We hypothesized that a poorer cardiovascular health status is related to a higher risk of hypertension-mediated organ-damage (HMOD) or hypertension-related comorbidities (HRC). We assessed the relationship between cardiovascular health metrics (CVHM) and HMOD-HRC in 243 hypertensive patients from primary care center followed for two years. We recorded the baseline CVHM score (Life's Simple 7) plus clinical data, including prevalent and incident HMOD-HRC, hospitalization and mortality. The prevalence of ideal CVHM scores was very low in both men and women. The patients with healthier CVHM scores were younger, and had a lower prevalence of diabetes, cardiovascular disease and chronic kidney disease. We recorded 264 cases of HMOD-HRC (225 at baseline and 39 during follow-up). Nine patients died and 64 had any-cause hospitalization during follow-up. A lower prevalence of HMOD-HRC and unfavorable outcomes was observed as the number of ideal CVHM increased (P<0.05). Multivariate logistic regression adjusted for confounders showed a lower CVHM score (0–1) was associated with increased odds of HMOD-HRC (4.04, 95% CI 1.26–12.94; P=0.019) and composite endpoint (HMOD-HRC, death or all-cause hospitalization) (3.43, 95% CI 1.19–9.92; P=0.023). Individual components were less predictive than the cumulative CVHM score. Few hypertensive patients in this urban population had ideal CVHM scores. An inverse relationship between scores and outcomes (HMOD-HRC, death or hospitalizations) was observed. Interventions to increase this score may improve prognosis among community-based hypertensive patients.
Nuestra hipótesis fue que un estado de peor salud cardiovascular está relacionado con un mayor riesgo de daño orgánico provocado por la hipertensión (DOP HTA) o de comorbilidades relacionadas con la hipertensión (CRHTA). Evaluamos la relación entre las métricas de la salud cardiovascular (MSCV) y el DOP HTA-CRHTA en 243 pacientes hipertensos procedentes de un centro de atención primaria, a quienes se realizó un seguimiento durante 2 años. Registramos la puntuación basal de MSCV (Life's Simple 7) y los datos clínicos, incluyendo DOP HTA-CRHTA prevalente e incidental, hospitalización y mortalidad. La prevalencia de puntuaciones MSCV ideales fue muy baja tanto en hombres como en mujeres. Los pacientes con puntuaciones MSCV más saludables fueron más jóvenes y tuvieron una menor prevalencia de diabetes, cardiopatías y enfermedad renal crónica. Registramos 264 casos de DOP HTA-CRHTA (225 al inicio y 39 durante el seguimiento). Nueve pacientes fallecieron y 64 fueron hospitalizados por cualquier causa durante el seguimiento. Se observó una menor prevalencia de DOP HTA-CRHTA y resultados no favorables a medida que aumentaba el MSCV ideal (p<0,05). La regresión logística multivariante ajustada a los factores de confusión reflejó una menor puntuación MSCV (0-1) asociada a un incremento de la odds ratio de DOP HTA-CRHTA (4,04, IC 95% 1,26-12,94; p=0,019) y un resultado compuesto (DOP HTA-CRHTA, muerte u hospitalización por cualquier causa) (3,43, IC 95% 1,19-9,92; p=0,023). Los componentes individuales fueron menos predictivos que la puntuación MSCV acumulada. Pocos pacientes hipertensos de esta población urbana tuvieron puntuaciones MSCV ideales. Se observó una relación inversa entre las puntuaciones y los resultados (DOP HTA-CRHTA, muerte u hospitalizaciones). Las intervenciones para incrementar esta puntuación pueden mejorar el pronóstico entre los pacientes hipertensos con base comunitaria.
Arterial hypertension has a high prevalence in the general population and is a major risk factor for cardiovascular diseases (CVD).1,2 Hypertension-mediated organ damage (HMOD), i.e., stroke, left ventricular hypertrophy (LVH), abnormal ankle-brachial index (ABI), and chronic kidney disease (CKD), substantially increases the risk of hypertension-related comorbidities (HRC), including overt CVD, such as coronary artery disease (CAD), heart failure, atrial fibrillation, stroke, peripheral vascular disease (PVD), and CKD or its progression as well as mortality, even in well-controlled hypertension.3–6 Indeed, large observational studies have demonstrated independent associations between hypertension and each of these outcomes. Additionally, controlled clinical trials of antihypertensive drugs have shown impressive reductions in cardiovascular events.7,8
The American Heart Association (AHA) has developed a metric, termed Life's Simple 7 (LS7), for defining and promoting ideal cardiovascular health metrics (CVHM).9 The LS7 includes four modifiable health behaviors (body mass index [BMI]<25kg/m2, physical activity, a healthy diet and nonsmoking) and three modifiable biological factors (untreated total cholesterol<200mg/dL, untreated blood pressure<120/80mmHg and untreated fasting blood glucose<100mg/dL). Achievement of the ideal in these metrics has been associated with improved CVD-free survival and a reduction in healthcare costs.10–12
A priori, the burden of cardiovascular disease risk factors is high among individuals with hypertension. Although hypertensive patients share many risk factors included in the LS7, the relationship between having an ideal risk factor profile in the LS7 plus other community risk factors and HMOD and HRC has not been thoroughly assessed. Thus, considering the increased morbidity and mortality as well as high healthcare costs associated with hypertension, identifying and treating these modifiable health behaviors and health factors could decrease hypertension-related life-threatening complications.
We hypothesized that a poorer cardiovascular health status is related to a higher risk of HMOD and HRC. Thus, we aimed to assess in a population-based cohort of hypertensive patients from an urban primary care center the association between the individual and combined factors that comprise the LS7, determined at baseline, and the presence of HMOD-HRC, recorded at the beginning of the study and during the two years of follow-up. Finally, we also assessed the relationship between ideal CVH plus other community risk factors, such as poverty, alcohol consumption, marital status and educational attainment,13–15 and adverse hypertensive patient outcomes.
MethodsStudy populationThe study included a community-based population of consecutive adult Caucasian hypertensive patients who were examined between September 2018 and September 2019 in an urban health care center (La Cuesta, La Laguna, Tenerife, Spain) and who gave their informed consent. Thus, both prevalent hypertensive patients and incident hypertensive subjects during the recruitment period were included. All patients were diagnosed with primary hypertension. Follow-up was censored up to the end of the observation period (2 years after baseline assessment), or at the time of death. Thus, all surviving patients were followed for at least 24 months from their study inclusion. The study protocol was approved by the institutional review board of a tertiary hospital in Spain (University Regional Hospital of Málaga) and is in accordance with the Declaration of Helsinki.
Data collectionSocio-demographic information, including community risk factors, medical history, and information about medications (antihypertensive, cholesterol-lowering, and glucose-lowering drugs) were obtained from self-reported questionnaires. Baseline characteristics included age, sex, weight and height, waist-to-height ratio, marital status (married/cohabiting, single or religious, divorced or separated and widowed), low annual household income (<25,000€), alcohol intake (low, moderate and high), nocturnal work, and education (primary school or less, secondary school, and college or university). A family history of CVD, diabetes, hypertension or cancer was also reported. Additionally, we recorded baseline preexisting HMOD (stroke, LVH abnormal ABI and CKD) and HRC, including nonfatal atherosclerotic events (CAD, stroke and symptomatic PVD), atrial fibrillation, heart failure and CKD,6 defined by self-reported prior physician diagnosis of each comorbidity. We also determined the presence of left ventricular hypertrophy (LVH) by electrocardiographic criteria, using a Sokolow–Lyon index (SV1+RV5/RV6, mm) greater than 35mm,16 and the ABI by an improved automated oscillometric device, the MESI MD®, which has recently been validated as a screening tool for the diagnosis de PVD in the general population.17 ABI measurements ≤0.9 were considered as occlusive PVD.
Baseline laboratory data included estimated glomerular filtration rate (eGFR), calculated by the MDRD equation, serum total cholesterol, HDL cholesterol, LDL cholesterol, triglycerides, fasting glucose, serum HbA1C, and serum high-sensitivity C-reactive protein (hs-CRP) concentrations, as well as the albumin-to-creatinine ratio in spot urine. CKD was defined on the basis of at least two ambulatory eGFR measurements<60ml/min/1.73m2 or an albumin-to-creatinine ratio>30mg/g measured on at least two occasions more than 3 months apart.
