Living donor kidney transplantation is a crucial treatment for chronic kidney disease, yet it raises significant ethical issues. This systematic review addresses these issues by analysing scientific literature from the past ten years. The objectives include identifying and thoroughly analysing the most common ethical dilemmas, describing them, examining the perspectives of various involved groups, and analysing clinical strategies to address them.
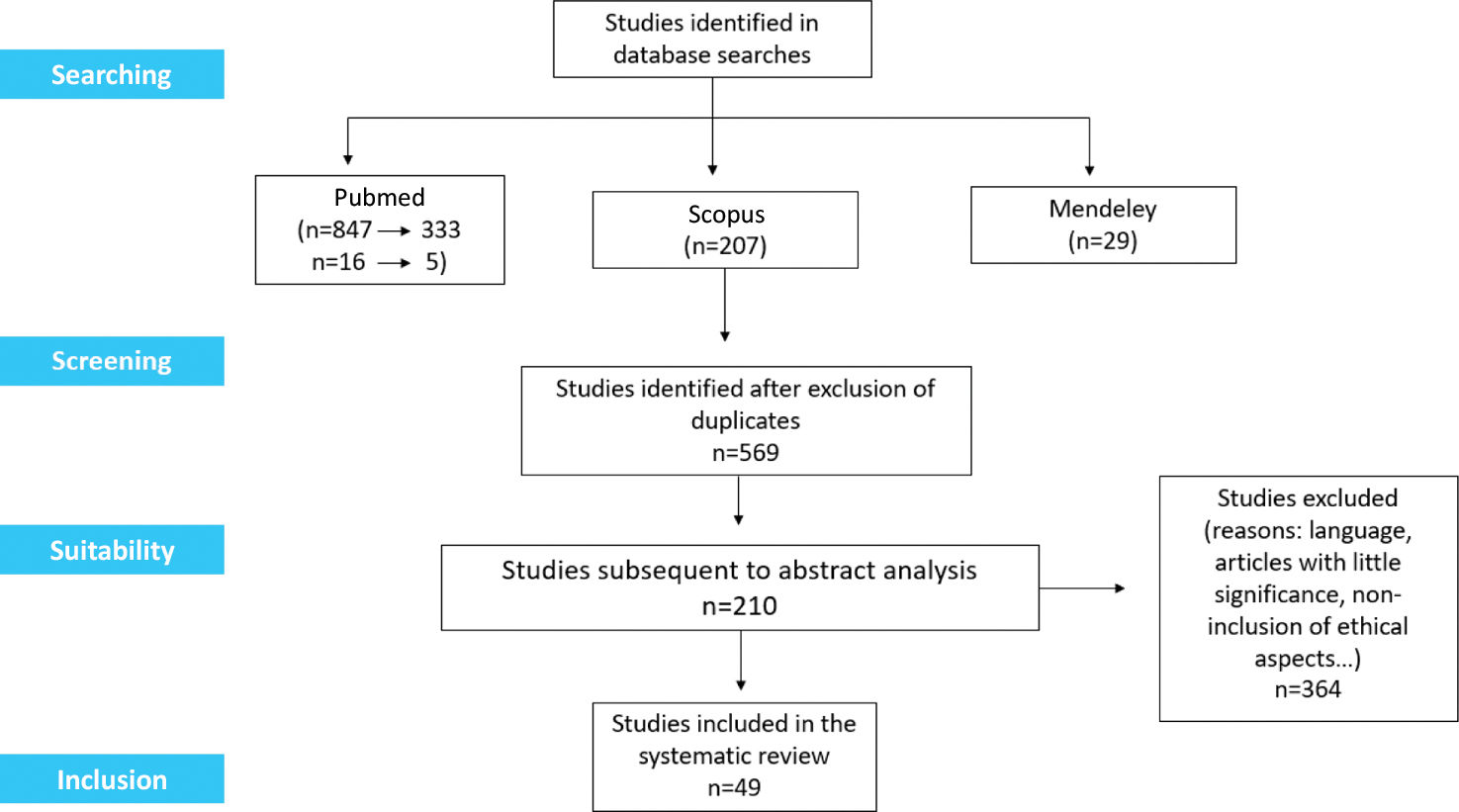
Material and methodsDatabases such as PubMed, Scopus, and Mendeley were used, following PRISMA guidelines, and 49 relevant studies were included.
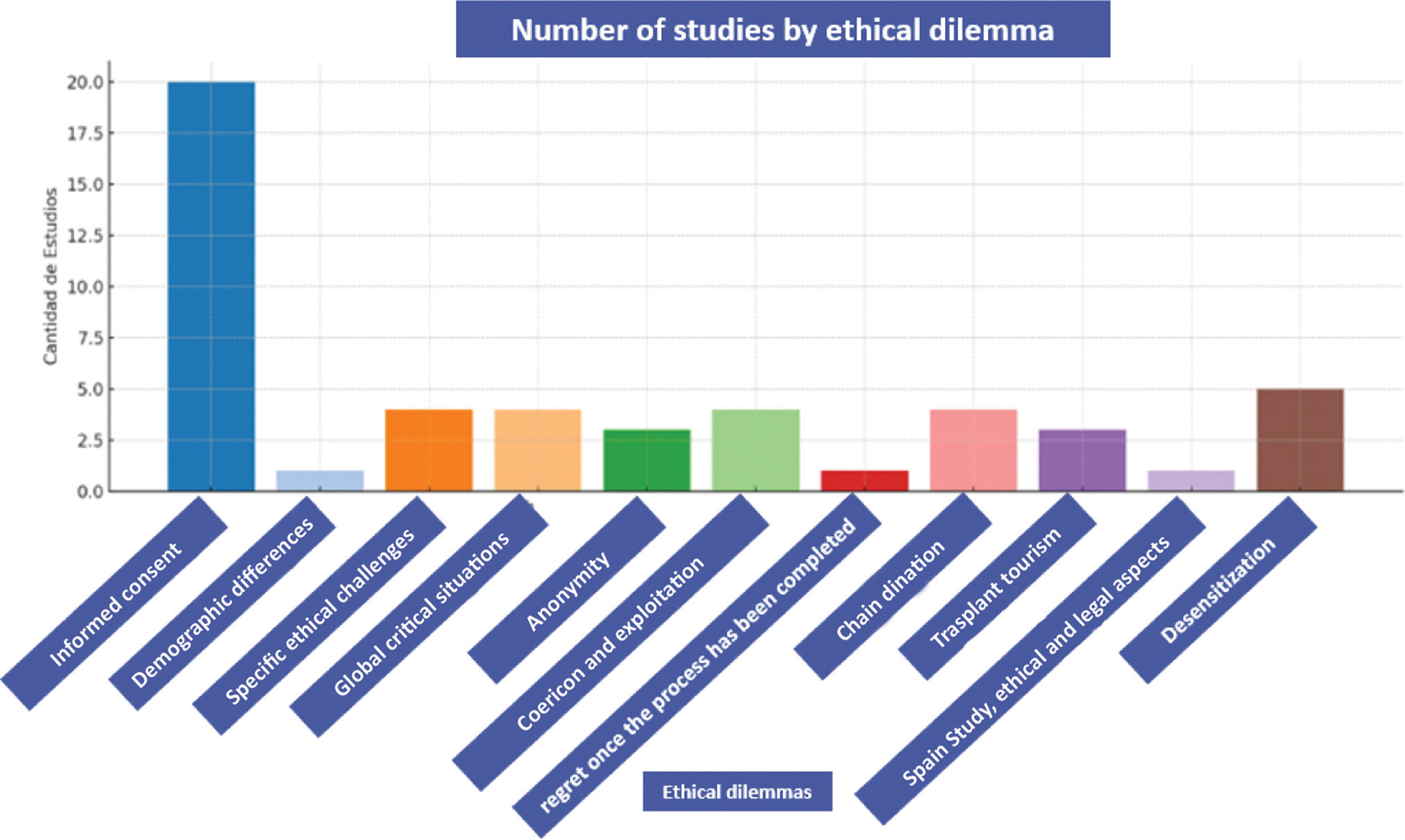
ResultsThe identified dilemmas encompass equity in access to transplantation, distributive justice, informed consent, transplant tourism, coercion, and ethical issues related to desensitization.
