Traditionally, the indication of the type of vascular access (VA) has been based on the surgeon's physical examination, but it is now suggested that imaging methods could provide a clinical benefit. Our aim was to determine whether or not preoperative Doppler ultrasound modifies outcomes of the first VA for hemodialysis.
Patients and methodsProspective cohort of patients undergoing a first VA from June 2014 to July 2017 who had a preoperative Doppler ultrasound (ECO group). They were compared to a historical cohort (January 2012–May 2014) of first VA indicated exclusively by clinical assessment (CLN group).
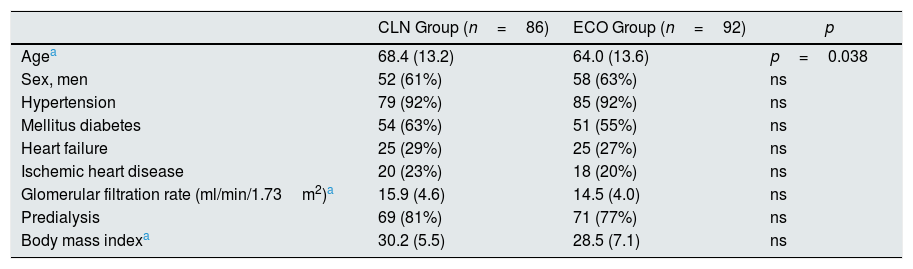
ResultsA total of 86 patients from the CLN group were compared to 92 from the ECO group, which was younger (68.4 vs 64.0, p=0.038).
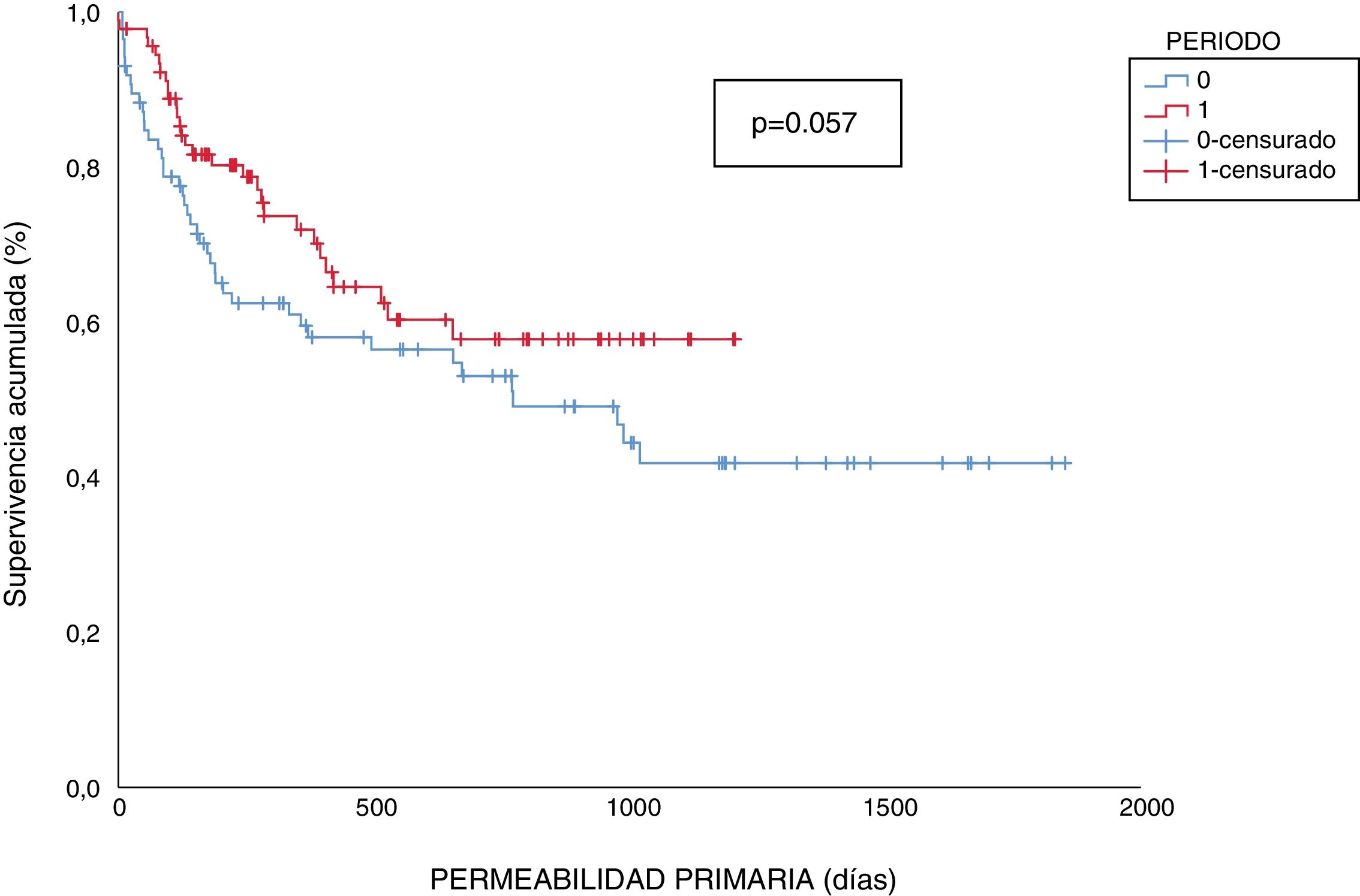
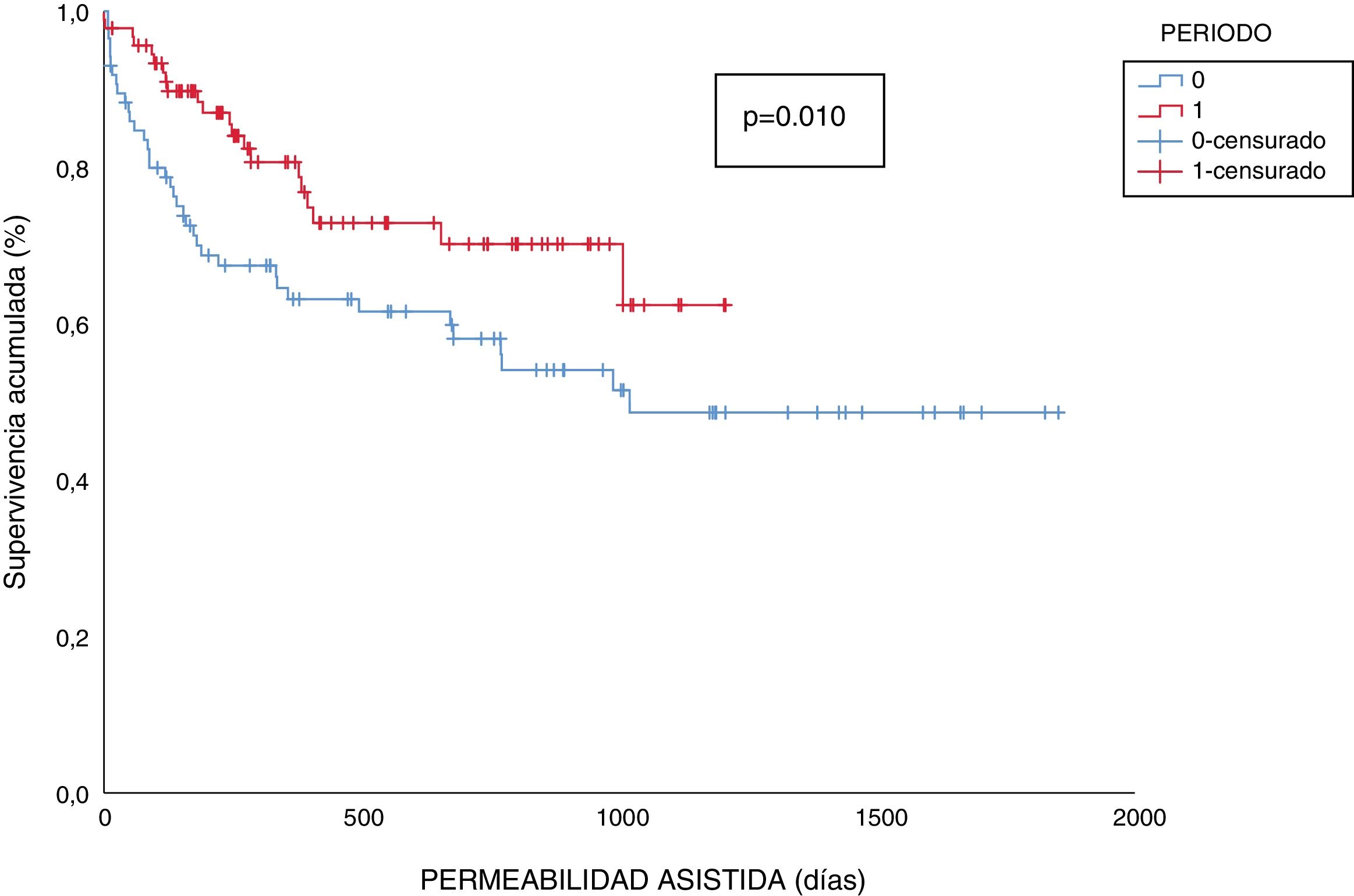
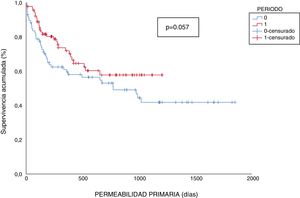
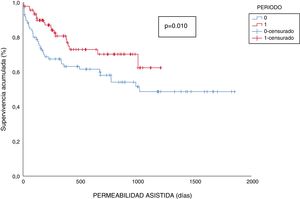