We also ascertained both HMOD and HRC at the study end according to clinical practice guidelines.6 CAD was defined as myocardial infarction (documented by elevated enzyme levels, with or without electrocardiography) or coronary artery revascularization, as adjudicated by a trained physician using standard criteria.18 Atrial fibrillation and LVH were ascertained by electrocardiography. Heart failure was identified by hospitalization or an emergency department visit plus proper treatment for a clinical syndrome presenting with signs and symptoms in consistence with cardiac decompensation or inadequate cardiac pump function. Stroke was diagnosed as a persistent central neurological deficit lasting at least 24h and unexplained by other causes. Finally, PVD was considered as the need for a revascularization procedure or amputation or ABI≤0.9. CKD progression was defined as a 50% decrease in eGFR from baseline or occurrence of end-stage renal disease. Lastly, we assessed all-cause hospitalizations and mortality from any cause during follow-up.
Life's Simple 7We used the AHA definition of CVH based on 7 metrics.9 The 7 metrics were as follows: (1) Body mass index (kg/m2), computed from weight in a scrub suit and standing height; (2) Smoking status (current, former, or never smokers), derived from interviews; (3) Diet score, based on fish, fruit and vegetable consumption, and sodium, sugar, and fiber/carbohydrate ratio intake according to the modified, 66-item Harvard Food Frequency questionnaire.19 An ideal diet was defined as meeting four or five of the following criteria: fish consumption≥2 servings/wk, fruit/vegetables≥4.5 cups/d, sodium intake<1500mg/d, sugar<450kcal/wk, and fiber/carbohydrate ratio>0.1; (4) Physical activity using the Baecke questionnaire (none, 1–3 times per week and ≥4 times per week; (5) Blood pressure, recorded three times in a seated position using a random-zero sphygmomanometer after five minutes rest, and the mean of the last two measurements used for the analysis; (6) Fasting total cholesterol, assessed by enzymatic methods; and (7) Fasting glucose, using the hexokinase/glucose-6-phosphate dehydrogenase method. Each metric was categorized into three levels as poor, intermediate, or ideal (Table S1).
In addition to using all 7 factors for a composite LS7 score, the seven health factors were grouped into their two domains (health behaviors: cigarette smoking, physical activity, diet, and body mass index; health factors: blood pressure (BP), cholesterol, and glucose).
Consistent with the LS7 scoring approach, hypertensive patients on treatment who achieved their goal levels for BP (systolic BP<140mmHg and diastolic BP<90mmHg), cholesterol (total cholesterol<200mg/dL), and glucose (serum glucose<126mg/dL) were placed in the intermediate health category.
We generated binary categories for each metric (i.e., ideal vs. not ideal) and computed an overall CVHM score (0–7) by allocating 1 point for each ideal category and 0 points for intermediate or poor status: ideal physical activity (vs. less than ideal or inactive), past or never smoker (vs. current smoker), healthy diet score of 4–5 (vs. 0–3), BMI of 20–25kg/m2 (vs. 25–30, or ≥30kg/m2), total-cholesterol<200mg/dL not on treatment (vs. 200–239mg/dL or treated to goal, or ≥240mg/dL), and fasting blood glucose<100mg/dL not on treatment (vs. 100–125mg/dL or treated to goal, or ≥126mg/dL). Because all patients had hypertension, no patient had the ideal blood pressure category according to the LS7 scoring. The score for each individual CVHM was then summed to yield the total CVHM score.
Study outcomesThe primary outcome in our study was the presence of HMOD and/or HRC (HMOD-HRC), preexisting or incident during follow-up. In addition, the status of all patients was assessed and data on mortality and any-cause hospitalization were also obtained for the entire cohort at the end of the follow-up. Thus, we generated one additional composite endpoint that included: global HMOD-HRC (preexisting and incident) and all-cause mortality or any-cause hospitalization because the CVHM score has also been associated with multiple vascular and nonvascular conditions.20
Statistical analysesCategorical variables were reported as frequency and percentage whereas continuous variables were reported as mean (SD) or median and interquartile range. Inter-group comparisons of quantitative variables were made by Student's t-test or the Mann–Whitney U test as appropriate. Categorical variables were compared using the chi-square test or Fisher's exact test. Correlations between clinical parameters were performed by univariate regression analysis. The distribution of each LS7 component as poor, intermediate, or ideal and the percent of participants with zero through seven ideal factors were calculated. Subjects were classified into groups with 0–1, 2–3 and ≥4 ideal CVHM scores as very few participants had extreme values, at either the lower (0) or upper (5) ends of the range. Additionally, we calculated the prevalence of the combination of HMOD plus HRC by level of each LS7 factor as the proportion of cases in our study population over a specified period of time (from diagnosis of hypertension until study end). Baseline characteristics were compared across the LS7 health categories (poor, intermediate and ideal) using one way ANOVA for continuous variables and chi-square tests for categorical variables. Multiple logistic regression analysis was performed to test the relationship between individual and cumulative CVHM scores with the composite endpoints after adjusting for confounder variables. We also assessed the relationship between community risk factors combined with CVHM and composite endpoints. The Hosmer–Lemeshow goodness of fit was the principal criterion for selection of the final models. Statistical significance for all comparisons including interactions was defined as P<0.05. All statistical computations were undertaken using SPSS software version 20.0.
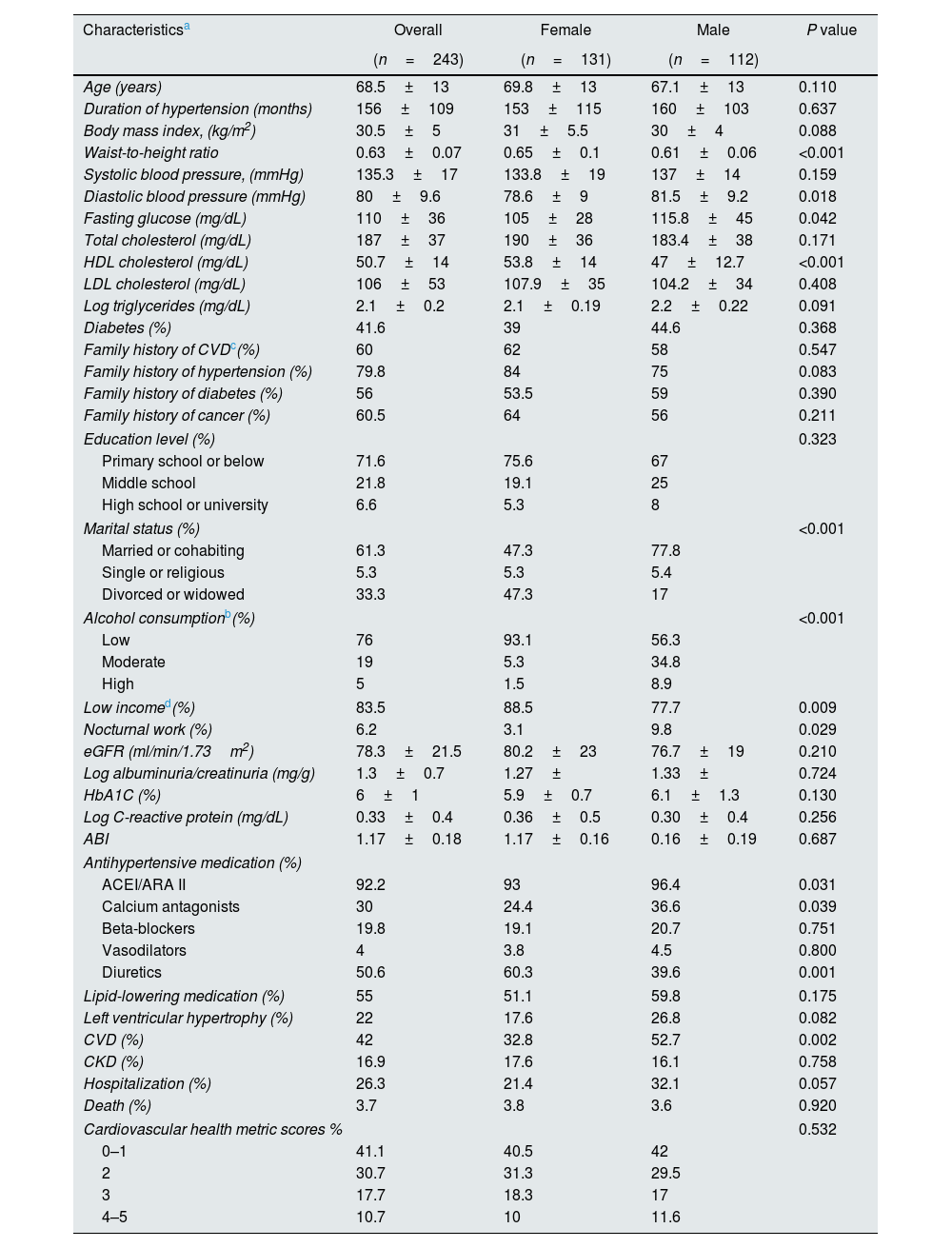
ResultsA total of 243 hypertensive patients were enrolled in this observational study, of whom 233 were prevalent hypertensive patients and 10 were incident hypertensive subjects. Table 1 shows baseline socio-demographic and clinical characteristics as well as CVHM and community risk factors in the whole study sample and stratified by gender. Overall, the mean age of the participants was 68.5±13 years and most had a low educational level and low family income, and were married or cohabiting. As expected, a family history of CVD and hypertension had a high prevalence as well as preexisting CVD. Given the study participation criteria, a high proportion of the entire cohort received ACEI/ARA II medication for blood pressure control.