DiscussionThe review highlights the need for multidisciplinary approaches and unified protocols to tackle these ethical challenges. It underscores the importance of adhering to fundamental ethical principles, aligning with international bioethical statements.
El trasplante renal de donante vivo es un tratamiento crucial para la enfermedad renal crónica; sin embargo, plantea importantes cuestiones éticas. Esta revisión sistemática aborda estos problemas mediante el análisis de la literatura científica de los últimos 10 años. Los objetivos incluyen identificar y analizar en profundidad los dilemas éticos más comunes, describirlos, examinar las perspectivas de los diversos grupos involucrados y analizar las estrategias clínicas para abordarlos.
Material y métodosSe utilizaron bases de datos como PubMed®, Scopus® y Mendeley®, siguiendo las directrices PRISMA, y se incluyeron 49 estudios relevantes.
ResultadosLos dilemas identificados incluyen la equidad en el acceso al trasplante, la justicia distributiva, el consentimiento informado, el turismo de trasplantes, la coerción y las cuestiones éticas relacionadas con la desensibilización.
DiscusiónLa revisión resalta la necesidad de enfoques multidisciplinarios y protocolos unificados para abordar estos desafíos éticos. Subraya la importancia de adherirse a principios éticos fundamentales, en concordancia con las declaraciones internacionales de bioética.
The kidney transplant from a living donor is an essential intervention to treat end-stage renal disease, a condition of great relevance in Europe and worldwide, affecting millions of people. Various factors such as diabetes, hypertension, obesity, and population aging contribute to the increase in this condition. This transplant modality stands out for its better clinical outcomes compared to deceased donor transplants, as kidneys from living donors have greater longevity, reduce the need for retransplants, shorten waiting lists, and improve patients’ quality of life, in addition to lowering overall healthcare costs. The first kidney transplant from a living donor was performed in 1954 between identical twins in the United States.1 Over time, the practice extended to non-related donors, thanks to research demonstrating similar survival rates between genetically related and unrelated donors. In Europe, the Action Plan on Organ Donation and Transplantation promoted living donation, leading to a 17% increase in the number of transplants. To increase access to kidney transplantation from living donors, it is important to consider several key aspects as: Education and information to promote kidney donation from living donors, information and education programs targeted at patients and their families are required (these campaigns should highlight the benefits of donation for the recipient and the safety for the donor), multidisciplinary work since the participation of multidisciplinary teams is fundamental in kidney transplantation. Nephrology, nursing, and psychology professionals play an essential role in identifying potential donors and optimizing procedures.2 Identified obstacles include the lack of communication between dialysis and transplant teams, the absence of standardized protocols, and cultural, linguistic, and psychosocial barriers. Furthermore, storytelling is an emerging strategy to promote kidney donation, particularly when it is based on real-life experiences of donors and recipients. This educational technique aims to reduce fears, increase understanding, and encourage acceptance of living donation. Although more studies are needed, initial results indicate that storytelling can change attitudes and behaviors. It is crucial to highlight the fundamental role of informed consent in living kidney donation. Donors must receive clear information about short- and long-term risks, surgery, and possible complications. This process must ensure the donor's full understanding and freedom to decide, free from external pressures. While surgical risks are low, it is essential for the medical team to supervise the entire process and provide psychological support before, during, and after the intervention. There are several types of living kidney donation: directed, altruistic, paired exchange donation and chain donation however, certain fundamental ethical principles that govern living kidney donation may be compromised, such as the principles of autonomy, justice, beneficence, and non-maleficence. Autonomy ensures the donor's free decision, while justice seeks equity in access to transplantation. The principles of beneficence and non-maleficence guarantee that the benefits to the recipient outweigh the risks assumed by the donor. Another major concern is the possible commercialization of organs, which is internationally prohibited. However, financial compensation or indirect benefits could compromise the autonomy of the most vulnerable donors. Regulations on living donation must prevent exploitation and protect equity and altruism.3 In global catastrophe situations like the COVID-19 pandemic, kidney transplantation practices were affected, especially living donation, as it was considered an elective surgery. Measures were adopted to reduce activity, impacting recipients’ quality of life and increasing waiting lists. Vaccination of donors and recipients was fundamental to resuming activity.4 Today, new techniques have emerged to overcome ABO incompatibility between donor and recipient, known as desensitization. This technique allows transplants even when blood types do not match. Although it involves risks associated with immunosuppression, it improves equity in transplant access and increases the availability of organs. Then, kidney transplantation from a living donor is an effective treatment alternative for chronic kidney disease. Despite ethical, legal, and operational challenges, its benefits for the recipient and society make it the most efficient option for kidney replacement. Multidisciplinary work, education, and appropriate regulation are key to its success and to promoting fair, safe, and altruistic donation. A systematic review of scientific articles analyzing the ethical dilemmas of organ donation is presented. This study aims to integrate the ethical perspective into daily clinical practice, train healthcare professionals, and highlight in the scientific literature the ethical issues that influence medical decision-making.
