Antecedentes: La falta de adherencia a la medicación inmunosupresora se asocia con la pérdida de injerto y con la muerte. El cuestionario simplificado de adherencia a la medicación (SMAQ) es un instrumento de evaluación de adherencia corto y fiable. Objetivo: Validación de una versión del cuestionario SMAQ, adaptado para evaluación de pacientes trasplantados, en una muestra de receptores de trasplante renal. Métodos: Estudio observacional, longitudinal prospectivo en 150 pacientes mayores de edad, con injerto renal de al menos un año de evolución, en terapia con tacrolimus. Se recogieron datos sociodemográficos y clínicos básicos. Los pacientes completaron el cuestionario SMAQ dos veces (administrado por médico/personal de enfermería) y la escala Morisky-Green. Se estudiaron los descriptivos de los parámetros recogidos y las características psicométricas del cuestionario (fiabilidad y validez). Resultados: La edad media de la muestra fue de 50,63 años (12,44), el 60,42% fueron hombres. El 20,14% de los pacientes presentaron concentraciones de tacrolimus subtarget (<5 ng/ml) y el 13,48% variaciones injustificadas en los niveles de inmunosupresor. Según el cuestionario SMAQ, el 39,01/41,84% de los pacientes eran no cumplidores (administración médico/personal de enfermería), el 22,38% según Morisky-Green. El coeficiente kappa para reproducibilidad interobservadores fue 0,821 (p <0,001). La V de Cramer para validez convergente fue 0,516 (p <0,001). La clasificación según SMAQ se asoció con las variaciones injustificadas en los niveles de tacrolimus. En la predicción de niveles de tacrolimus (target frente a subtarget), SMAQ comparado con Morisky-Green, clasificó mejor a los pacientes y presentó una mayor sensibilidad y una menor especificidad. Conclusiones: El cuestionario presenta buenas características psicométricas. Una mayor sensibilidad permite una mejor detección de pacientes no cumplidores para un mejor seguimiento.
Background: Non-adherence to immunosuppressive medication is associated with graft loss and death. The simplified medication adherence questionnaire (SMAQ) is a short and reliable instrument for assessing adherence to medication. Objective: Validation of a version of the SMAQ instrument adapted for use in transplant patients in a sample of kidney graft recipients. Methods: Observational, longitudinal prospective study in 150 renal transplant patients on tacrolimus, over 18 years old, who had received a graft at least one year before. Basic sociodemographic and clinical data were recorded; patients completed the SMAQ twice (administered by doctor/nurse) and self-administered the Morisky-Green scale. The analysis database included 144 patients that met selection criteria and that provided the required data. Descriptive characteristics for all recorded parameters and psychometric characteristics of the questionnaire (reliability and validity) were studied. Results: Mean age in the sample was 50.63 (12.44) years, 60.42% were men. Some 20.14% of patients had sub-target tacrolimus levels (<5ng/ml), and unjustified variations in immunosuppressive drug levels were reported for 13.48%. Regarding SMAQ results, 39.01%/41.84% of patients were non-adherent (doctor/nurse administration); 22.38% according to the Morisky-Green scale. Interobserver agreement (kappa) was 0.821 (P<.001). The Cramer’s-V statistic for convergent validity was 0.516 (P<.001). SMAQ scores were associated with unjustified variations in tacrolimus levels. In the prediction of tacrolimus levels (target vs subtarget), SMAQ compared to Morisky-Green provided a better classification of patients, with greater sensitivity and lower specificity. Conclusion: The questionnaire provides good levels of validity and interobserver agreement. An enhanced sensitivity is advantageous to better detect non-adherent patients for a better follow-up.