The primary patency (CLN/ECO) at 1 and 2 years was 59.5%/71.9% and 53.1%/57.8% respectively, marginally better in the ECO group (p=0.057). The assisted patency at 1 and 2 years was 63.2%/80.7% and 58.1%/70.2%, respectively, significantly better for the ECO group (p=0.010).
Due to lack of patency/utility of the initial VA, 26.7% in the CLN group and 7.6% in the ECO group (p<0.001) required a new VA during the first 6 months. An average of 1.39 interventions were performed to achieve a useful VA in the CLN group and 1.08 in the ECO group (p<0.001), the first VA being useful at the radiocephalic level in 31.0%/45.1% (p=0.039).
ConclusionThe indication of the first VA according to a preoperative Doppler ultrasound examination could decrease the need for new VA, enable them to be made more distal, and significantly improve patency.
Tradicionalmente la indicación del tipo de acceso vascular (AV) se ha basado en la exploración física del cirujano, pero actualmente se sugiere que los métodos de imagen podrían aportar un beneficio. Nuestro objetivo fue valorar si el eco-doppler preoperatorio modifica los resultados del primer AV para hemodiálisis.
Pacientes y métodosCohorte prospectiva de pacientes sometidos a un primer AV entre junio de 2014 y julio de 2017, a quienes se practicó un eco-doppler preoperatorio (grupo ECO). Se compararon con una cohorte histórica (enero de 2012-mayo de 2014) de primeros AV indicados exclusivamente mediante clínica (grupo CLN).
ResultadosSe compararon 86 pacientes del grupo CLN con 92 del ECO, siendo estos últimos más jóvenes (68,4 vs 64,0 años; p=0,038).
Las permeabilidades primarias (CLN/ECO) a 1 y 2 años fueron del 59,5/71,9% y del 53,1/57,8%, marginalmente mejores en el grupo ECO (p=0,057). Las permeabilidades asistidas a 1 y 2 años fueron del 63,2/80,7% y del 58,1/70,2%, siendo significativamente mejores para el grupo ECO (p=0,010).
Requirieron un nuevo AV durante los primeros 6 meses, por falta de permeabilidad/utilidad del inicial, el 26,7% en el grupo CLN y el 7,6% en el ECO (p<0,001). Se realizaron una media de 1,39 intervenciones para conseguir un AV útil en el grupo CLN y 1,08 en ECO (p=0,001), siendo el primer AV útil a nivel radiocefálico en el 31,0/45,1% (p=0,039).