The aim of this study is to identify and thoroughly analyze the most common ethical dilemmas associated with living donor kidney transplantation, describing the types of ethical dilemmas identified in the literature, such as equity in access, informed consent, and conflicts of interest, examining the perspectives of different stakeholder groups, such as doctors, patients, donors, and regulators, to contextualize ethical dilemmas from various viewpoints; and analysing the strategies and protocols used in clinical practice to address these dilemmas in an ethical and fair manner.
Material and methodsA systematic review of the literature was conducted following the PRISMA model, consulting the Pubmed, Scopus, and Mendeley databases. A combined search strategy was used with MeSH terms and keywords related to ethical dilemmas in living donor kidney transplantation. The included studies had to address ethical dilemmas related to living donor kidney transplantation, be published in peer-reviewed scientific journals, and be written in English, Italian, or Spanish. Studies that did not focus on ethical dilemmas, abstracts, editorials, letters to the editor, or those not available in full text were excluded (Fig. 1). The study selection was performed in two stages: first, titles and abstracts were reviewed, and then full texts of the studies meeting the inclusion criteria were examined. A single reviewer performed the selection, and discrepancies were resolved by consulting a second reviewer. Information was extracted on the year of publication, study location, title, objective, study design, research methods, results, and conclusions. In Pubmed, 847 results were identified, of which 22 studies were selected. In Scopus, 207 results were obtained, with 15 studies selected, and in Mendeley, 29 results were identified, with 7 studies selected. In total, 49 studies were selected for the review (Table 1). The review was conducted in accordance with international ethical standards, such as the Declaration of Helsinki and the Declaration of Oviedo, ensuring respect for autonomy, informed consent, data confidentiality, and risk minimization. Although ethical committee approval was not required for this study, the fundamental ethical principles for scientific research were followed. Local regulations on data protection and good clinical practices were also considered, maintaining an ethical approach throughout all stages of the review.
Selected papers in the systematic review.
| Study | Country | Year | Design | Objectives | Method of research | Results |
|---|---|---|---|---|---|---|
| 1. “Ethical issues in increasing living kidney donations by expanding kidney paired exchange programs”Ross LF, et al.23 | USA | 2000 | Literature review | Discuss ethical issues in increasing living donations through kidney donor exchange programs. | Analysis of articles on ethics and Programs exchange of donors. | - Increasing living donations with exchange raises ethical questions. |
| 2. “Ethical and Legal Aspects of Transplantation living donor kidney: Management and coordination of the living donation”Perea M, et al.21 | Spain | 2005 | Literature review | To analyze the ethical and legal aspects of living kidney donation. | Analysis of articles and documents on Ethics and legislation in kidney donation. | - Living kidney donation raises complex ethical and legal questions.- Ethical management is needed and coordinated process. |
| 3. “Ethical issues in living donor kidney transplantation”Mazaris E, et al.24 | United Kingdom | 2006 | Narrative Review | To examine ethical issues in living-donor kidney transplantation. | Review of the literature and analysis of common ethical dilemmas. | - Risks to the living donor- Equity in organ allocation Informed consent |
| 4. “Ethical issues surrunding high-risk Kidney Recipients: implications for the living donor”O’Hara JF Jr, et al.25 | USA | 2007 | Literature review | Analyze the ethical issues of recipients of high risk in Kidney transplant with a living donor. | Analysis of articles and documents on Ethics in kidney donation. | - High-risk recipients pose dilemmas ethical because of the risk to the donor.- Detailed informed consent is needed. |
| 5. “Ethical issues with nondirected (“good samaritan”) kidney donation for transplantation”Petrini C, et al.26 | Italy | 2011 | Literature review | Evaluate the ethical aspects of donation non-directed renal kidney (“Good Samaritan”) for transplantation. | Analysis of articles, reports and relevant documents. | - Undirected kidney donation poses challenges unique ethical requirements, such as obtaining the consent informed, justice in organ allocation and potential donor exploitation.- Clear ethical guidelines and protective measures are needed to Guarantee the donation undirected renal is ethically responsible. |
| 6. “The evolving approach to ethical issues in living donor kidney transplantation: A review based on illustrative case vignettes”Venkat KK, et al.27 | USA | 2014 | Descriptive study: Case Series | Analysis of the possible ethical issues raised in the TRDV | Review of a series of cases | Ethical principles found in each case:- Beneficence- Non-maleficence- Non-paternalism- Autonomy |
| 7. “Ethical challenges in nephrology: a call for action”Martin DE, et al.28 | International | 2017 | Narrative Review | Identify the most common ethical challenges in nephrology and propose strategies to address them. | Literature review and case study analysis. | 10 common ethical challenges were identified, including the consent informed, the limitation of effort, the resource allocation and the end of life. The authors proposed A number of strategies to address these challenges, including the improving education and training, Development of guidelines ethics and the promotion of research in nephrology ethics. |
| 8. “Advanced donation programs and deceased donorinitiated chains—2 innovations in kidney paired donation”Wall AE, et al.29 | USA | 2017 | Narrative Review | Analyze two innovations in the kidney donation by Exchange: Advanced Programs and Chains initiated by a deceased donor. | Literature review and analysis of approaches novel in renal exchange. | - Increased compatibility between Donors and recipients- Increasing complexity in program management |