Baseline characteristics of hypertensive patients.
| Characteristicsa | Overall | Female | Male | P value |
|---|---|---|---|---|
| (n=243) | (n=131) | (n=112) | ||
| Age (years) | 68.5±13 | 69.8±13 | 67.1±13 | 0.110 |
| Duration of hypertension (months) | 156±109 | 153±115 | 160±103 | 0.637 |
| Body mass index, (kg/m2) | 30.5±5 | 31±5.5 | 30±4 | 0.088 |
| Waist-to-height ratio | 0.63±0.07 | 0.65±0.1 | 0.61±0.06 | <0.001 |
| Systolic blood pressure, (mmHg) | 135.3±17 | 133.8±19 | 137±14 | 0.159 |
| Diastolic blood pressure (mmHg) | 80±9.6 | 78.6±9 | 81.5±9.2 | 0.018 |
| Fasting glucose (mg/dL) | 110±36 | 105±28 | 115.8±45 | 0.042 |
| Total cholesterol (mg/dL) | 187±37 | 190±36 | 183.4±38 | 0.171 |
| HDL cholesterol (mg/dL) | 50.7±14 | 53.8±14 | 47±12.7 | <0.001 |
| LDL cholesterol (mg/dL) | 106±53 | 107.9±35 | 104.2±34 | 0.408 |
| Log triglycerides (mg/dL) | 2.1±0.2 | 2.1±0.19 | 2.2±0.22 | 0.091 |
| Diabetes (%) | 41.6 | 39 | 44.6 | 0.368 |
| Family history of CVDc(%) | 60 | 62 | 58 | 0.547 |
| Family history of hypertension (%) | 79.8 | 84 | 75 | 0.083 |
| Family history of diabetes (%) | 56 | 53.5 | 59 | 0.390 |
| Family history of cancer (%) | 60.5 | 64 | 56 | 0.211 |
| Education level (%) | 0.323 | |||
| Primary school or below | 71.6 | 75.6 | 67 | |
| Middle school | 21.8 | 19.1 | 25 | |
| High school or university | 6.6 | 5.3 | 8 | |
| Marital status (%) | <0.001 | |||
| Married or cohabiting | 61.3 | 47.3 | 77.8 | |
| Single or religious | 5.3 | 5.3 | 5.4 | |
| Divorced or widowed | 33.3 | 47.3 | 17 | |
| Alcohol consumptionb(%) | <0.001 | |||
| Low | 76 | 93.1 | 56.3 | |
| Moderate | 19 | 5.3 | 34.8 | |
| High | 5 | 1.5 | 8.9 | |
| Low incomed(%) | 83.5 | 88.5 | 77.7 | 0.009 |
| Nocturnal work (%) | 6.2 | 3.1 | 9.8 | 0.029 |
| eGFR (ml/min/1.73m2) | 78.3±21.5 | 80.2±23 | 76.7±19 | 0.210 |
| Log albuminuria/creatinuria (mg/g) | 1.3±0.7 | 1.27± | 1.33± | 0.724 |
| HbA1C (%) | 6±1 | 5.9±0.7 | 6.1±1.3 | 0.130 |
| Log C-reactive protein (mg/dL) | 0.33±0.4 | 0.36±0.5 | 0.30±0.4 | 0.256 |
| ABI | 1.17±0.18 | 1.17±0.16 | 0.16±0.19 | 0.687 |
| Antihypertensive medication (%) | ||||
| ACEI/ARA II | 92.2 | 93 | 96.4 | 0.031 |
| Calcium antagonists | 30 | 24.4 | 36.6 | 0.039 |
| Beta-blockers | 19.8 | 19.1 | 20.7 | 0.751 |
| Vasodilators | 4 | 3.8 | 4.5 | 0.800 |
| Diuretics | 50.6 | 60.3 | 39.6 | 0.001 |
| Lipid-lowering medication (%) | 55 | 51.1 | 59.8 | 0.175 |
| Left ventricular hypertrophy (%) | 22 | 17.6 | 26.8 | 0.082 |
| CVD (%) | 42 | 32.8 | 52.7 | 0.002 |
| CKD (%) | 16.9 | 17.6 | 16.1 | 0.758 |
| Hospitalization (%) | 26.3 | 21.4 | 32.1 | 0.057 |
| Death (%) | 3.7 | 3.8 | 3.6 | 0.920 |
| Cardiovascular health metric scores % | 0.532 | |||
| 0–1 | 41.1 | 40.5 | 42 | |
| 2 | 30.7 | 31.3 | 29.5 | |
| 3 | 17.7 | 18.3 | 17 | |
| 4–5 | 10.7 | 10 | 11.6 | |
Abbreviations: ABI, ankle brachial index; ACEI/ARA II, angiotensin-converting enzyme inhibitors or angiotensin receptor antagonists; CKD, chronic kidney disease; CVD, cardiovascular disease; eGFR, estimated glomerular filtration rate.
Women, who comprised 54% of the study sample, had a higher waist-to-height ratio, BMI, and HDL-cholesterol level. Conversely, diastolic blood pressure and fasting glucose were significantly lower in the females than males. In addition, males had a higher family income, were more often married, had more nocturnal work and a higher alcohol consumption. Finally, CVD was more prevalent in male subjects.