ConclusiónLa indicación del primer AV en función de una exploración mediante eco-doppler preoperatoria podría mejorar de forma significativa la permeabilidad, disminuir la necesidad de nuevos AV y permitir realizarlos más distales.
An adequate vascular access (VA) available before initiation of the hemodialysis (HD) program is a big challenge in end-stage renal disease. It is widely recognized that native arteriovenous fistulas (AVF) are the ideal VA, but early failure is up to 23%1 and a limited medium-term primary permeability is 60% the first year and 51% at 2 years.1 Insufficient maturation of 28–53%2 of the accesses impede the availability of a functioning nAVF at the time it is needed.
Traditionally the decision of the type of VA has been made based on the history and physical examination, but these elements usually do not allow a correct assessment of venous system (especially in case of obesity or history of punctures) or the artery (in diabetic patients or with peripheral arterial disease).3
The use of a preoperative echo-Doppler (ED) in patients undergoing AV for HD could improve the clinical evaluation. ED is non-invasive, widely available, and provides anatomical and hemodynamic information that made it an important tool when planning any AV strategy. In fact, for some years the use ED has been recommended by the clinical guidelines of the Kidney Disease Outcomes Quality Initiative (KDOQI),4 of the European Renal Association-European n Dialysis and Transplant Association (ERA-EDTA)5 and more recently by the Spanish Multidisciplinary Group Vascular Access (GEMAV),6 although recommendations have been made with a low level of evidence. However, at the moment, in daily clinical practice the use of ED is not generalized.
The objective of this study was to assess whether the introduction of a preoperative echo-doppler results in a modification of the usual strategy of performing AVF, permeability and success of the vascular access for HD, as well as the need for further interventions.
Patients and methodsProspective cohort of consecutive patients who had a first VA for HD between June 2014 and July 2017 (ECO group) in the Department of Angiology and Vascular Surgery of Hospital del Mar (Barcelona). All patients were evaluated preoperatively clinically and by means of echo-doppler.
The control group (CLN group), included a cohort of consecutive patients that had VA for HD between January 2012 and May 2014 in the same center and were analyzed retrospectively.
In both groups, the decision of the type of VA to be performed was taken by experienced vascular surgeons, in the CLN group only with clinical assessment and in the ECO group the decision was based on the information obtained with preoperative echo-doppler.
The clinical evaluation included demographic variables (age, sex), clinical history (diabetes mellitus, body mass index) and nephrological data (active HD or pre-dialysis, previous central venous catheters [CVC]). The physical examination included pulses in the upper extremities, Allen's maneuver, presence of scars, edema or collateral circulation and clinical exploration of venous drainage with proximal compression using smarch.
The ultrasound assessment was performed by a single operator using a linear transducer of 7–11MHz and Logiq S7 Expert equipment (General Electric Healthcare, USA). The radial and humeral arteries were analyzed in the examination, considering them suitable for AV if: (a) diameter>2mm; (b) absence of significant calcification; (c) thriphasic doppler curve, and (d) peak-systolic velocity>50cm/s. The venous examination was performed with proximal compression using smarch and the veins were considered suitable for VA if: (a) diameter>2.5mm; (b) depth<6 mm, and (c) permeability throughout its path.7,8 Finally, the absence of indirect signs of proximal venous occlusion (axillary respiratory fasicity) was assessed.
The time elapsed between the indication of the VA by the nephrologist and the assessment by the vascular surgeon and the delay between this visit and the performance of the surgical intervention were collected.
The interventions were performed by experienced vascular surgeons. The first follow-up visit was scheduled two weeks after surgery with the vascular surgeons. Subsequently controls were performed by Nephrology clinics every 3–4 months in CKD stage 4 (eGFR between 30–15ml/min) and every 1–2 months in stage 5 (FG<15ml/min). Patients with lack of maturation of the VA or with abnormal function had and ultrasound performed by Vascular Surgery.
