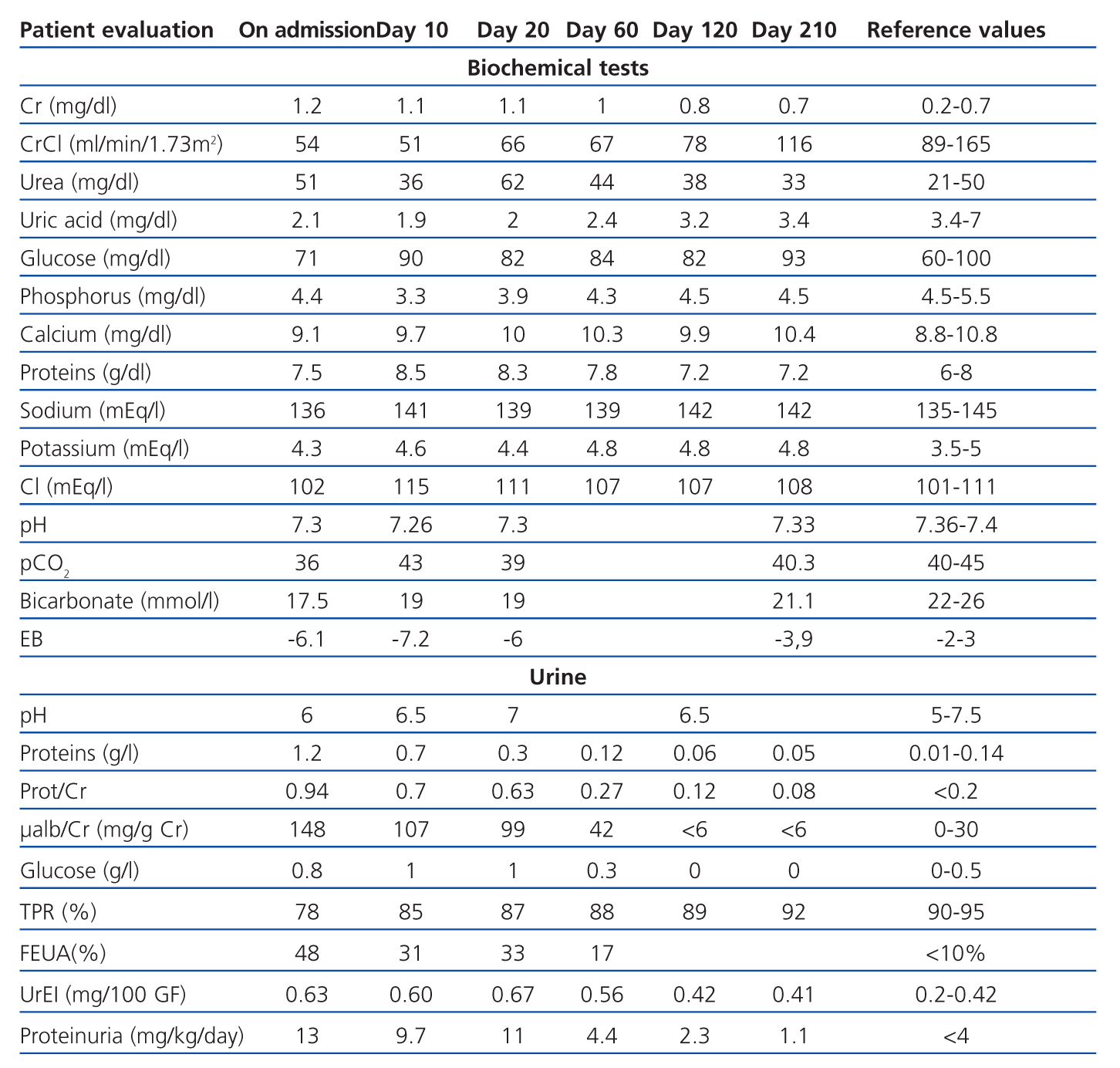
Blood analysis revealed renal dysfunction: creatinine (Cr) 1.2mg/dl; creatinine clearance 64ml/min/1.73 m2; urea 51mg/dl; uric acid 2.1mg/dl; phosphorus 4.4mg/dl; mild metabolic acidosis with C-reactive protein 29mg/l and globular sedimentation velocity 62mm (Table 1).
The urine analysis showed glycosuria (0.8g/l); non-nephrotic range proteinuria (13mg/kg/day, microalbuminuria 148mg/g Cr); hyperphosphaturia with low tubular phosphate reabsorption (78%); hyperuricosuria with a high uric acid index (0.78 100mg/100ml); normal glomerular filtration and calcium levels (1.1mg/kg/day); fractional excretion of sodium 0.3%, and fractional excretion of potassium 19%. Urinary sediment showed granular and hyaline casts, leukocyturia without eosinophils and a negative urine culture.
These findings are compatible with multiple dysfunctions of the proximal tubule (PT), or Fanconi syndrome.
Liver, thyroid and parathyroid functions were normal. The immunological study revealed low-level positivity for antinuclear antibodies (1/80). The anti-streptolysin O (ASLO) titre was high (2175IU/ml) with a negative oropharyngeal culture. Immunoglobulin levels were normal, but IgG was high 1 week later (1820mg/dl). An IgM test was run for Epstein-Barr, cytomegalovirus, parvovirus B19, toxoplasmosis and hepatitis B and C. All were negative. Renal ultrasound was normal.