| 9. “Advanced Donation Programs and Deceased DonorInitiated Chains—2 Innovations in Kidney Paired Donation”Wall AE et al.30 | USA | 2017 | Literature review | Discuss ethical issues in programs advanced donation and chains started by deceased donors in peer donation. | Analysis of articles on ethics and programs advanced peer donation. | - Advanced peer giving programs raise new ethical questions. |
| 10. “The Journal of Medicine and Philosophy: A Forum for Bioethics and Philosophy of Medicine”Samuel J Kerstein, et al.31 | United Kingdom | 2017 | Literature review | To analyze equity in kidney donation through vouchers. | Analysis of the concept of kidney vouchers and the impact on equity. | - Kidney vouchers could exacerbate inequities existing in access to transplantation.- Herself need alternative solutions to guarantee a fair distribution of donated kidneys. |
| 11. “ABO-incompatible kidney transplantation: an update on clinical experience and ethical considerations”Cecka M, et al.16 | Multinational | 2017 | Revision | Updating clinical expertise and ethical considerations | Analysis of existing literature | Summarize results, complications, and ethical issues |
| 12. “Ethical challenges in dialysis and Transplantation: Perspectives from the developing world”Shekhani SS, et al.13 | Pakistan | 2018 | Literature review | Summarize the ethical challenges in dialysis and transplantation from the Developing world perspective. | Literature review on ethical challenges in dialysis and transplantation in developing countries low and middle income. | Low- and middle-income countries face a number of ethical challenges in dialysis and transplantation, such as lack of access to resources, disparity in care, and donor exploitation. |
| 13. “Utilization of deceased donor kidneys to initiate Living Donor Chains: Practical, ethical, and logistical issues: Practical, ethical, and logistical issues”Ferrari P, et al.32 | Italy | 2018 | Literature review | Examine practical, ethical and Logistics of using deceased donors to start live kidney donation chains. | Review of the literature and analysis of potential barriers. | The use of deceased donors to initiate chains of Living kidney donation is but there are challenges logistical and ethical factors that require an approach. |
| 14. “Kidney transplant tourism: cases from Canada”Wright L, et al.14 | Canada | 2018 | Case Studies | Describe cases of transplant tourism kidney disease in Canada and analyze their ethical implications. | Analysis of four cases of kidney transplant tourism. | Kidney transplant tourism highlights the Global inequalities in health care and raises questions on the exploitation and ethics of the organ commercialization. |
| 15. “ABO-incompatible kidney transplantation: a systematic review and meta-analysis of outcomes”Lozano-Muñoz J, et al.18 | International | 2018 | Systematic review and meta-analysis | Analyze ABO Transplant Results incompatible vs. ABO compatible | Compared studies on rates of graft and patient survival | Incompatible ABO transplants have Long-term outcomes similar to compatible ABOs |
| 16. “An ethical comparison of living kidney donation and surrogacy: understanding the relational dimension”Beier K, et al.33 | Germany | 2019 | Qualitative study | To study and link the ethical discourses of the surrogacy, and the TRDV | Comparative analysis | Common points and other ethical dilemmas for TRDV:- Relational stability- Altruism is considered natural in TRDV- Unresolved reciprocity |
| 17. “International travel for living donor kidney donation: A proposal for focused screening of vulnerable groups”Hartsock, et al.8 | USA | 2019 | Qualitative study | To study possible situations of organ trafficking in the United States and Setting ethical boundaries | Ethical analysis | - Ethical dilemmas about the donor “bought” from a foreign country.- Less easy to identify cases of coercion.- The willingness to enter a country,- The US in this case can be coercive.- No care for DV not resident in the USA. |
| 18. “The 3-Step Model of informed consent for living kidney donation: a proposal on behalf of the DESCaRTES Working Group of the European Renal Association”Grossi AA, et al.19 | Europe | 2019 | Systematic review and meta-analysis | Assessing the evidence on consent models informed for the Living kidney donation and develop a recommended model | Search Bibliography at Databases Electronics, Study Analysis qualitative and quantitative. | We identified 42 studies. Consent models reported varied in terms of its complexity and content. The authors proposed a model 3-step program that includes:1) Preoperative information, 2) psychosocial evaluation and 3) final consent. |
| 19. “Living donor program crisis Management plans: Current landscape and talking point recommendations”Henderson ML, et al.34 | USA | 2019 | Descriptive review | Examine crisis management plans in Living kidney donation programs. | Survey analysis or Studies of Observation on crisis management plans. | - Lack of donor crisis management programs.- Greater concern of the transplant team in case of failure. |
| 20. “Ethical issues faced by a kidney transplant recipient”Crais E, et al.35 | USA | 2019 | Theoretical essay | Examine the ethical issues faced by kidney transplant recipients. | Analysis of the literature and experience Author's personal identity as a kidney transplant recipient. | Kidney transplant recipients face a series of ethical issues, such as gratitude to the donor, responsibility for the graft care and the possibility of graft rejection. |
| 21. “Deceased donor initiated chains: First Report of a successful deliberate case and its ethical implications”Furian L, et al.36 | Italy | 2019 | Case report | Describe the first deliberate case of donor-initiated chain deceased and analyze its ethical implications. | Analysis of a successful case of kidney donation chain initiated by a deceased donor. | Kidney donation chains initiated by deceased donors are feasible and can increase access to transplantation. However, they raise questions ethics that require continuous debate |