The following parameters were recorded during the follow-up, permeability, satisfactory use during HD, reinterventions and the need for new VA. A mature VA was considered if that complied with the rule of 6- by echo-doppler (vein diameter>6mm, depth<6mm, flow>600ml/min), which could be punctured by an experienced HD nurse.
The statistical analysis was performed using the program SPSS version 22. For the descriptive analysis, the mean and standard deviation (SD) were used for quantitative variables, and the frequency and percentages for qualitative variables. The comparison between groups was made using the Student's t-test for quantitative variables and the chi-square or Fisher's test for qualitative variables. The permeability analysis was performed using Kaplan–Meier survival curves and were compared by the Log-Rank and Breslow tests. The multivariable analysis was performed using Cox and logistics regression.
ResultsFrom the initial 113 patients in the ECO group, 12 patients had to be excluded because the preoperative ultrasound could not be performed (the ultrasound equipment was not available) and 9 patients in whom new clinical events advised against the use of echo-doppler for the election of the first VA (4 were AVFs in which there was a change of laterality but not of level because the indicated veins had been injured by punctures; 4 were AVFs performed at a proximal level, in patients requiring a fast VA and the surgeon considered that it would imply a faster maturation, and one was performed distally without a described cause). Therefore, the ECO group finally included 92 patients, while 86 were included in the CLN group.
Regarding the baseline characteristics, patients from the ECO group were younger than the CLN group. Table 1 describes the characteristics of both groups of patients.
Baseline characteristics of patients undergoing first surgical vascular access for hemodialysis, indicated after clinical assessment (CLN) or after the use of preoperative echo-Doppler (ECO).
| CLN Group (n=86) | ECO Group (n=92) | p | |
|---|---|---|---|
| Agea | 68.4 (13.2) | 64.0 (13.6) | p=0.038 |
| Sex, men | 52 (61%) | 58 (63%) | ns |
| Hypertension | 79 (92%) | 85 (92%) | ns |
| Mellitus diabetes | 54 (63%) | 51 (55%) | ns |
| Heart failure | 25 (29%) | 25 (27%) | ns |
| Ischemic heart disease | 20 (23%) | 18 (20%) | ns |
| Glomerular filtration rate (ml/min/1.73m2)a | 15.9 (4.6) | 14.5 (4.0) | ns |
| Predialysis | 69 (81%) | 71 (77%) | ns |
| Body mass indexa | 30.2 (5.5) | 28.5 (7.1) | ns |
The time elapsed between indication of VA by the Nephrologist and evaluation by the vascular surgeon was 23.8 days (SD=23.8) for the CLN group and 17.6 days (SD=17.2) for the ECO group, the difference was close to significant (p=0.063), and the period between the evaluation and the realization of the VA was 53.3 days (SD=70.7) and 32.1days (SD=35.6), for CLN and ECO group respectively, the difference being statistically significant (p=0.012).
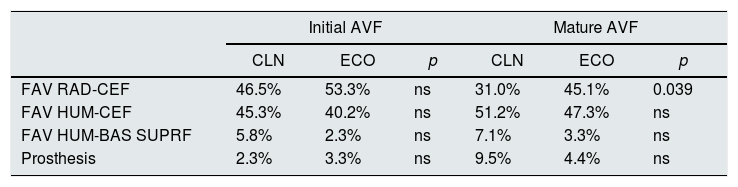
The type of VA performed in each of the groups is described in Table 2. There were no significant differences between them. The VA was performed in the left arm in 64% of CLN patients and in 68.5% of the ECO group.