INTRODUCTION
Non-adherence in transplant patients is, to some degree, a direct cause of or at least a factor associated with graft loss and death.1-3 Non-adherence also has repercussions on the quality of life of transplant patients, as well as on the health costs associated with the underlying disease, usually in the form of needing a second transplant and dialysis.4-6
The estimated percentage of transplant patients that are non-compliant with treatment regimens ranges between 20% and 54%.1,7,8 In renal transplants, the lack of compliance is estimated to contribute to 20% of acute rejections and 16% of graft losses.7
Among the factors associated with a lack of adherence to immunosuppressive treatment are age, depression, stress, the number of doses per day, secondary effects of the immunosuppressive therapy, a lack of trust in the medication prescribed, low patient autonomy, having received the graft from a live donor, and a deficient cultural concept of health care.4,7,9
Because of the clinical importance of adherence, it should be closely monitored in routine clinical protocols for solid organs recipients.10 The level of adherence is especially important in renal transplant recipients, since the rate of patients that do not comply with immunosuppressive treatment protocols is higher in this group that in those that receive other types of transplants.11
Adherence can be measured using an objective measurement (direct observation of the medications used) or through indirect methods such as measuring the quantity of medication in blood or serum samples, biological markers, or electronic monitoring. There are also subjective measurements, such as medical opinion or patient testimony. There is no consensus on an optimal procedure for measuring adherence in clinical practice. However, it was shown that the combined use of subjective and indirect methods provides a highly sensitive measure for estimating compliance.12
The Simplified Medication Adherence Questionnaire (SMAQ) is a short and simple tool based on questions posed directly to the patient regarding his/her medication-taking habits, which was originally validated for the measurement of adherence in patients on anti-retroviral treatment.13 In the field of nephrology, this tool has been used for evaluating compliance with phosphate-binding treatment in haemodialysis patients, although it has not been validated for this group of patients.14,15 In this study, we present the validation of an SMAQ questionnaire that has been adapted for use in transplant patients. Our objective was to produce a tool that is applicable in routine clinical practice, both alone and in combination with indirect methods, for detecting transplant patients that are at risk for non-compliance with the prescribed immunosuppressive medication, so as to increase the control and minimise the possible adverse effects.
PATIENTS AND METHOD
Ours was an observational epidemiological study evaluating the psychometric properties of the Simplified Medication Adherence Questionnaire (SMAQ) in renal transplant recipients.
We planned to recruit a total of 150 renal graft recipients that had undergone kidney transplant at least one year before their inclusion in the study. With the objective of maximising the homogeneity of the sample and avoiding the excessive variability associated with the immunosuppressive regimens normally used in solid organ transplant recipients, we limited our study to patients receiving tacrolimus, thus reducing the possible prescriptions to those involving combinations of this drug with other immunosuppressants commonly associated with it.
The selection criteria used were the following: patients 18 years of age or older, with a renal transplant of at least 12 months evolution, and on immunosuppressive therapy with tacrolimus. We also considered it to be a fundamental requirement for participation in the study and data collection that the patient be informed of the goals and methods of the study and voluntary sign the written informed consent form.
The basic socio-demographic and clinical data were collected from each patient by the specialist doctor. Each patient completed the Morisky-Green scale16 and the SMAQ, the latter involving two independent interviews carried out on the same day, one by the specialist doctor and one by the nursing staff.
The Morisky-Green scale is a simple scale involving only 4 items that ask the patient how he/she complies with the medication regimen prescribed by the doctor. This scale allows us to classify patients as compliant or non-compliant. It has been properly validated in Spain.17
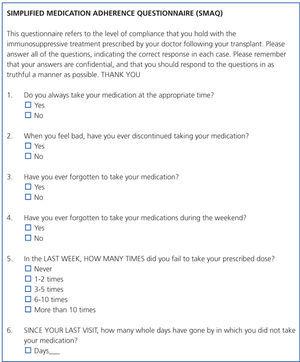
The SMAQ questionnaire was developed as a modification of the Morisky-Green questionnaire to measure adherence to antiretroviral treatment in patients with acquired immunodeficiency syndrome (AIDS). This questionnaire consists of six questions that evaluate different aspects of patient compliance with treatment: forgetfulness, routine, adverse effects, and a quantification of omissions. A patient is classified as non-compliant if he/she responds to any of the questions with a non-adherence answer, and in terms of quantification, if the patient has lost more than two doses during the last week or has not taken medication during more than two complete days during the last three months. This questionnaire was validated in a sample of Spanish patients under treatment with unboosted nelfinavir between 1998 and 1999.13 The SMAQ questionnaire subject to validation (Figure 1) was a Spanish version adapted for use in transplant patients. The adaptation process took place through expert consultations, along with a patient/expert panel.