| 22. “Travel for transplantation and transplant commercialism in Argentina: a 4-decade experience from a University Hospital”Rodríguez-Reimundes E, et al.37 | Argentina | 2019 | Qualitative study | Explore transplant travel experiences and commercialism of transplants in Argentina. | Patient interviews, health professionals and government representatives. | The transplant journey and the commercialism of transplants propose Ethical concerns and challenges in access equitable health care. |
| 23. “Ethical considerations in ABO-incompatible kidney transplantation”,Sander D, et al.17 | USA | 2019 | Revision | Discuss ethical considerations | Discusses ethical issues surrounding incompatible ABO transplants | Examine consent informed risk-benefit analysis and resource allocation |
| 24. “The ethics of ABO incompatible kidney transplantation: a position statement of the American Society of Transplantation”Morris A, et al.38 | USA | 2019 | Revision | Analyze ethical aspects of incompatible ABO transplants | Address concerns and promotes ethical practice | Supports ABO transplantation incompatible with due safeguards |
| 25. “Will you give my kidney back? Organ restitution in living related kidney transplantation: ethical analyses”Nakazawa E, et al.39 | Japan | 2020 | Literature review | Analyze the ethical arguments for and in favor of against the return of organs in the Context of kidney transplantation from living donors. | Literature review of articles academics and documents relevant information on the Ethics of organ transplantation. | The authors identified a series of arguments in favor and against the return of organs, and concluded that there is no easy answer to the question of whether it is ethically justifiable. |
| 26. “Kidney exchange strategies: new aspects and applications with a focus on deceased donor-initiated chains”Di Bella, et al.40 | Italy | 2020 | Narrative review | Analyze new strategies of renal exchange, with an emphasis on chains initiated by deceased donors. | Literature review and analysis of approaches novel in renal exchange. | Expands access to kidney transplantation:- Maximizes the number of transplants in a chain.- Inclusion of those with special characteristics.- Regional and national programs. |
| 27. “Paired kidney donation: are we going beyond reasonable limits in living-donor transplantation?”Medina-Pestana J, et al.41 | Brazil | 2020 | Quantitative study | Evaluate the characteristics and outcomes of the Kidney donation in pairs. | Retrospective analysis of 104 cases of kidney donation by couples. | Kidney donation in pairs is a safe alternative and effective in increasing access to kidney transplantation. However, it is Important to select carefully to the couples and provide them with adequate follow-up. |
| 28. “The present and future of transplant organ shortage: some potential remedies”Bastani B, et al.42 | International | 2020 | Theoretical essay | Explore potential solutions for the shortage of organs for transplantation. | Analysis of the literature and theoretical proposals. | The shortage of organs for transplantation is a global problem with serious consequences for public health. Approaches needed innovative ones, such as the Incentive to donate or genetic modification of animal organs, to increase the supply of organs. |
| 29. “Living kidney donation: outcomes, ethics, and uncertainty”Reese PP, et al.43 | Canada | 2020 | Literature review | Summarize the results, ethics, and uncertainty of living kidney donation. | Review of the literature and analysis of the findings. | Living kidney donation is an option viable for transplantation kidney, but it has risks and uncertainties that must be carefully considered. |
| 30. “ABO-incompatible kidney transplantation: where do we stand?”Nadal J, et al.44 | Europe | 2020 | Revision | Assess the current status of incompatible ABO transplantation | Discusses progress and remaining challenges | Highlights progress in techniques and needs research in course |
| 31. “Pre-emptive live donor kidney transplantation-moving barriers to opportunities: An ethical, legal and psychological aspects of organ transplantation view”David van Dellen, et al.5 | United Kingdom | 2021 | Qualitative study | Examination of the factors influencing the access to preventive TRDV | Grouping according to existing constraints | - National frameworks- Society- Individualization- Ease of donor-Possible lack of receptor adhesion |
| 32. “Have we reached the limits in altruistic kidney donation?”Thomas R, et al.45 | United Kingdom | 2021 | Narrative review | To analyze whether the limits of altruistic kidney donation have been reached. | Review of the literature and analysis of trends in altruistic donation. | - Increased demand for kidneys- Difficulty finding compatible donors |
| 33. “Perceptions of psychosocial and ethical issues and the psychological Characteristics of donors in the clinical setting of living kidney donors: a qualitative study”Arai N, et al.46 | Japan | 2021 | Qualitative study | Explore perceptions of living kidney donors on psychosocial and ethical issues. | Semi-structured interviews with 20 living kidney donors. | Donors experienced a variety of emotions, including anxiety, worry, and happiness. Also identified several psychosocial and ethical challenges, such as burden financial and family pressure. |
| 34. “Living donors and the issue of informed consent”Lederer SE, et al.20 | USA | 2021 | Literature review | Analyze the concept of consent reported in the living organ donation. | Literature review and ethical analysis. | Informed consent in the Living organ donation is complex and requires a process to ensure the understanding the risks and benefits. |
| 35. “Emerging ethical challenges in living kidney donation”Guignard VV, et al.11 | Canada | 2021 | Literature review | Examine the new ethical challenges that arise in living kidney donation. | Literature review and ethical analysis. | Living kidney donation presents new ethical challenges related to the marketing, coercion and the use of social networks. |
| 36. “Gender and race/ethnicity differences in living kidney donor demographics: Preference or disparity?”Ross LF, et al.6 | USA | 2021 | Population descriptive study | Analysis of differences demographic, on everything, gender and race in the TRDV | Vulnerability analysis of groups to study, based on Kenneth's work Kipnis | Underrepresentation of Black people as donors, and Overrepresentation of women |