Location of the first vascular access in the initial intervention (initial AVF) and the first useful or mature AV (mature AVF), indicated after clinical assessment alone (CLN) or after preoperative echo-doppler (ECO), values presented as percentage.
| Initial AVF | Mature AVF | |||||
|---|---|---|---|---|---|---|
| CLN | ECO | p | CLN | ECO | p | |
| FAV RAD-CEF | 46.5% | 53.3% | ns | 31.0% | 45.1% | 0.039 |
| FAV HUM-CEF | 45.3% | 40.2% | ns | 51.2% | 47.3% | ns |
| FAV HUM-BAS SUPRF | 5.8% | 2.3% | ns | 7.1% | 3.3% | ns |
| Prosthesis | 2.3% | 3.3% | ns | 9.5% | 4.4% | ns |
AVF: arteriovenous fistula; HUM-BAS SUPERF: superficialized humerobasilic; HUM-CEF: humerocephalic; ns: not significant; RAD-CEF: radiocephalic.
There were 21 immediate complications from the CLN group (24.4%): 10 immediate thrombosis, 3 mild bruising, 5 mild infection, 2 mild “steal” ischemia and one deep vein thrombosis of the lower limb. In 8 interventions, a surgical exploration of the carpal vein was performed, and it was decide to place a more proximal VA. In the ECO group, 11 patients (12%) had immediate post-surgical complications: 2 thrombosis, 2 bruises (one required surgical revision), 5 minor wound infections, one mild “steal” ischemia and a persistent edema of the extremity. The rate of immediate complications was lower in the ECO than CLN group (p=0.024).
Mean follow-up was 1277 and 556 days in the CLN and ECO group respectivey. Primary permeability in the CLN group at 1, 6, 12 and 24 months were 89.5, 67.6, 59.5 and 53.1% respectively; whereas in the ECO group primary permeabilities were 97.8, 81.6, 71.9 and 57.8%. Primary permeabilities appear to be better in the ECO group however the differences were marginally significant, (p=0.057) (Fig. 1).
During follow-up, to maintain the function of the VA, 7 additional interventions were required in the CLN group (4 deferred superficializations, 2 simple angioplasties and a collateral ligation) and 13 in the ECO (9 simple angioplasties, 2 deferred superficializations and 2 segmental thrombectomies). Assisted permeability rates in the CLN group at 1, 6, 12 and 24 were of 89.5, 70.0, 63.2 and 58.1%, while in the ECO group were 97.8, 88.4, 80.7 and 70.2%. Permeability rates for the ECO group were significantly greater in ECO than CLN group (p=0.010) (Fig. 2).
To limit the bias of difference in age between the groups, the permeability analysis was repeated stratifying for an age less than and above 65 years. In the primary permeability significant differences were detected in the <65 years (p=0.049), while in the >65th birthday, no statistical differences (p=0.209). Regarding of assisted permeability, differences between groups were maintained in both <65 year (p=0.047) and in >65 (p=0.042).
During the first 6 months after surgery due to thrombosis or non- functional access a new VA was required in 26.7% of patients in the CLN group and 7.6% in the ECO group (p<0.001). An average of 1.39 interventions were carried out until a useful VA was achieved in the CLN and 1.08 in the ECO group (p<0.001). As a consequence of these interventions, the first useful VA for HD was significantly more distal in the ECO group than in the CLN group (p<0.001) (Table 2).
By multivariable Cox regression and logistics analysis none of the clinical variables evaluate had significant influence in the permeability or the need for new VA.
The percentage of patients that required a catheter to initiate HD was 19% in the CLN group of and 22%in the ECO group; these values were not significantly different. In the ECO group, the 20 CVC were placed due to the need for urgent HD before being referred to Vascular Surgery for the assessment and performance of the AVF. In the CLN group, there were 14 catheters also implanted to initiate HD, but 2 CVC were placed after the completion of the AVF, due to the lack maturation of the AVF at the time of starting the HD.
Patients not included in the study were also reviewed, obtaining a primary permeability per year of 54% and 57% assisted. Permeability analysis was repeated per intention of the treatment, including the excluded in the ECO group, and the overall primary permeability at 1 and 2years was 68.9 and 56%, and assisted permeability of 76.4 and 68%. As far as primary permeability these results were not statistically different from that obtained in the CLN group (p=0.19) but were statistically different in terms of assisted permeability (p=0.045).