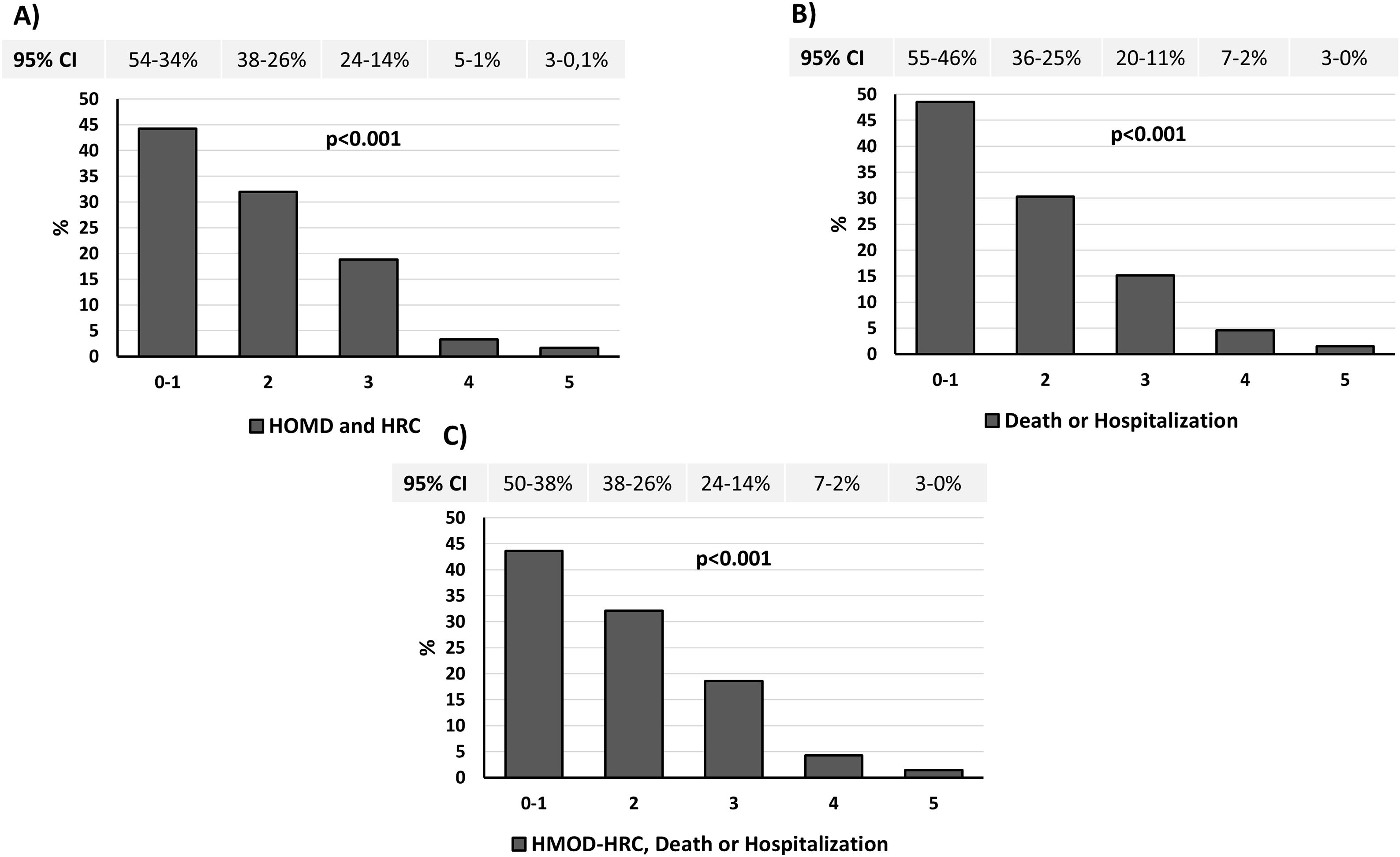
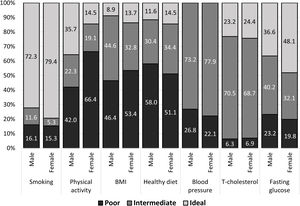
Baseline characteristics according to the Life's Simple 7 factorsThe distribution of poor, intermediate and ideal LS7 component scores by gender is presented in Fig. 1. Smoking and blood glucose were the most common ideal health components in both genders, whereas an ideal BMI and healthy dietary pattern were the least common. Due to the study design, no patient had an ideal blood pressure level. Only three patients presented 5 ideal CVHM scores. Lastly, women had numerically higher ideal scores than men in all components except for ideal physical activity that was significantly higher in men (P<0.001).
Baseline socio-demographic and clinical characteristics according to the different LS7 component scores are shown in Tables S2 and S3. As compared to current smokers, participants who never smoked were older and had lower triglyceride levels. Compared with inactive patients, individuals with an ideal physical activity were more likely to be male and had a lower BMI and waist-to-height ratio. As compared to individuals with a BMI≥30kg/m2, subjects with a BMI<25kg/m2 had higher HDL-cholesterol levels and a lower prevalence of diabetes as well as lower HbA1c and hs-CRP levels. Interestingly, a significant correlation between hs-CRP and BMI was also observed in the whole population (r=0.282; P=0.0001). Compared to individuals with a poor diet, patients with an ideal diet were older and had a lower diastolic pressure (Table S2). As compared to individuals with poor fasting glucose levels, patients with ideal glucose levels were younger, had a higher educational level and a lower prevalence of CVD and LVH, showed lower triglyceride levels and had a lower albuminuria/creatinine ratio and HbA1c levels as well as higher levels of total-, LDL- and HDL-cholesterol, and were treated with fewer lipid-lowering drugs. Compared to individuals with intermediate or poor cholesterol levels, participants with ideal cholesterol levels were younger and had a lower prevalence of CVD and lower triglyceride levels. Finally, compared to individuals with poor blood pressure, subjects with intermediate blood pressure control had a lower systolic blood pressure (Table S3).
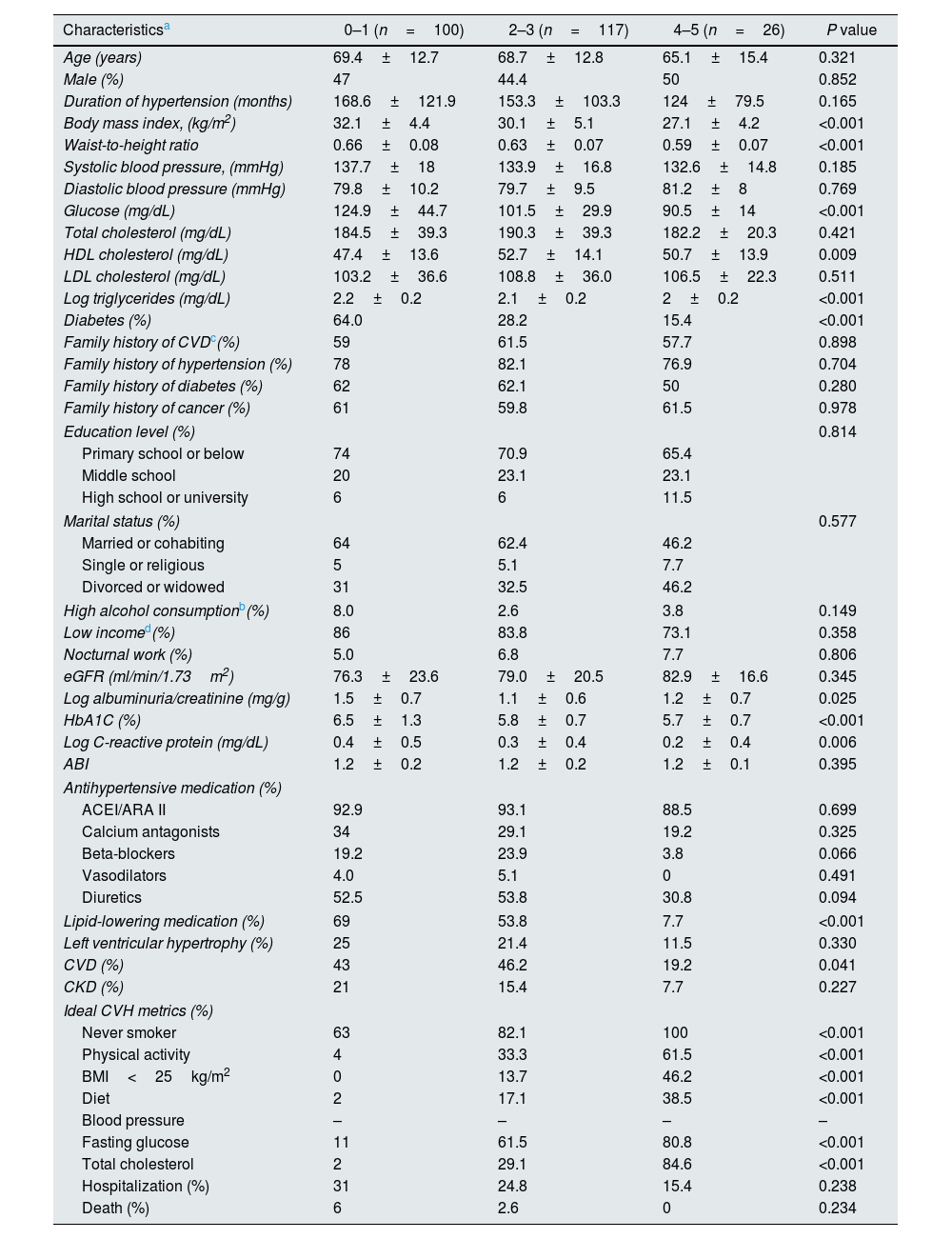
Cardiovascular health metric score distributionThe median CVHM score in the entire population was 2 (interquartile range 1–3). The distribution of the CVHM scores was as follows: 100 (41.1%) had a score of 0–1; 117 (48.1%) had a score of 2–3; and 26 (10.7%) had a score of 4–5. Table 2 shows the clinical characteristics and community risk factors according to grouped CVHM scores. Compared to patients with a score of 0–1, those with more healthy LS7 components were more likely to be younger and had a lower BMI and waist-to-height ratio, as well as lower glucose, triglyceride and hs-CRP levels, and presented a lower prevalence of diabetes and CVD and a trend to a lesser prevalence of CKD. Of note, hs-CRP levels were inversely correlated with CVHM scores (r=−0.155; P=0.016).