| 37. “Ethical Challenges in Independent Living Donor Advocacy”Vittone SB, et al.47 | USA | 2021 | Qualitative study | Identify in donors:- Obligations- Ethical principles- Ethical challenges | Survey provided via REDcap.Quantitative and qualitative analysis | 34 participants responded.- Non-maleficence, the most common principle for the decision to donate. |
| 38. “Ethical analysis examining the prioritization of living donor transplantation in times of healthcare rationing”Kulkarni S, et al.10 | USA | 2021 | Qualitative study | Analyze the situation of limitations of health resources, to carry out Futures protocols Episodes | Ethical analysis | - TRDV should not be suspended- SARS VOCs 2, Infections should be considered as extra risk- COVID Protocols 19 in transplant hospitals |
| 39. “Controversies in living kidney donation”Winston Wing-Shing Fung, et al.48 | International | 2022 | Population descriptive study | Analysis of concerns and Current ethical controversies in TRDV | Ethical analysis | - Informed consent is simplistic- Arguments for and against the anonymity of the donor.- Validity of the consideration of donors to minors.- Responsibility of the transplant team |
| 40. “Risk assessment and management for Potential Living Kidney donors: The role of “third-party” Commission”Tattoli L, et al.12 | Italy | 2022 | Retrospective observational study | Evaluate the role of a “third-party commission” in the evaluation of living kidney donors and the management of associated risks. | Analysis of 116 medical records Kidney Donations with the intervention of a third-party commission. | - The third-party commission identified potential risks in donors who then were discarded or subjected to additional follow-up.- The intervention of the commission contributed to decision-making informed and voluntary by donors. |
| 41. “Ethical issues in kidney transplant and donation during COVID-19 pandemic”Chow K-M, et al.49 | International | 2022 | Narrative Review | Exploring ethical issues in kidney transplantation and donation during the COVID-19 pandemic. | Review of the literature and analysis of emerging ethical situations. | - Risk of COVID-19 transmission- Prioritization of health resources- Decision to postpone transplants |
| 42. “The Ethics of Living Donation. In: Sharif, A., Lipkin, G. (eds) Living Kidney Donation”Cronin, A.J, et al.50 | United Kingdom | 2022 | Book Chapter | To analyze the ethical issues of living kidney donation. | Analysis of ethics in living kidney donation. | - Living kidney donation poses dilemmas ethical that require continuous analysis. |
| 43. “Deceased donors as nondirected donors in kidney paired donation”Wang W, et al.51 | USA | 2022 | Quantitative study | Assess the feasibility of using donors deceased not directed in renal donation by couples. | Retrospective analysis of 188 deceased donors did not directed in a Program of Kidney donation in pairs. | The use of deceased donors does not Directed in Kidney Donation by Pairs is feasible and safe. It can increase the number of available donors and access to kidney transplantation. |
| 44. “Paired kidney donation: are we going beyond reasonable limits in living-donor transplantation?”Medina-Pestana J, et al.52 | Brazil | 2022 | Population descriptive study | - Comparison of TRV frequencies with deceased donor TR- Reflection on TRDV's ethical dilemmas | Analysis of frequencies of both modalities by TR | Increase in the number of deceased donors in recent years comparison with the live one in Brazil. |
| 45. “Controversies in living kidney donation”Winston Wing-Shing Fung, et al.7 | International | 2022 | Population descriptive study | Analysis of concerns and Current ethical controversies in TRDV | Ethical analysis | -Informed consent is simplistic-Arguments for and against the anonymity of the donor.-Validity of the consideration of donors to minors.-Responsibility of the transplant team- Marketing programs. |
| 46. “Report from a multidisciplinary symposium on the future of living kidney donor transplantation”Peters TG, et al.48 | USA | 2023 | Qualitative study | Approach to the future of kidney transplantation, review of the moral, economic, and regulatory bodies that affect in a way Refusal to patients in the USA | Multidisciplinary study | -There is no increase in TRDV donations, it is necessary to search for strategies to expand the donor pool.They are financial compensation or donor chains |
| 47. “Kidney transplantation during Mass Disasters – From COVID-19 to other catastrophes A Consensus Statement by the DESCARTES Working Group and Ethics Committee of the ERA”Sever MS, et al.9 | Europe | 2023 | Literature review | To make recommendations to be followed in possible mass disasters | Analysis of the COVID 19 pandemic | - Standard ethical principles may not apply, in situations of massive disasters.- Priority to the preservation of the health personnel.- No practical situation to the problem of lack of health care. |
| 48. “Anonymity in kidney paired donation: a systematic review of reasons”Marcus K, et al.15 | Switzerland | 2023 | Systematic review | Evaluate the reasons for and against anonymity in the kidney donation by exchange. | Search Bibliography at databases and analysis of studies. | Reasons for and against anonymity: 24 for and 38 against.- Main reason in favor, protection from damages to both parties.- Against, respect for people's wishes. |
| 49. “Red flags in the living kidney donor process”Lagging E, et al.53 | Sweden | 2023 | Narrative Review | Identify red flags in the process of living kidney donation, using a donor survey. | Literature review and case study analysis. | Several statistically significant risk factors were identified:- More fatigue and pain than expected after the intervention.- Sense of duty.Other:- Expectations different from reality.- Psychosocial concerns. |
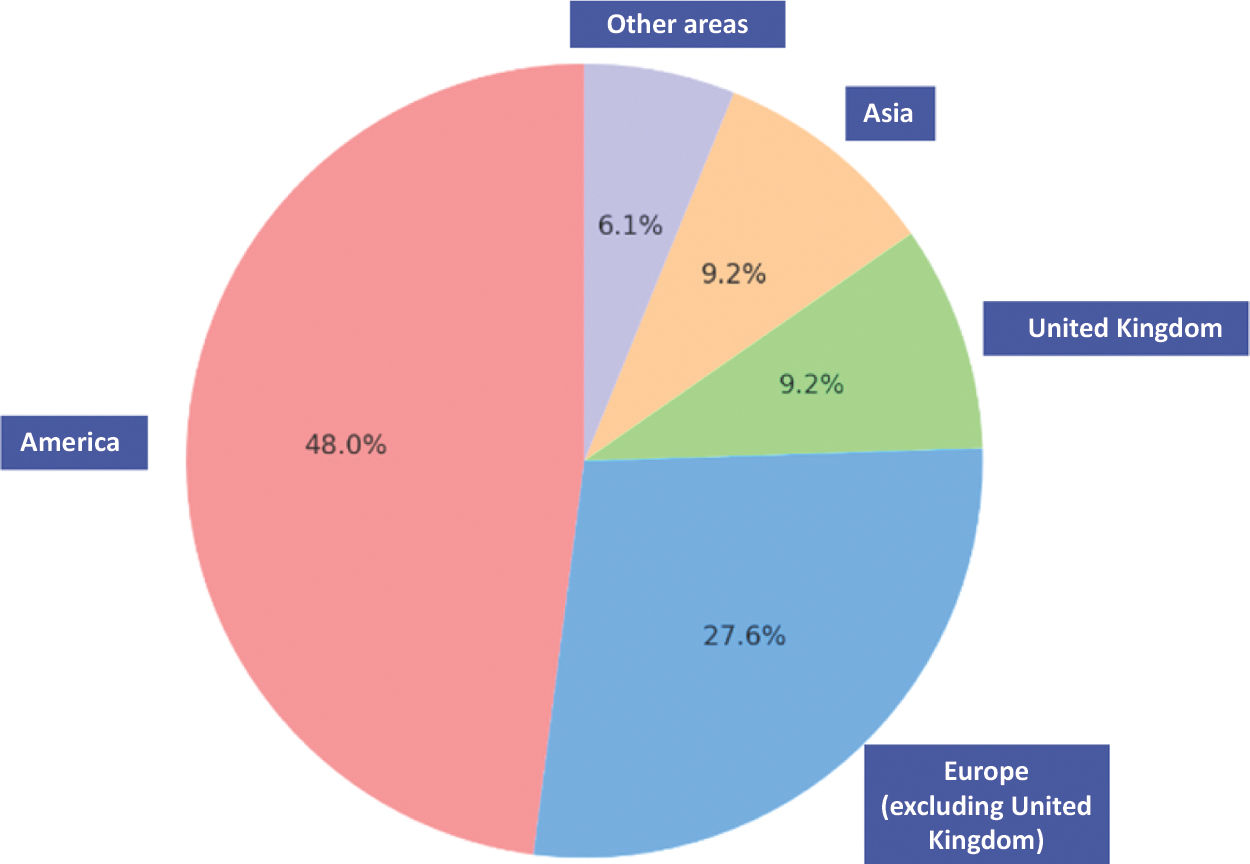
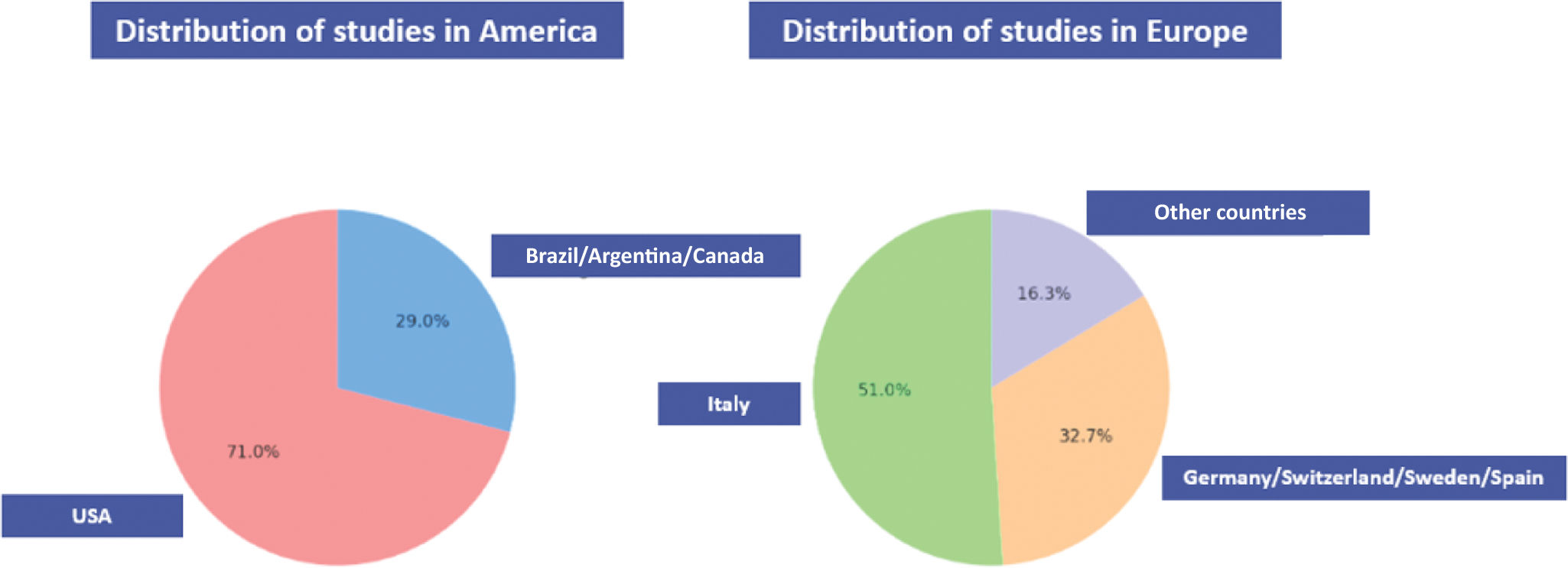