DiscussionHaving an adequate VA at the start of the HD is a challenge, and more so considering that the recommended VA should be a native AVF (nAVF). The literature describes rates of early failure of 23%, a limited primary patency of (60% at year 1 and 51% at 2 years)1 and a lack of maturation of 28–53%,2 which makes many of the nAVF useless. These figures are similar to those observed in our historical control. Therefore, introducing a change that could improve the prognosis of the technique would be a great advance.
However, at the scientific level there is still controversy regarding the usefulness of the ultrasound evaluation prior to the VA. Ferring et al.,9 published in 2008 a review in which they conclude that preoperative echo-doppler should be reserved for certain cases in which there are difficulties for the clinical examination (obese, absence of pulses, previous surgeries), patients with possible peripheral vascular disease or with possible venous lesions. A more recent review of Cochrane10 in 2015 also concludes that the preoperative instrumental evaluation does not improve the results of the AVF. By contrast, the meta-analyzes performed by Wong et al.,11 in 2013 and Georgiadis et al.,12 in 2015, based on 3 and 5 clinical trials, respectively, suggest a benefit of using ED routinely in preoperative exploration, with better long-term permeability rates.
The patients included in the two groups of our study(CLN and ECO) are similar, except for a more advanced average age in the CLN group. Among the recognized risk factors,13,14 advanced age is one of those that may imply a worse prognosis of VA,15 especially in distal AVF. The difference found between study groups (68.4 vs 64 years) might have some have had some influence in the worse outcome of the CLN group. For this reason we perform a new analysis of permeability stratifying by age, confirming that, regardless of the age difference between the study groups, the ultrasound assessment influences the permeability, since significant results are maintained in assisted permeability and Statistical significance is reached in the primary permeability of the subgroup <65 years. As for the rest of the variables, they also showed no influence on the permeability results in the multivariable analysis.
The implementation of the program resulted in a modification of the referral protocols of the patients, as well as improvements in the registration of patients waiting for intervention. These changes have allowed a significant reduction in the delay times of both valuation (by 35%) and intervention (by 66%).
There were no differences in the percentage of patients who required a catheter to start dialysis (22% vs 19%), observing an increase in cases not controlled by Nephrology that have needed HD urgently, without influencing in these cases the improvements of the branch circuit for the realization of a FAV. It has been reduced to zero is the need to place a CVC for delays in the placement or maturation of the AVF.
The improvement observed in primary and assisted permeability is clinically relevant, although in the case of assisted permeability it has been at the price of an increase in endovascular intervention. At this point, the evaluation with echo-Doppler has also influenced the favorable results since in patients whose nephrologist detects a lack of maturation using the ED may help to have the lesion corrected early.
But the most remarkable result is the decrease in the need to perform new VA, with 30% less reinterventions, and with a significant increase in the number of functioning and useful distal radiocephalic vascular accesses (difference that was already observed after the first intervention, but did not reach significance).
To the benefits described by the study, one could add another more intangible one, which would be the possibility of better planning of future accesses, since, knowing from the beginning the arterial and venous heritage, better strategies we can design based on the options available.
Our study presents the main limitations of having a limited number of patients, the retrospective nature of the control cohort and a parallel increase in endovascular intervention in the follow-up of VA. As for the patients rejected from the study, their results are comparable with those of the CLN group, a fact consistent with the fact that they were carried out without taking into account the ultrasound recommendation and the reason why it was decided not to include them in the study group.
Given the results presented, the use echo-doppler scan for indication of the first VA seems to improve the results, it could increase the permeability, reduce the need for new VAs and place them more distally, although at the expense of greater endovascular intervention during follow-up.
Financial supportThe present investigation has not received specific aid from public sector agencies, commercial sector or non-profit organizations.
Conflicts of interestThe authors have no conflicts of interest to declare.
This article has been carried out within the framework of the doctoral studies of the Autonomous University of Barcelona (UAB).
Please cite this article as: Mateos Torres E, Collado Nieto S, Cao Baduell H, Lacambra Peñart M, Velescu A, Clará Velasco A. Utilidad de la valoración ecográfica previa a la realización del primer acceso vascular para hemodiálisis. Nefrologia. 2019;39:539–544.