Baseline clinical characteristics of study population by CVHM score categories.
| Characteristicsa | 0–1 (n=100) | 2–3 (n=117) | 4–5 (n=26) | P value |
|---|---|---|---|---|
| Age (years) | 69.4±12.7 | 68.7±12.8 | 65.1±15.4 | 0.321 |
| Male (%) | 47 | 44.4 | 50 | 0.852 |
| Duration of hypertension (months) | 168.6±121.9 | 153.3±103.3 | 124±79.5 | 0.165 |
| Body mass index, (kg/m2) | 32.1±4.4 | 30.1±5.1 | 27.1±4.2 | <0.001 |
| Waist-to-height ratio | 0.66±0.08 | 0.63±0.07 | 0.59±0.07 | <0.001 |
| Systolic blood pressure, (mmHg) | 137.7±18 | 133.9±16.8 | 132.6±14.8 | 0.185 |
| Diastolic blood pressure (mmHg) | 79.8±10.2 | 79.7±9.5 | 81.2±8 | 0.769 |
| Glucose (mg/dL) | 124.9±44.7 | 101.5±29.9 | 90.5±14 | <0.001 |
| Total cholesterol (mg/dL) | 184.5±39.3 | 190.3±39.3 | 182.2±20.3 | 0.421 |
| HDL cholesterol (mg/dL) | 47.4±13.6 | 52.7±14.1 | 50.7±13.9 | 0.009 |
| LDL cholesterol (mg/dL) | 103.2±36.6 | 108.8±36.0 | 106.5±22.3 | 0.511 |
| Log triglycerides (mg/dL) | 2.2±0.2 | 2.1±0.2 | 2±0.2 | <0.001 |
| Diabetes (%) | 64.0 | 28.2 | 15.4 | <0.001 |
| Family history of CVDc(%) | 59 | 61.5 | 57.7 | 0.898 |
| Family history of hypertension (%) | 78 | 82.1 | 76.9 | 0.704 |
| Family history of diabetes (%) | 62 | 62.1 | 50 | 0.280 |
| Family history of cancer (%) | 61 | 59.8 | 61.5 | 0.978 |
| Education level (%) | 0.814 | |||
| Primary school or below | 74 | 70.9 | 65.4 | |
| Middle school | 20 | 23.1 | 23.1 | |
| High school or university | 6 | 6 | 11.5 | |
| Marital status (%) | 0.577 | |||
| Married or cohabiting | 64 | 62.4 | 46.2 | |
| Single or religious | 5 | 5.1 | 7.7 | |
| Divorced or widowed | 31 | 32.5 | 46.2 | |
| High alcohol consumptionb(%) | 8.0 | 2.6 | 3.8 | 0.149 |
| Low incomed(%) | 86 | 83.8 | 73.1 | 0.358 |
| Nocturnal work (%) | 5.0 | 6.8 | 7.7 | 0.806 |
| eGFR (ml/min/1.73m2) | 76.3±23.6 | 79.0±20.5 | 82.9±16.6 | 0.345 |
| Log albuminuria/creatinine (mg/g) | 1.5±0.7 | 1.1±0.6 | 1.2±0.7 | 0.025 |
| HbA1C (%) | 6.5±1.3 | 5.8±0.7 | 5.7±0.7 | <0.001 |
| Log C-reactive protein (mg/dL) | 0.4±0.5 | 0.3±0.4 | 0.2±0.4 | 0.006 |
| ABI | 1.2±0.2 | 1.2±0.2 | 1.2±0.1 | 0.395 |
| Antihypertensive medication (%) | ||||
| ACEI/ARA II | 92.9 | 93.1 | 88.5 | 0.699 |
| Calcium antagonists | 34 | 29.1 | 19.2 | 0.325 |
| Beta-blockers | 19.2 | 23.9 | 3.8 | 0.066 |
| Vasodilators | 4.0 | 5.1 | 0 | 0.491 |
| Diuretics | 52.5 | 53.8 | 30.8 | 0.094 |
| Lipid-lowering medication (%) | 69 | 53.8 | 7.7 | <0.001 |
| Left ventricular hypertrophy (%) | 25 | 21.4 | 11.5 | 0.330 |
| CVD (%) | 43 | 46.2 | 19.2 | 0.041 |
| CKD (%) | 21 | 15.4 | 7.7 | 0.227 |
| Ideal CVH metrics (%) | ||||
| Never smoker | 63 | 82.1 | 100 | <0.001 |
| Physical activity | 4 | 33.3 | 61.5 | <0.001 |
| BMI<25kg/m2 | 0 | 13.7 | 46.2 | <0.001 |
| Diet | 2 | 17.1 | 38.5 | <0.001 |
| Blood pressure | – | – | – | – |
| Fasting glucose | 11 | 61.5 | 80.8 | <0.001 |
| Total cholesterol | 2 | 29.1 | 84.6 | <0.001 |
| Hospitalization (%) | 31 | 24.8 | 15.4 | 0.238 |
| Death (%) | 6 | 2.6 | 0 | 0.234 |
Abbreviations: ABI, ankle-brachial index; ACEI/ARA II, angiotensin-converting enzyme inhibitors or angiotensin receptor antagonists; CKD, chronic kidney disease; CVD, cardiovascular disease; CVHM, cardiovascular health metric; eGFR, estimated glomerular filtration rate.
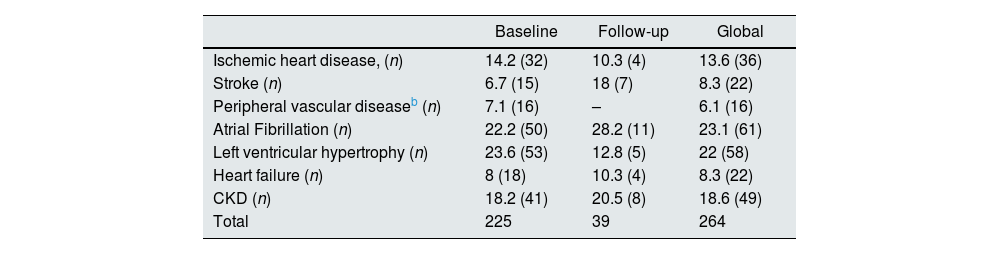
Table 3 displays HMOD-HRC at baseline and during the two-year follow-up. In the current study, we recorded a total of 264 cases of HMOD-HRC in 243 patients, of which 225 were collected in the initial assessment and 39 occurred during the follow-up. The overall crude HMOD-HRC incidence rate was 7.1 per 100-person-years (95% CI 4.1–10.1) in the entire population. In particular, patients experienced the following HMOD-HRC at follow-up: 11 atherosclerotic events (CAD and stroke), 8 CKD or progression, 4 heart failure, 11 atrial fibrillations and 5 de novo LVH. Overall, a total of 58 patients had more than one HMOD-HRC. Additionally, we recorded 9 deaths: 6 attributed to CVD, 2 due to cancer and 1 due to infectious complication. Lastly, 64 patients had any-cause hospitalization at follow-up.
Hypertension-mediated organ damage and hypertension-related comorbidities at baseline and during follow-up.a
| Baseline | Follow-up | Global | |
|---|---|---|---|
| Ischemic heart disease, (n) | 14.2 (32) | 10.3 (4) | 13.6 (36) |
| Stroke (n) | 6.7 (15) | 18 (7) | 8.3 (22) |
| Peripheral vascular diseaseb (n) | 7.1 (16) | – | 6.1 (16) |
| Atrial Fibrillation (n) | 22.2 (50) | 28.2 (11) | 23.1 (61) |
| Left ventricular hypertrophy (n) | 23.6 (53) | 12.8 (5) | 22 (58) |
| Heart failure (n) | 8 (18) | 10.3 (4) | 8.3 (22) |
| CKD (n) | 18.2 (41) | 20.5 (8) | 18.6 (49) |
| Total | 225 | 39 | 264 |
Abbreviations: CKD, chronic kidney disease.
Data are provided as percentage, and in parentheses the total number.