This systematic review included 49 articles that primarily evaluated the ethical aspects of living donor kidney transplantation and some demographic characteristics. Of the studies analyzed, 47% were conducted in the Americas, with 71% of them in the United States and the rest in Brazil, Argentina, and Canada. In Europe, 27% of the studies were conducted, with Italy accounting for 50% of them. Other European countries, such as Germany, Sweden, Switzerland, and Spain, represented 8% each. 9% of the studies were from the United Kingdom and Asia (China, Japan, Pakistan). Additionally, 6% of the studies were conducted in international collaboration (Figs. 2 and 3). The articles highlight the complexity of the ethical dilemmas surrounding of living donor kidney transplantation, emphasizing the need for multidisciplinary approaches and unified protocols to address both current and future challenges. The ethical issues found vary depending on geographic location, study design, and specific objectives. Living donor kidney transplantation poses multiple ethical challenges (Fig. 4). The principle of beneficence requires ensuring that the benefits outweigh the risks, while the principle of non-maleficence mandates minimizing potential harm. Van Dellen D et al. highlight the importance of equity in access to transplants and the individualization of the process to overcome preventive barriers.5 The principle of justice is also frequently addressed, particularly in the allocation of organs. The review shows that, in some countries, there are racial and gender inequalities in donation. Ross LF et al. highlight the underrepresentation of the Black race and the overrepresentation of women as donors, evidencing an equity issue.6
Informed consentThe principle of autonomy, one of the bioethical pillars established by Beauchamp and Childress, is materialized in practice through informed consent. This document must be understandable, accessible, and adapted to the educational level of those involved. In the context of the living donor kidney transplantation, its relevance increases, as it involves both donors and recipients, who are in situations of particular vulnerability. Several studies highlight the need to include emotional, psychological, and motivational aspects in the consent process, beyond surgical and clinical risks. Fung WW-S et al. emphasize the importance of reflecting the donor's emotional concerns, while Hartsock JA et al. underscore the role of consent in preventing human trafficking in countries where the commercialization of organs is allowed.7,8 The studies by Sever MS et al. and Kulkarni S et al. analyze informed consent under disaster conditions, such as the COVID-19 pandemic, where the risk of infection increases, requiring greater understanding from patients and the need for consent to reflect these exceptional circumstances.9,10
Coercion, exploitation, transplant tourism and global equityThe possibility of donor coercion and exploitation is a recurring concern in the literature. The studies by Hartsock JA et al. and Guignard VV et al. examine the commercialization of organs and the need to establish effective controls to prevent exploitation.8,11 The creation of “third-party commissions,” as proposed by Tattoli L et al. allows for the evaluation of potential risks in donors and guarantees informed and pressure-free decisions.12 Transplant tourism, where patients travel to other countries to receive organs, raises important ethical questions. Inequalities in access to organs between rich and poor countries are highlighted by Shekhani SS et al. and Wright L et al. Both studies address the issue of donor exploitation in countries with fewer resources and the inequity in global healthcare.13,14
Anonymity and privacyAnonymity in organ donation is a controversial issue. Marcus K et al. and Fung WW-S et al. highlight the pros and cons of maintaining donor anonymity. On the one hand, it protects privacy and reduces psychological pressure; on the other hand, it is argued that knowing the recipient's identity can increase donor satisfaction.7,15
Desensitization and incompatible blood type (ABO) transplantsIncompatible blood type (ABO) transplants also raise ethical dilemmas, especially regarding informed consent and resource allocation. Cecka M et al. and Sander D et al. highlight the need to adapt the consent process to reflect the additional risks of this procedure.16,17 Lozano-Muñoz J et al. show that although clinical outcomes are similar to those of compatible blood type transplants, the ethical aspects require deeper analysis.18
DiscussionThe review includes proposals to improve ethics in living donor kidney transplantation. Grossi et al. propose a model of informed consent based on three phases: preoperative information, psychosocial evaluation, and final consent.19 Lederer et al. recommend a prior educational process to ensure donors fully understand the risks.20 Perea et al. highlights the need for coordinated ethical management in living kidney donation.21 They propose the collaboration of various healthcare professionals and compliance with strict legal requirements, such as legal age, mental competence, and access to complete and understandable information. This systematic review mainly highlights that the informed consent is the cornerstone of ethics in living donor kidney transplantation, guaranteeing the autonomy, dignity, and respect of patients. The review reveals the need to integrate emotional, social, and psychological aspects into the consent process, in addition to the usual surgical risks. Issues of equity, anonymity, exploitation, and transplant tourism also stand out as significant ethical challenges. In general, the findings of this review underscore the need to develop robust ethical frameworks to address emerging issues in living donor kidney transplantation, promoting fair, equitable practices centered on respect for the autonomy of both the donor and the recipient.22 Living donor kidney transplantation has emerged as a crucial therapeutic option for patients with end-stage renal disease. Results show that there is a largest proportion of living-donor transplants originate in chronic kidney disease units, rather than in dialysis units. This could be due to the fact that patients managed in this stage, are more likely to be referred the living-donor transplant option than those in dialysis unit. Patients in dialysis units, often experience delays in referral for transplantation, so they accumulate more comorbidities and are less likely to identify a living donor option.