Statistical analysis
The data were entered into a database created specifically for this purpose using STATA statistical software, version 10, which was submitted to ranges and internal coherence rules in order to control incoherence and/or corrections in the collection and tabulation of the data. The preliminary database included 146 cases received by the closing date. Later, we performed quality control checks on the data, reviewing and correcting any incomplete or incorrect data. Additionally, we performed an analysis of compliance with the inclusion criteria “patient with a kidney transplant of at least 12 months post-transplant evolution,” based on the timespan between the transplant date and the first visit for the study. This analysis led to the removal of two cases that had less than one year with their transplants. The resulting database that we analysed consisted of a total of 144 cases.
With respect to the analysis, we used a statistical significance value (α) of 0.05 in all exploratory and analytical statistical tests. We also described the sample in terms of the different socio-demographic and clinical variables collected during the study.
In the analysis of the psychometric properties of the SMAQ questionnaire, we studied the inter-observer reproducibility using Cohen’s kappa coefficient as a measure of reliability. In the validity analysis, we analysed the association between the results of the questionnaire and the different clinical variables related to adherence. We also examined the sensitivity and specificity of the questionnaire (as compared to the Morisky-Green scale) in detecting non-compliant patients, using the level of tacrolimus in blood samples as our gold standard, with sub-target concentrations being those less than 5ng/ml. Finally, the convergent validity of the survey was evaluated using an analysis of the association between questionnaire scores and those from the Morisky-Green scale.
We performed all statistical analyses using STATA statistical software, version 10. The analyses were based on the number of entries given for each specific item, such that we never assigned values to items with lost values. The scores from the questionnaires, and thus the analyses that involved the management of these scores, were calculated only for those patients that had responded to all of the items for the questionnaire considered.
RESULTS
As we mentioned previously, the database that we analysed included 144 adult patients that had received a kidney transplant at least one year before their inclusion in the study, and who were undergoing immunosuppressive therapy with tacrolimus.
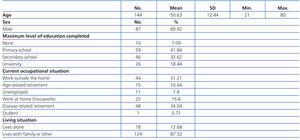
Table 1 describes the sample in terms of socio-demographic variables. The mean patient age in our sample was 50.63 years, and the sample was composed primarily of males.
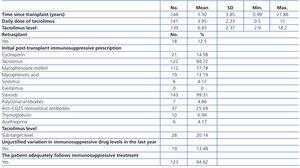
The mean time elapsed between the transplant and the first visit for inclusion in our study was 5.30 years (Table 2). The minimum time registered was 0.99 years, since one patient was considered valid as only a few days were needed in order to comply with the 1-year inclusion criteria. The patients underwent a second transplant in 12.5% of cases. Tacrolimus was prescribed as an initial post-transplant immunosuppressive therapy in 84.72% of cases, and 99.31% received steroids. The mean daily dose of tacrolimus prescribed upon inclusion in the study was 3.95mg, and mean levels were 6.83ng/ml. Based on the lower limit value for tacrolimus of 5ng/ml, 20.14% of patients had sub-target levels. According to the attending physicians, 13.48% of patients had unjustified variations in immunosuppressive drug levels during the year prior to the initial visit for our study, and 94.62% had adequately followed their immunosuppressive treatment protocols.
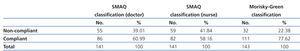
Table 3 shows how patients were classified according to their responses to the two questionnaires. According to the SMAQ questionnaire, 39.01% of patients were classified as non-compliant when the survey was administered by the doctor, and 41.84% when administered by the nursing staff. The Morisky-Green scale determined that 22.38% of patients were non-compliant.