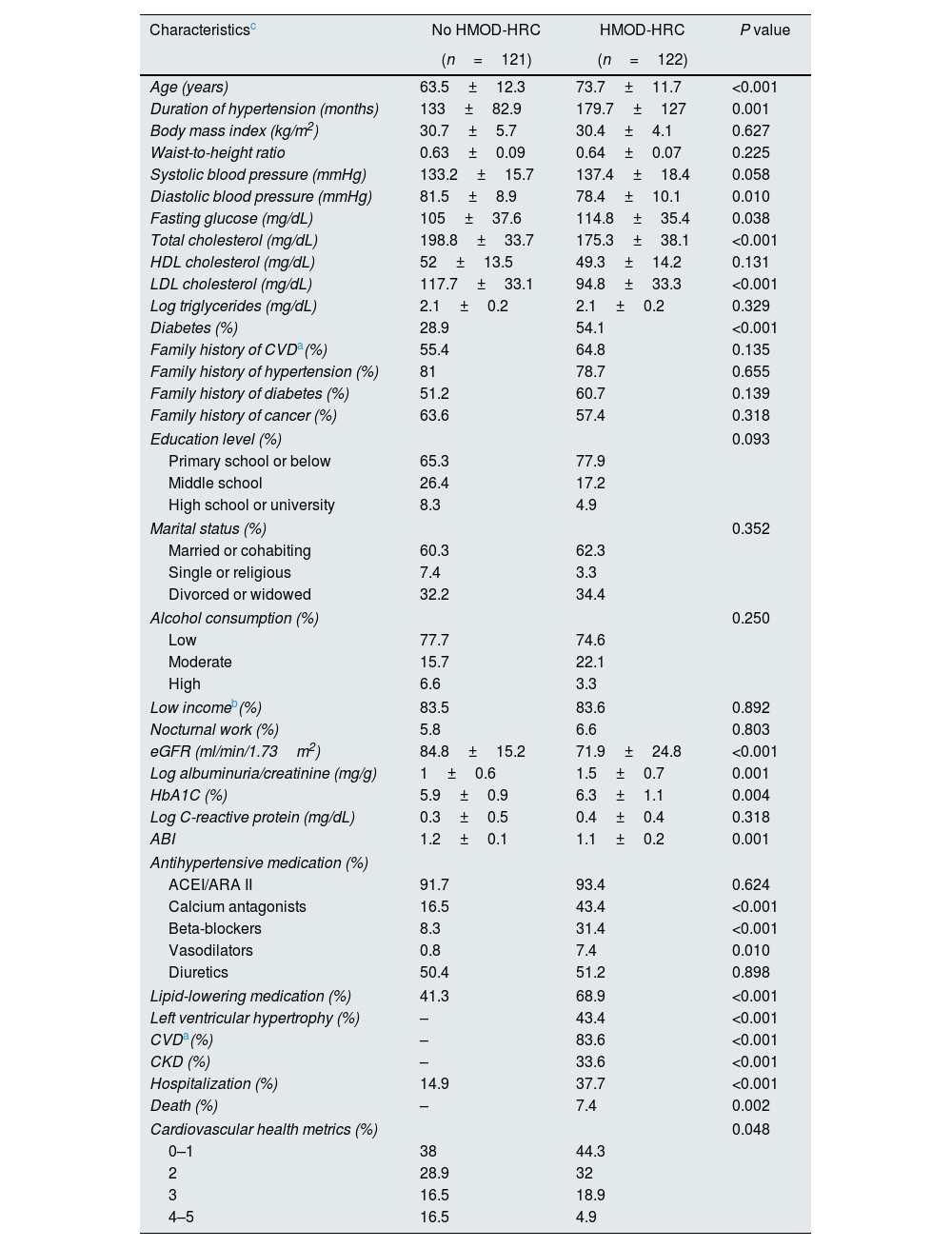
Table 4 shows comparisons between patients with and without HMOD-HRC. As expected, patients with HMOD-HRC were older, had a longer history of hypertension and a higher proportion had diabetes, as well as a lower GFR and higher albuminuria/creatinine ratio and HbA1c levels. Likewise, they received a higher proportion of lipid-lowering medication because they had a worse lipid profile before inclusion in the study. Consequently, total- and LDL-cholesterol levels were significantly lower in the HMOD-HRC group at baseline assessment. A higher proportion of ideal CVHM scores was observed in patients without HMOD-HRC. Finally, patients with HMOD-HRC had a greater proportion of any-cause hospitalization and all deaths occurred in those with HMOD-HRC.
Characteristics of patients with and without hypertension-mediated organ damage and hypertension-related comorbidities.
| Characteristicsc | No HMOD-HRC | HMOD-HRC | P value |
|---|---|---|---|
| (n=121) | (n=122) | ||
| Age (years) | 63.5±12.3 | 73.7±11.7 | <0.001 |
| Duration of hypertension (months) | 133±82.9 | 179.7±127 | 0.001 |
| Body mass index (kg/m2) | 30.7±5.7 | 30.4±4.1 | 0.627 |
| Waist-to-height ratio | 0.63±0.09 | 0.64±0.07 | 0.225 |
| Systolic blood pressure (mmHg) | 133.2±15.7 | 137.4±18.4 | 0.058 |
| Diastolic blood pressure (mmHg) | 81.5±8.9 | 78.4±10.1 | 0.010 |
| Fasting glucose (mg/dL) | 105±37.6 | 114.8±35.4 | 0.038 |
| Total cholesterol (mg/dL) | 198.8±33.7 | 175.3±38.1 | <0.001 |
| HDL cholesterol (mg/dL) | 52±13.5 | 49.3±14.2 | 0.131 |
| LDL cholesterol (mg/dL) | 117.7±33.1 | 94.8±33.3 | <0.001 |
| Log triglycerides (mg/dL) | 2.1±0.2 | 2.1±0.2 | 0.329 |
| Diabetes (%) | 28.9 | 54.1 | <0.001 |
| Family history of CVDa(%) | 55.4 | 64.8 | 0.135 |
| Family history of hypertension (%) | 81 | 78.7 | 0.655 |
| Family history of diabetes (%) | 51.2 | 60.7 | 0.139 |
| Family history of cancer (%) | 63.6 | 57.4 | 0.318 |
| Education level (%) | 0.093 | ||
| Primary school or below | 65.3 | 77.9 | |
| Middle school | 26.4 | 17.2 | |
| High school or university | 8.3 | 4.9 | |
| Marital status (%) | 0.352 | ||
| Married or cohabiting | 60.3 | 62.3 | |
| Single or religious | 7.4 | 3.3 | |
| Divorced or widowed | 32.2 | 34.4 | |
| Alcohol consumption (%) | 0.250 | ||
| Low | 77.7 | 74.6 | |
| Moderate | 15.7 | 22.1 | |
| High | 6.6 | 3.3 | |
| Low incomeb(%) | 83.5 | 83.6 | 0.892 |
| Nocturnal work (%) | 5.8 | 6.6 | 0.803 |
| eGFR (ml/min/1.73m2) | 84.8±15.2 | 71.9±24.8 | <0.001 |
| Log albuminuria/creatinine (mg/g) | 1±0.6 | 1.5±0.7 | 0.001 |
| HbA1C (%) | 5.9±0.9 | 6.3±1.1 | 0.004 |
| Log C-reactive protein (mg/dL) | 0.3±0.5 | 0.4±0.4 | 0.318 |
| ABI | 1.2±0.1 | 1.1±0.2 | 0.001 |
| Antihypertensive medication (%) | |||
| ACEI/ARA II | 91.7 | 93.4 | 0.624 |
| Calcium antagonists | 16.5 | 43.4 | <0.001 |
| Beta-blockers | 8.3 | 31.4 | <0.001 |
| Vasodilators | 0.8 | 7.4 | 0.010 |
| Diuretics | 50.4 | 51.2 | 0.898 |
| Lipid-lowering medication (%) | 41.3 | 68.9 | <0.001 |
| Left ventricular hypertrophy (%) | – | 43.4 | <0.001 |
| CVDa(%) | – | 83.6 | <0.001 |
| CKD (%) | – | 33.6 | <0.001 |
| Hospitalization (%) | 14.9 | 37.7 | <0.001 |
| Death (%) | – | 7.4 | 0.002 |
| Cardiovascular health metrics (%) | 0.048 | ||
| 0–1 | 38 | 44.3 | |
| 2 | 28.9 | 32 | |
| 3 | 16.5 | 18.9 | |
| 4–5 | 16.5 | 4.9 | |
Abbreviations: ABI, ankle-brachial index; ACEI/ARA II, angiotensin-converting enzyme inhibitors or angiotensin receptor antagonists; CKD, chronic kidney disease; CVD, cardiovascular disease; eGFR, estimated glomerular filtration rate. HMOD-HRC, hypertension-mediated organ damage and/or hypertension-related comorbidities.