Despite its clear benefits for recipients, the ethical complexity of this procedure should not be overlooked. This systematic review of 49 studies explores the various ethical dilemmas associated with living donor kidney transplantation, offering a broad perspective on the issues involving both donors and recipients.
The review shows a strong geographic concentration of studies in the United States and Europe, reflecting greater development and access to living donor kidney transplantation programs in these regions, as well as growing interest in its ethical analysis. Most studies were published between 2019 and 2023, indicating recent dynamism in research on this topic. The significant disparity in the rate of living-donor kidney transplants worldwide, particularly the difference between Spain and other countries, may be attributed to multiple factors. Among these, Spain's strong emphasis on deceased-donor kidney transplantation plays a central role, along with strict policies aimed at preventing issues such as coercion or commercialization in living-donor transplants. Additionally, the country has a highly coordinated deceased-donor transplant system, while there is a notable lack of information and promotion regarding living-donor kidney transplantation.54,55 We propose some strategies to increase the rate of living-donor kidney transplants in accordance with current legal and ethical regulations (Table 2).
Strategies to increase living-donor kidney transplant.
| Strategy to increase the rate of living-donor kidney transplant | Description |
|---|---|
| 1. Public education programs and awareness campaigns. | Increase awareness and knowledge about living donation, avoiding undue pressure and providing understandable information. |
| 2. Strengthening informed consent. | Clearer, more understandable protocols adapted to each donor's reality. |
| 3. Independent psychosocial counseling. | External evaluations to verify the donor's voluntariness and readiness, aiming to prevent coercion and exploitation. |
| 4. Promoting equity in access. | Identification and elimination of demographic or structural barriers. |
| 5. Continuous bioethics training for professionals. | Mandatory training on ethical dilemmas to improve the quality of clinical and ethical decision-making. |
| 6. Creation of adaptable ethical frameworks. | Flexible regulations that are updated in line with medical and social advances, as well as proposals to respond to crises and adapt to new technologies. |
| 7. Interdisciplinary collaboration. | Joint work between physicians, bioethicists, lawyers, and civil society. |
| 8. Promotion of ethical and empirical research. | Funding studies on the ethical implications of LDKT that explore emerging dilemmas such as desensitization. |
Moreover, the need for expanding the ethical analysis is highlighted, as recent advancements, such as ABO incompatible desensitization, generate new dilemmas that require more attention. The included methodological studies cover a wide range, from case analyses to quantitative and qualitative studies, enriching the understanding of the ethical aspects of living donor kidney transplantation. The most recurrent ethical dilemmas identified in the review include issues of beneficence and non-maleficence, where the risks and benefits for both donors and recipients are evaluated. A central issue is the nephrectomy performed on a healthy donor, which involves additional risks, but also emotional and psychological benefits for both the donor and the recipient, who receives a renal therapy that improves their quality of life. Another relevant dilemma is equity in access to living donor kidney transplantation, as demographic disparities in race, gender, and geographic location are observed. This highlights the need for a fair and non-discriminatory distribution of organs. In this regard, advanced age is often a reason for excluding patients from living-donor kidney transplantation, despite the lack of clinical guidelines supporting such exclusion. While doctors may offer alternative treatments, this reflects a persistent problem of misinformation. Importantly, using age alone as an exclusion criterion is neither clinically nor ethically justified. Both the European Renal Association-European Dialysis and Transplant Association (ERA-EDTA) and the National Kidney Foundation Kidney Disease Outcomes Quality Initiative (KDOQI) state that older recipients can gain significant survival and quality-of-life benefits from transplantation—especially from living donors—even when the donor is also older. Patient and donor autonomy must be respected, highlighting the need for thorough, unbiased informed consent that includes all options and their respective risks and benefits. In conclusion, decisions should be based on individual assessment, not age alone.
Regarding anonymity and confidentiality, the balance between protecting the donor's privacy and ensuring transparency and preventing coercion is emphasized.56 Informed consent is one of the key ethical pillars in living donor kidney transplantation, and the review notes that, due to the inherent risks of organ donation, it is crucial for donors to fully understand the potential risks and benefits of the process. Furthermore, concerns about organ commercialization and coercion are addressed, highlighting the need to prevent the exploitation of vulnerable donors. The global crisis of the COVID-19 pandemic is also discussed in the studies, emphasizing the importance of maintaining solid ethical principles during extreme situations. Additionally, innovations in donation strategies, such as kidney exchange and ABO incompatible desensitization, which expand transplant options, are explored but also pose dilemmas regarding equity and associated risks. From a Spanish perspective, an article reviewed emphasizes the need for ethical and coordinated management of living donor kidney transplantation, highlighting the importance of informed consent and minimizing risks for donors. The review also emphasizes the need for continuous ethical training to address the challenges posed by living donor kidney transplantation. This review reflects on the importance of having adaptable ethical frameworks that can address emerging dilemmas, encourage public dialog, and promote interdisciplinary collaboration. The findings of this review largely align with the existing literature, but contribute a systematic and updated vision of living donor kidney transplantation ethics, providing a foundation for future research and more ethical and equitable practices.
ConclusionsWe need robust and adaptable ethical frameworks that can address new challenges and emerging technologies, as well as global crises, ensuring responsible ethical decision-making, highlighting the importance of ethical education, promoting dialog about living donor kidney transplants. This is crucial to increase understanding and enable informed decisions by donors, recipients, and healthcare professionals, while promoting fair and equitable practices. Moreover, we need interdisciplinary collaboration since a joint effort is required between healthcare professionals, bioethicists, philosophers, lawyers, and representatives of civil society to comprehensively evaluate ethical dilemmas and develop effective solutions. Due to complexity of the ethical landscape, living donor kidney transplant presents a wide range of ethical dilemmas, such as beneficence, non-maleficence, equity, anonymity, informed consent, and organ commercialization, all of which must be carefully considered in each case. Thus, it is crucial to ensure that access to living donor kidney transplants is fair and equitable, without discrimination based on race, gender, or geographical location, and to promote a transparent, non-discriminatory system. This review wants to give a continuous and reflective ethical approach which is needed to address new dilemmas and ensure that practices remain aligned with ethical principles as the practice of living donor kidney transplantation evolves.
Authors’ contributionsIRM: Conceptualization, bibliographic analysis, results and discussion.
JLC: Methodological design and discussion.
FundingThis systematic review did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestNone declared.