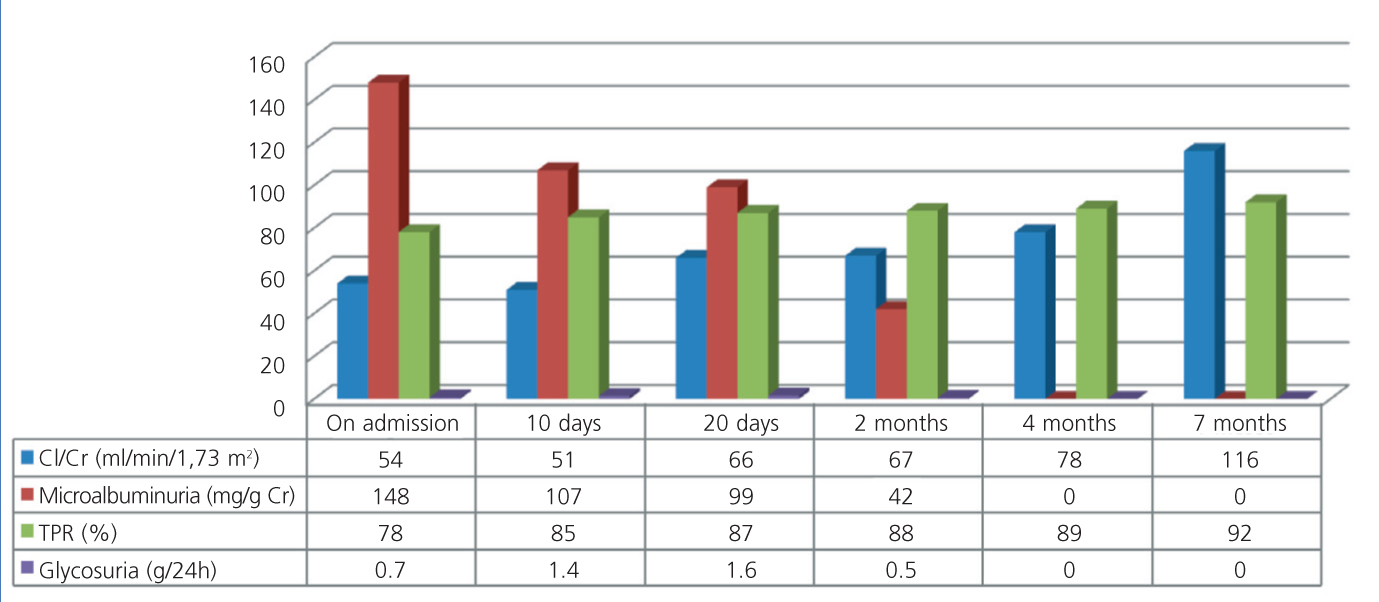
Given the PT dysfunction and mild renal failure, we suspected a case of TIN. We adopted a watchful waiting approach and kidney function and blood pressure normalised in less than 4 weeks. No kidney biopsy was performed (Figure 1).
One month after renal symptoms began, he presented with acute anterior uveitis, which evolved favourably under treatment with topical steroids and cycloplegic agents.
According to Mandeville’s criteria,1 we diagnosed tubulointerstitial nephritis associated with uveitis (TINU). After 18 months, renal function remains normal, although there have been various relapses of uveitis.
DISCUSSION
The aetiology and pathogenesis of this disease are unknown, but hypotheses suggest mechanisms mediated by cellular immunity. It has been linked to infections, systemic diseases and previous use of medications.2
In our case, the high ASLO titres suggested a streptococcus infection, but there were no associated symptoms and the oropharyngeal culture was negative. It seems unlikely to have originated with the desmopressin as no causal relationship has been established. We have not found any cases linking TIN to the use of that drug.
Clinical manifestations are variable, with non-specific systemic symptoms and renal symptoms that include flank pain, sterile pyuria, haematuria, non-nephrotic range proteinuria and different stages of renal failure. Proximal and distal tubular defects may also be associated.
Our patient presented glycosuria with general PT dysfunction, moderate renal dysfunction and mild hypertension.
We diagnosed TINU syndrome according to Mandeville's criteria.1 Differential diagnosis was performed to rule out other entities involving both renal and ocular disease,2 such as sarcoidosis, Sjögren's syndrome, Wegener's granulomatosis, Behçet’s disease, toxoplasmosis, tuberculosis, histoplasmosis and brucellosis.
Renal dysfunction tends to be self-limiting,3 but becomes persistent in some 10% of patients. Oral steroids are the treatment of choice,4 although immunomodulators may also be used in patient with a poor response.2
Uveitis may develop prior to (in 20%) or after (in 65%) renal symptoms, and is rarely concomitant. Cases of uveitis presenting as much as 2 months before or 14 months after renal symptoms have been observed.2 Uveitis generally has a favourable prognosis, but some articles report complications in up to 20% of patients2 and relapses are frequent.
Since the manifestations of TINU syndrome are non-specific, its true incidence rate may be underestimated. Both nephrologists and ophthalmologists must be aware of this entity and check renal function in patients with uveitis (and vice versa).
Conflicts of interest
The authors affirm that they have no conflicts of interest related to the content of this article.
Table 1. Laboratory blood and urine analyses at onset of symptoms and during syndrome progression
Figure 1. Creatinine clearance, microalbuminuria, tubular reabsorption of phosphate and glycosuria