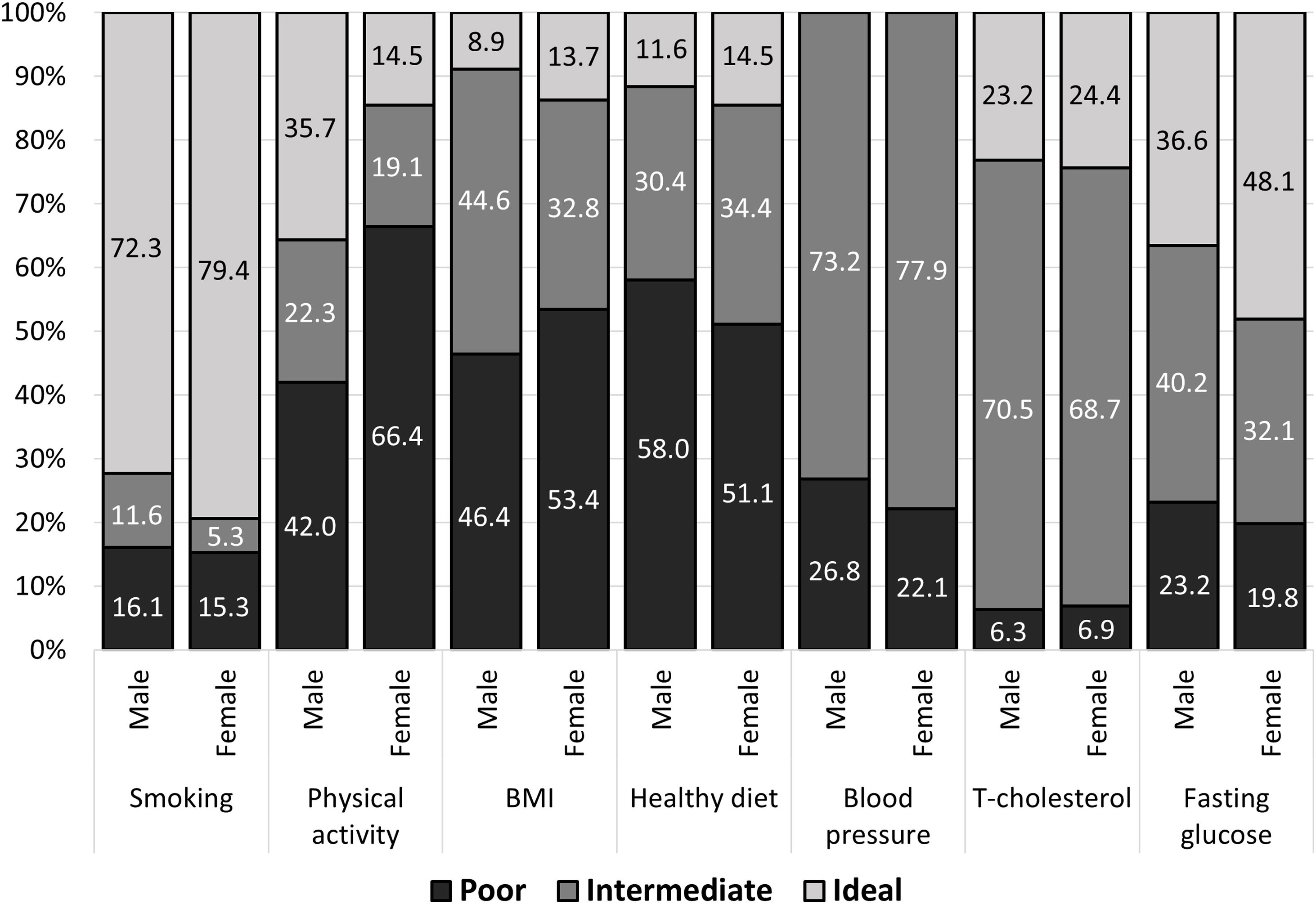
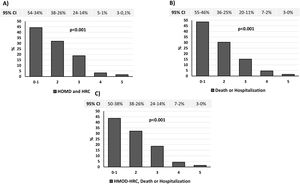
Fig. 2A displays a significantly lower prevalence of HMOD plus HRC as the number of ideal CVHM scores increased. Similarly, the prevalence of death and any-cause hospitalization (Fig. 2B), and the composite endpoint that included mortality, all-cause hospitalization and HMOD-HRC were also lower as the number of ideal CVHM scores increased (Fig. 2C).
Prevalence of HMOD plus HRC (A), death or any-cause hospitalization (B) and HMOD or HRC, death or all-cause hospitalization (C) according to the number of ideal CVHM. Data are provided as percentage and 95% confidence interval. Abbreviations: CVHM, cardiovascular health metrics. HMOD, hypertension-mediated organ damage; HRC, hypertension-related comorbidities.
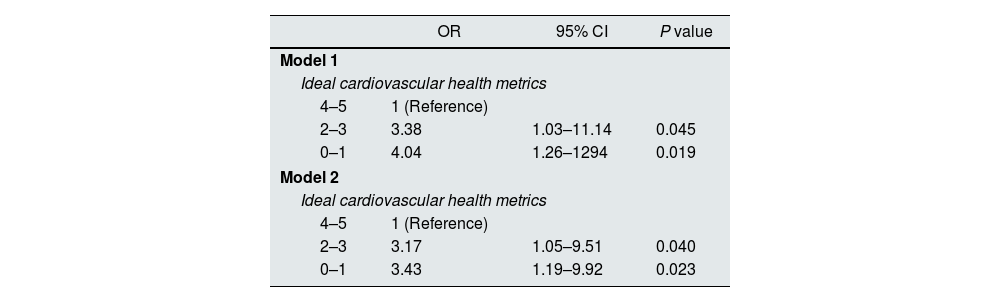
In an age- and sex-adjusted logistic regression analysis, individual CVHM components were not associated with either the presence of HMOD-HRC or the composite endpoint (HMOD-HRC, death or any-cause hospitalization) (Table S4). However, in a fully multivariate logistic regression adjusted for confounders (Table 5), the risk of HMOD-HRC significantly increased as the number of ideal CVHM scores decreased, using subjects with 4 to 5 ideal CVHM scores as the reference (Model 1). Similarly, when the composite endpoint used as dependent variable was death, hospitalization or HMOD-HRC, again subjects with lower CVHM scores had significantly higher odds of the composite endpoint (Model 2).
Multivariate logistic regression for associations between number of ideal cardiovascular health metrics and hypertension-mediated organ damage or hypertension-related comorbidities and mortality and all-cause hospitalization.
| OR | 95% CI | P value | |
|---|---|---|---|
| Model 1 | |||
| Ideal cardiovascular health metrics | |||
| 4–5 | 1 (Reference) | ||
| 2–3 | 3.38 | 1.03–11.14 | 0.045 |
| 0–1 | 4.04 | 1.26–1294 | 0.019 |
| Model 2 | |||
| Ideal cardiovascular health metrics | |||
| 4–5 | 1 (Reference) | ||
| 2–3 | 3.17 | 1.05–9.51 | 0.040 |
| 0–1 | 3.43 | 1.19–9.92 | 0.023 |
Adjusted for: Age, sex, duration of hypertension, ankle-brachial index, family history of cardiovascular disease, low income, education level, marital status, alcohol consumption, HbA1c, hs-PCR and hypertensive medication. Model 1, dependent variable used was: hypertension-mediated organ damage (HMOD) or hypertension-related comorbidities (HRC). Model 2, dependent variable used was: HMOD or HRC or death or all-cause hospitalization. (Hosmer–Lemeshow test: Model 1, P=0.114; Model 2, P=0.227).
The main findings of this prospective study are: (1) an overall very low prevalence of ideal CVHM scores was seen in hypertensive patients from an urban population. This finding was mainly driven by unhealthy behaviors, and was similar between men and women; (2) patients with a greater number of ideal CVHM scores had in general a more favorable state of biological and metabolic factors and a graded and reduced risk for adverse outcomes, including HMOD-HRC, mortality and any-cause hospitalizations; and (3) the presence of poorer cumulative ideal CVHM scores (0–1) was associated with unfavorable outcomes in this particular population. These findings suggest that an optimal CVH status could help to reduce the risk of HMOD-HRC. This is one of just a few studies to evaluate thoroughly the association between a combination of healthy lifestyle factors and modifiable biological factors plus other community-risk factors and HMOD-HRC in the setting of hypertensive patients from an urban population.