For the analysis of the psychometric properties of the SMAQ questionnaire, we first studied the level of concordance between the SMAQ scores for the two different interviews administered. As shown in Table 4, the level of concordance between the results from the interview with the doctor and the interview with the nurse was quite high, suggesting a very good inter-observer reproducibility.
We examined the convergent validity using the association between the classification produced by the SMAQ questionnaire for both interviews and the score from the Morisky-Green scale. As shown in Table 5, a moderate level of correlation exists between the two scales. Regarding the criteria validity, this same table shows the negative association between adherence as measured by the SMAQ questionnaire and the unjustified variations in immunosuppressive drug levels. There was also an almost significant relationship between the classification provided by the SMAQ questionnaire and the attending physician’s impression of the proper compliance on the part of the patient with the immunosuppressive protocol.
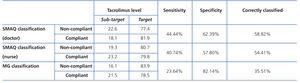
We also examined the sensitivity and specificity of the questionnaire in detecting non-compliant patients using the gold-standard of the tacrolimus concentration in blood samples (Table 6). If we compare it to the Morisky-Green scale, the SMAQ questionnaire provides a greater sensitivity and lower specificity, as well as a higher percentage of correctly classified patients.
DISCUSSION
In this study, we attempted to validate a version of the SMAQ questionnaire in order to obtain a simple instrument for detecting transplant patients that are not complying with immunosuppressive treatment in normal clinical practice in Spain.
The questionnaire has adequate values of validity and inter-observer reproducibility.
Previous studies showed that the mean non-compliance with immunosuppressive treatment is 28% in kidney transplant patients, according to patient testimony.7 According to the results from our study, the adapted SMAQ has classified a higher percentage of non-compliant patients than the established mean, whereas the Morisky-Green scale classified a lower number as non-compliant. The percentage of non-compliant patients according to the SMAQ in this study was also higher than the rate from the original validation study for compliance with anti-retroviral treatment in patients with AIDS,13 although our rate was similar to published values for adherence to phosphate-binding medication in haemodialysis patients.14,15
Using tacrolimus levels in blood samples as our gold standard, the SMAQ questionnaire provides a higher sensitivity and lower specificity than the Morisky-Green scale. A higher sensitivity is advantageous in a tool such as this, since it provides a greater power of detection of non-compliant subjects and thus leads to better clinical follow-up. As a limitation to the study, we should point out that, although we obtained a favourable tendency, the values obtained for sensitivity and specificity as compared to the classification using target/sub-target tacrolimus concentrations is far below the desired range for a tool of this type, and below the results obtained in the original validation using the results from a medication monitoring system as a gold standard.13 This is probably due to the nature of the gold standard used in our study, since the values obtained using the Morisky-Green scale were also far below the expected range.
We should also point out that, although the results from the SMAQ questionnaire were associated with medical opinion on patient adherence, the rate of non-compliant patients according to the medical reports did not reach 6%, whereas the rate based on the questionnaire exceeded 39% (22%, according to the Morisky-Green scale). On the other hand, over 20% of patients had sub-target tacrolimus values in blood samples. The differences between professional perception and the results from the tests and analyses are in accordance with the common under-detection rates of poor adherence in this type of patient,18 which shows the need for a compliance measurement tool that is applicable in daily practice for a better detection and follow-up of non-compliant patients.
As regards the analysis of the psychometric properties of the questionnaire, the level of inter-observer concordance was higher than that obtained in the original validation of the questionnaire.13 The questionnaire also exhibits adequate convergent and criteria validity, by being correlated with the Morisky-Green scale and the clinical parameters analysed, which leads us to conclude that the adapted SMAQ questionnaire had adequate psychometric properties –reliability and validity– for detecting transplant patients that are non-compliant with immunosuppressant medication in normal clinical practice.
Table 1. Socio-demographic variables
Table 2. Clinical data
Table 3. Patient classification according to questionnaire responses
Table 4. Inter-observer reproducibility
Table 5. Criteria validity analysis
Table 6. Characteristics of the questionnaires in predicting sub-target tacrolimus values
Figure 1. SMAQ questionnaire adapted for use in transplant patients