In 2010, the AHA defined the concept of ideal CVHM, since when an increasing number of studies in the general population have suggested that adherence to various healthy lifestyle factors and biological factors is related to better clinical outcomes.21–28 However, an important number of reports in different populations have found that the prevalence of ideal CVHM was extremely low (<3%).29–35 Consistent with previous studies, we also found that the prevalence of ideal CVHM was very low in hypertensive patients from an urban population. Our patients were classified into groups with 0–1, 2–3 and ≥4 ideal CVHM scores as very few participants had extreme values, either the lower (0) or upper (5) ends of the range. This allowed for a reasonable number of participants in each risk group. No patients presented 6 or 7 ideal CVHM factors and only three patients had 5 ideal CVHM. In fact, given the study design no patient presented an ideal level of blood pressure. This suggests that behavior changes required for compliance with the ideal CVHM are difficult targets to achieve, especially in an aging population. Indeed, our study comprised a mostly elderly population with a high prevalence of other well-known vascular risk factors such as BMI>30kg/m2 (50.2%), diabetes (41.6%) or the presence of CKD (16%), which could have contributed to the scarcity of healthy factors and healthy behaviors in our patients. Thus, recommendations for the general population, included in CVHM, might not apply to an elderly hypertensive population with a high burden of unhealthy behaviors and lifestyles, like in the current study.
Hypertension has a high prevalence in the general population (∼50%) and comprises an important risk factor for HMOD-HRC,36 which in turn leads to unfavorable outcomes. Additionally, many hypertension-related risk factors are included in the LS7. It is expected, therefore, that a poor cardiovascular health status, evaluated through the measurement system of the AHA, which combines 4 health behaviors and 3 vascular risk factors, could contribute to the life-threatening complications of this disease. In fact, the positive assessment of these seven estimates has been associated with a decrease in the risk of CVD and a lower rate of global and cardiovascular mortality in multiple observational studies.10,12,33,37 Individuals with 5–7 ideal CVHM have a much lower rate of cardiovascular entities and cardiovascular mortality, as well as all-cause mortality than those with 0–1 ideal CVHM. Conversely, those with a lower number of ideal CVHM have an increased risk of hypertension-mediated comorbidities and any-cause mortality.38 In the current study, we assessed the relationship between behavior factors plus health factors and HMOD-HRC and unfavorable outcomes in hypertensive patients, mostly aging, in whom multiple well-known vascular risk factors coexist. It is plausible to think, thus, that these patients were less likely to possess beneficial CVH components and consequently possess fewer ideal CVHM, leading to an increased risk of HMOD-HRC and poorer outcomes. In this line, our patients with more healthy LS7 components were more likely to be younger and had a higher number of ideal healthy behaviors and biological factors than those with fewer ideal CVHM. As a result, we observed a lower prevalence of HMOD plus HRC as well as a lesser mortality and any-cause hospitalization as the number of CVHM increased gradually.
Interestingly, hs-CRP levels declined with the increase in the number of CVHM. Additionally, hs-CRP levels were negatively associated with the number of CVHM in our hypertensive population. This is consistent with previous reports.39,40 Hs-CRP may play an important role in the incidence and progression of hypertension, and hs-CRP levels increase if other comorbidities are present in hypertensive patients, such obesity or metabolic syndrome.41,42
Individual ideal CVHM were not associated with the study endpoints. Consistent with our findings, previous reports also found no association with ideal BMI, healthy diet score, desirable cholesterol levels or HbA1c levels, especially when other comorbidities are present.25,43–45 This suggests that ideal CVH components can act collaboratively rather than individually, mainly in patients with multiple comorbidities, including those with hypertension. In other words, the excess risk of HMOD-HRC among hypertensive patients may be explained by the clustering of other cardiovascular risk factors associated with hypertension. Of note, we found that patients with a lower cumulative ideal CVHM score (0–1) had a higher risk for HMOD-HRC. In particular, the risk for HMOD-HRC increased 3–4 times in those patients with ≤3 CVH components compared with individuals with 4–5 ideal CVHM after adjusting for potential confounding factors such as age, sex, duration of hypertension, parental history of CVD, poverty, alcohol consumption, marital status, educational levels, ABI, hs-CRP, HbA1c and hypertensive medication. Likewise, meeting a lower number of cardiovascular health metrics also appeared to be associated with a higher risk for the composite endpoint that included HMOD-HRC, death or all-cause hospitalization. In consonance with our findings, many observational studies provide strong evidence to support the beneficial effects of cumulative ideal CVHM on CVD incidence and mortality in the general population and in patients with other cardiovascular comorbidities, including hypertension.25,27,33,45–47 With this background, preventative efforts to reduce HMOD-HRC should implement strategies promoting a more holistic approach, focusing on a combination of cardiovascular risk factors to achieve optimal vascular health, which may yield greater benefits than would be expected by targeting individual CVH components independently.
Data from the current study were not available to assess whether changes in cardiovascular health actually reduce HMOD-HRC risk, as documented.48 Previous reports have demonstrated in both diabetic and nondiabetic patients that intensive multifactorial interventions aimed at reducing cardiovascular risk factors (achieving lower blood pressure, lipid treatment goals, ACEI use and aspirin use) were associated with a substantially lower incidence of nephropathy, progression of retinopathy and progression of neuropathy as well as a lower CVD rate and all-cause mortality.49,50 Whether these goals could be achieved in hypertensive patients is, at the moment, uncertain and further large prospective observational studies are needed to elucidate this concern.
The findings from the present study should be interpreted within the context of known and potential limitations. Results of our study may not be generalized to other populations with a different context, age, race and lifestyle culture. Our patients were mostly old, had several comorbidities and came from an urban population, which may also have led to selection bias. Indeed, populations in rural areas are unique compared with those in metropolitan areas. Additionally, due to the self-reported nature of the data collected, social desirability bias was also likely. This could also underestimate the impact of CVHM on outcome. Likewise, we studied a relatively small sample of hypertensive patients and perhaps future studies with a larger sample size are needed in this particular population. Finally, the data from this study cannot elucidate whether changes in health measures can actually reduce HMOD-HRC and mortality.
Despite these limitations, our study also has some strengths. We performed an observational study and collection of baseline data was broad and complete using a standardized questionnaire. There were no missing data in the current study. In addition, we followed strictly not only the recommendations of the 7 AHA ideal metrics as previously reported, but also recorded other community risk factors such as family income, nocturnal work, education level or alcohol consumption, which could have a negative influence on CVHM.
The results from the current study using the AHA metrics demonstrate that these measurements are useful for assessing unfavorable outcomes in a high-risk population (hypertensive individuals) to suggest prevention efforts. Consequently, the systematic assessment of healthy behaviors and modifiable biological factors in this particular population could serve as an enhanced tool for clinical practice to counsel patients about those risk factors and to address with community-based hypertension prevention programs. Clinical and public health efforts should be aimed at fomenting the ideal CVHM to further improve prevention of CVD and mortality in hypertensive populations. In this way, early detection of hypertension and adequate blood pressure treatment, control of obesity and overweight, providing ideal diet and advising physical activity, stopping smoking and using modern therapeutic strategies to manage diabetes and dyslipidemia can minimize HMOD-HRC, mainly in elderly hypertensive patients.
ConclusionsIn conclusion, our findings show a low prevalence of ideal CVHM in hypertensive patients from an urban population who have a high burden of well-known cardiovascular risk factors. An inverse relationship between CVHM scores and outcomes (HMOD-HRC, death or hospitalizations) was observed. Therefore, intervention studies aimed to increase this score may improve prognosis among community-based hypertensive patients.
FundingThis study was supported in part by the Spanish Ministry of Economy and Innovation (grant PI17/02043 and grant ICI21/00042) from the Instituto de Salud Carlos III co-funded by the Fondo Europeo de Desarrollo Regional-FEDER (REDinREN, RD16/0009/0006, RD16/0009/0031 and RICORS, RD21/0005/0012).
Conflicts of interestThe authors declare no conflict of interest.
The authors thank the team of health professionals from La Cuesta Primary Healthcare Centre (La Laguna, Tenerife, Spain). We also thank Ian Johnstone for linguistic assistance in the preparation of the text.